Hypoplastic Dysplasia of Kidney with Hydroureter: Two Cases
Sarojini Raman1, Sukant Kumar Padhy2, Jayasree Rath3, Urmila Senapati4
1 Associate Professor, Department of Pathology, KIMS, Bhubaneswar, Odisha, India.
2 Assistant Professor, Department of Urology, KIMS, PBMH, Bhubaneswar, Odisha, India.
3 Professor, Department of Pathology, KIMS, Bhubaneswar, Odisha, India.
4 Professor and Head, Department of Pathology, KIMS, Bhubaneswar, Odisha, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sarojini Raman, Associate Professor, Department of Pathology, KIMS, Campus-5, Bhubaneswar-751024, Odisha, India.
E-mail: sarojini.raman@kims.ac.in
Various congenital anomalies of the kidney and urinary tract cause significant morbidity and mortality in children. Renal agenesis, hypoplasia and dysplasia belong to this group of abnormalities. The exact aetiology is still unknown. Imaging modalities like Ultrasonography (USG), Dimercaptosuccinic Acid (DMSA) Radionuclide Scan, Diethylene Triamine Pentaacetic Acid (DTPA) scan and Mercaptoacetyletriglycine (MAG3) scan are useful for assessing the relative functional status, degree of blood flow and any possible obstruction to the kidneys particularly in very young children and in patients with poor kidney function. Management is determined by the severity of cases. We report two cases of hypoplastic dysplasia of kidney, in which one case remained undetected till adulthood. Grossly the affected kidneys were small in size with dilated ureters. Histopathological study showed primitive ducts surrounded by immature mesenchymal tissue representing dysplasia. Radiological and histopathological examination remains the mainstay in diagnosis of such cases.
Hypoplasia kidney, Multicystic dysplastic kidney, Ultrasonography
Case Report
Case 1
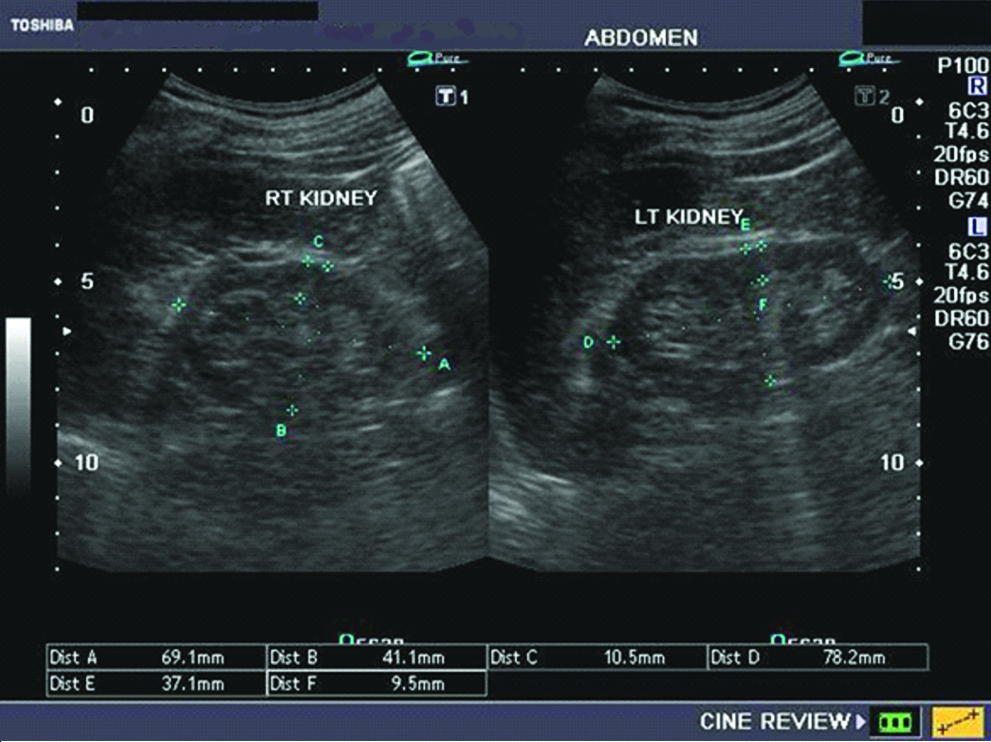
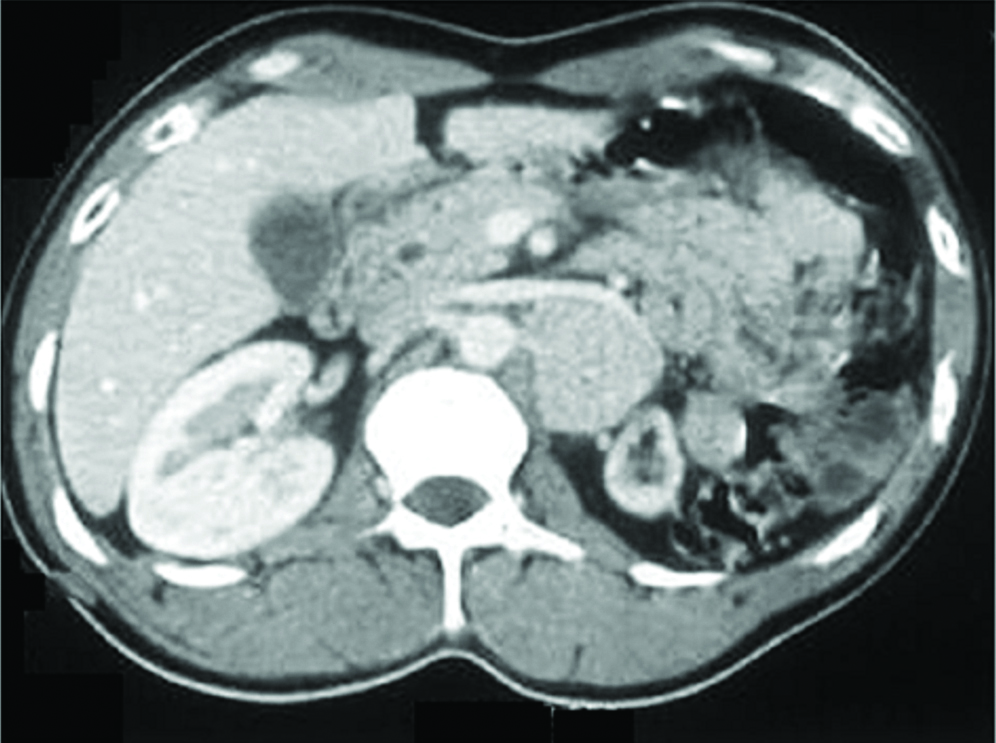
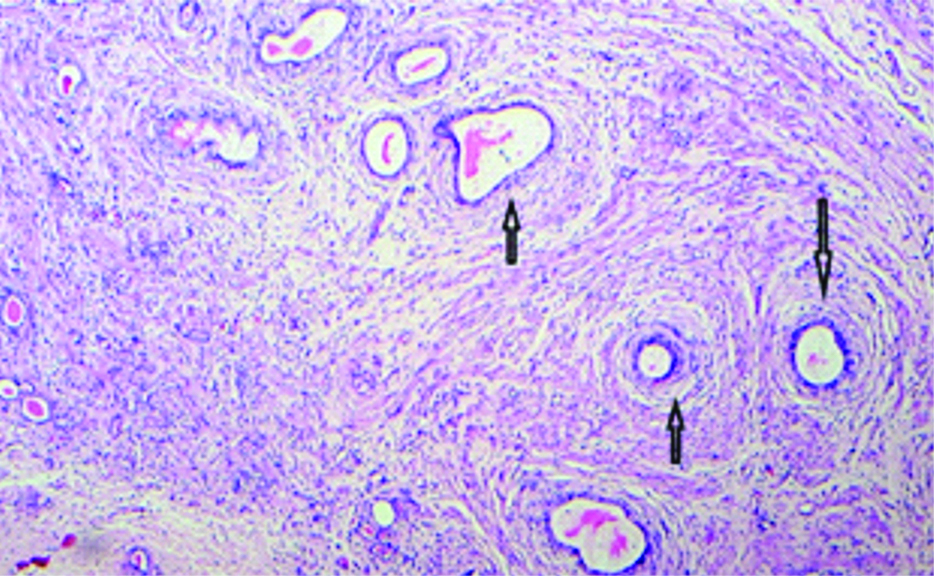
A 20-year-old pregnant female came for routine antenatal checkup with complain of mild pain in left flank. On examination her blood pressure was normal with no other systemic abnormalities. Further investigations revealed: Blood urea-18 mg/dL, Sr creatinine-0.7 mg/dL, Urine RE/ME: Albumin-nil, Pus cells-nil, Epithelial cells-0-2/hpf. USG Abdomen and pelvis showed small sized left kidney with mild hydronephrosis and dilated ureter. Right kidney showed compensatory hypertrophy [Table/Fig-1]. X-ray IVU revealed non excretion of contrast from left kidney [Table/Fig-2]. CECT KUB/CT IVU showed small sized left kidney with no excretion of contrast from left kidney [Table/Fig-3]. So, clinical diagnosis was Left nonfunctioning kidney with reflux nephropathy with three diagnostic possibilities: (1) Atrophic kidney due to chronic pyelonephritis and hydronephrosis, (2) Hypoplastic dysplasia with hydronephrosis and (3) Renal segmental hypoplasia or Ask-upmark kidney. Her pregnancy was uneventful. Two years later she underwent left nephrectomy with ureterectomy. Grossly the specimen was a small sized kidney which measured 4×2×2 cm with thin cortex. Attached ureter was 20 cm long with distal cut end diameter 0.2 cm. Ureter was dilated proximally with internal diameter 0.5 cm [Table/Fig-4]. Histology sections showed normal glomeruli and tubules adjacent to areas containing entrapped immature tubules with surrounding smooth muscle cuffing. Focal nerve bundles, cartilage and thick walled blood vessels were also present [Table/Fig-5,6 and 7]. Ureter sections showed thin urothelium and dilated lumina. Histopathological diagnosis was Hypoplastic dysplasia of left kidney with hydroureter. Postoperative course has been uneventful for patient.
USG Abdomen and pelvis showing a small sized left kidney with mild hydronephrosis, dilated ureter. Right kidney had compensatory hypertrophy.
X-ray IVU showing non excretion of contrast from left kidney.

CECT KUB/CT IVU: Small sized left kidney. No excretion of contrast from left kidney.
Gross-left nephrectomy specimen measuring 4×2×2 cm with attached dilated ureter 20 cm long.
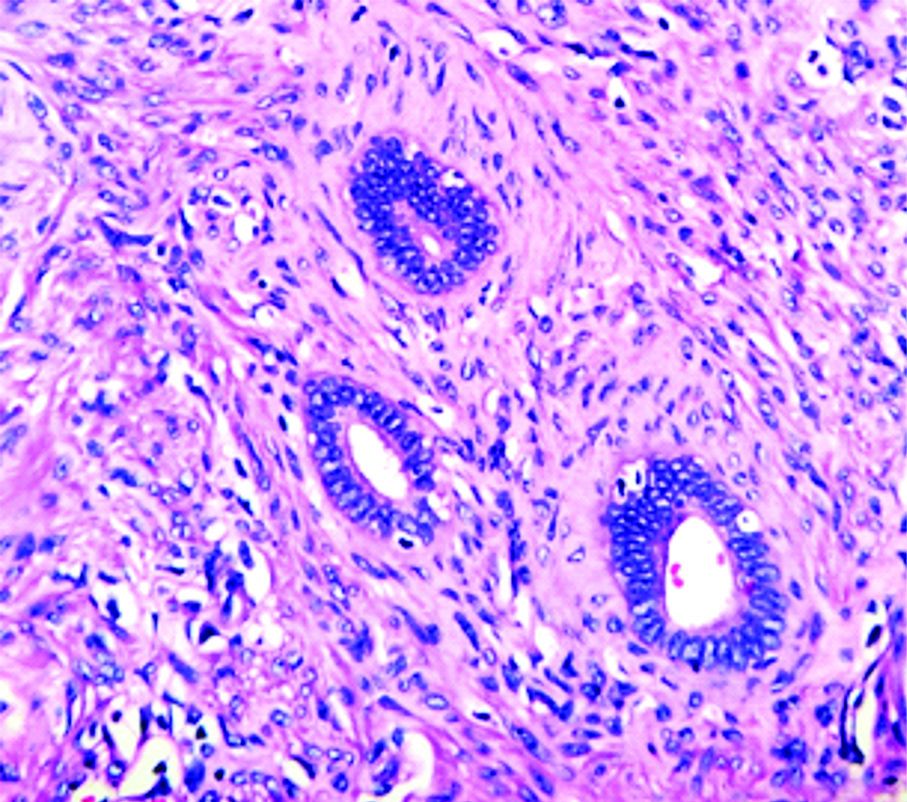
Photomicrograph showing ducts with surrounding smooth muscle cuffing (Arrow marked), H&E stain, 40x.
Ducts lined by cuboidal epithelium and surrounding smooth muscle, H&E stain, 400x.
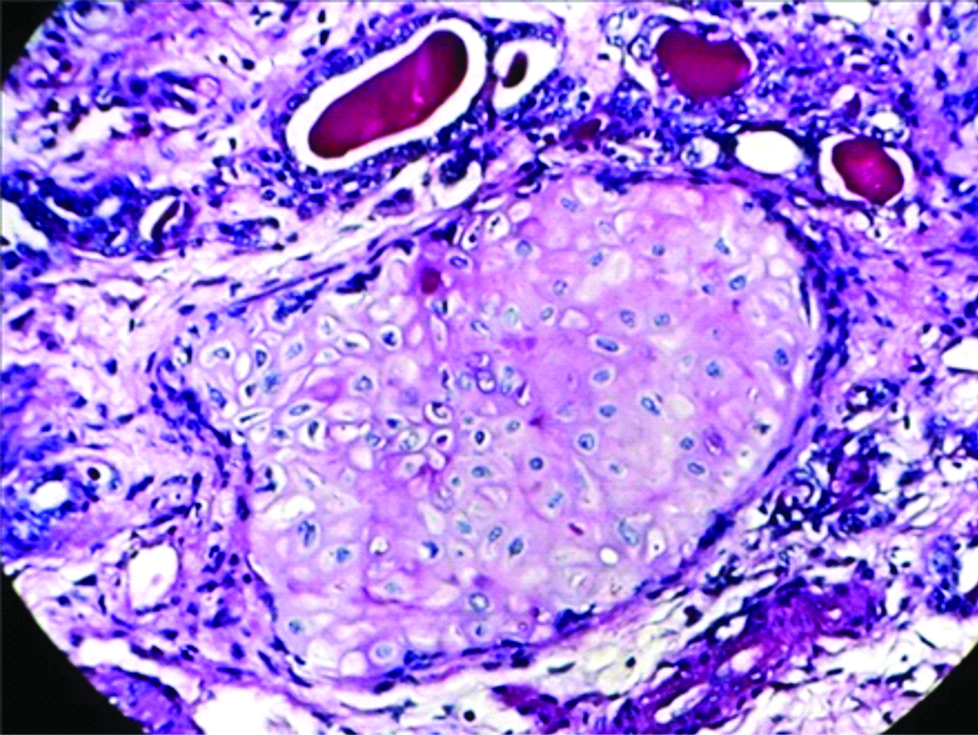
Photomicrograph showing cartilage tissue, PAS stain, 400X.
Case 2
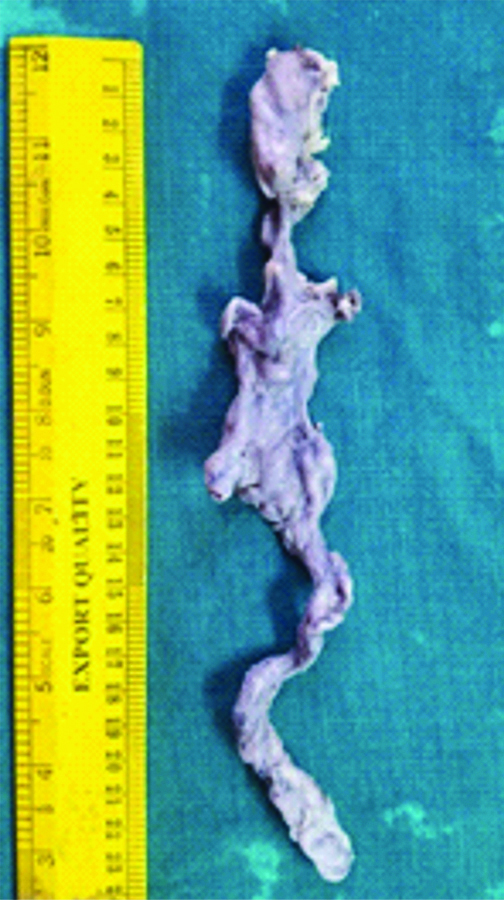
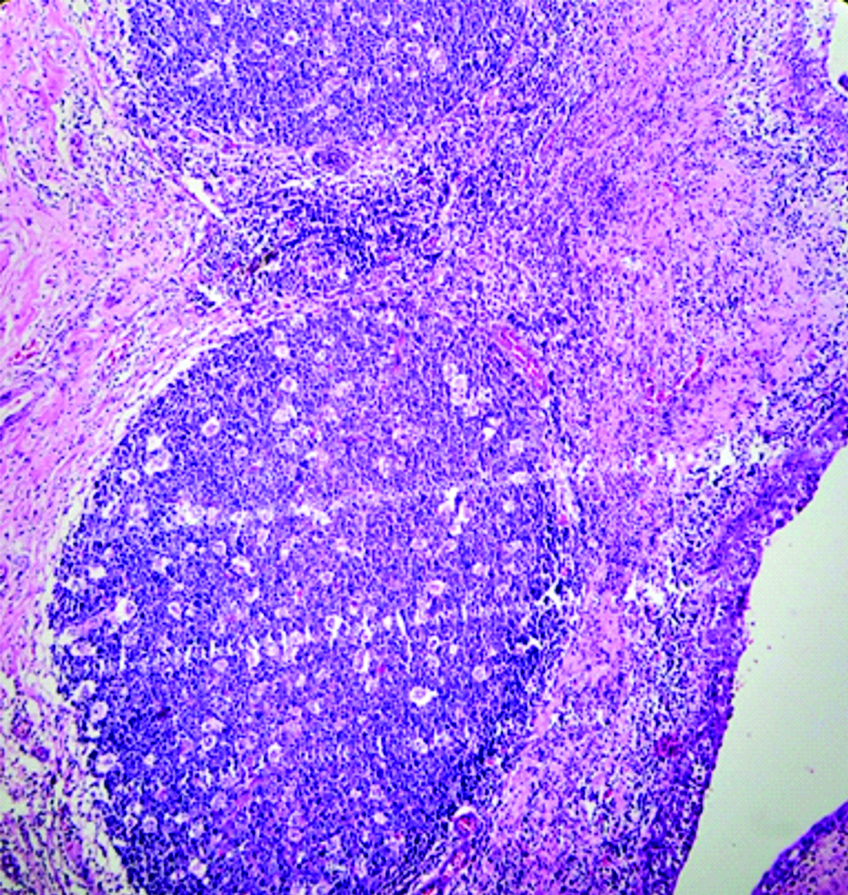
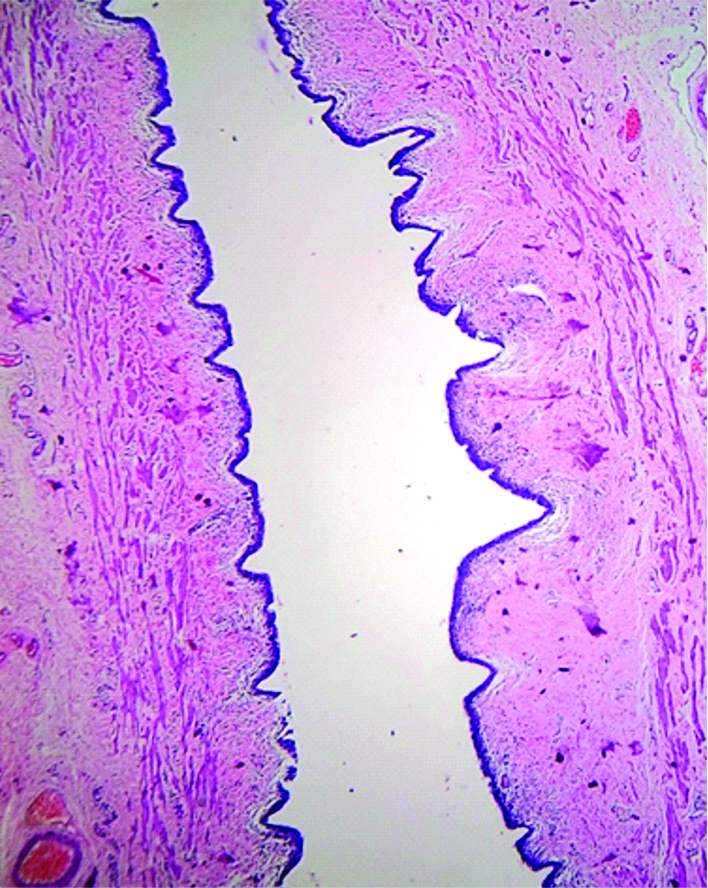
A two-year-old female child came to pediatric surgery OPD with haematuria. Investigations showed Hb-12.35 gm/dL, TLC-12160/cmm, TPC-2.93 lac/cmm, PT-11 sec, INR-0.94, CRP-9.74 mg/dL, Sr Urea-28 mg/dL, Sr Creatinine-0.3 mg/dL, Sr Albumin-5.3 gm/dL, Sr Calcium-10.3 mg/dL, Sr Phosphorus-4.9 mg/dL, Urine C/S showed Escherichia coli growth. So, antibiotic therapy was started. Ultrasonography of abdomen and pelvis showed the right kidney measuring 2.3 cm in length with a thin cortex and dilated right ureter. The left kidney had features of compensatory hypertrophy. Micturating cystourethrogram showed grade 2 right vesicoureteral reflux. DMSA scan showed a non-functioning right kidney with a normal left kidney function, a 98% split function. With the above scan results provisional clinical diagnosis was right poorly functioning kidney with hydroureteronephrosis with ectopic insertions. The differentials were hypoplastic dysplasia with hydronephrosis and Ask-upmark kidney. Patient underwent right nephrectomy. Gross specimen received in pathology department was a small sized right kidney measuring 2.3×1.5×1.2 cm. Ureter was dilated and tortuous measuring 10 cm long [Table/Fig-8]. Distinction between cortex and medulla was ill defined. Salient histological findings included areas of normal appearing glomeruli and tubules adjacent to areas containing fetal glomeruli and immature tubules which were surrounded by chronic inflammation and fibrosis [Table/Fig-9,10]. Concentric areas of immature mesenchyme seen around primitive appearing tubules lined by cuboidal to flattened epithelium with small foci of calcification at places. Mixed inflammatory cells and secondary lymphoid follicles seen underneath urothelium [Table/Fig-11]. Ureteric lining was thinned at places and infiltrated with inflammatory cells [Table/Fig-12]. Diagnosis was Hypoplastic dysplasia of kidney with hydroureter and associated reflux nephropathy.
Gross-Small right kidney measuring 2.3×1.5×1.2 cm with dilated tortuous ureter 10 cm long.

Areas of immature mesenchyme adjacent to normal appearing tubules and glomeruli, H&E stain, 100x.
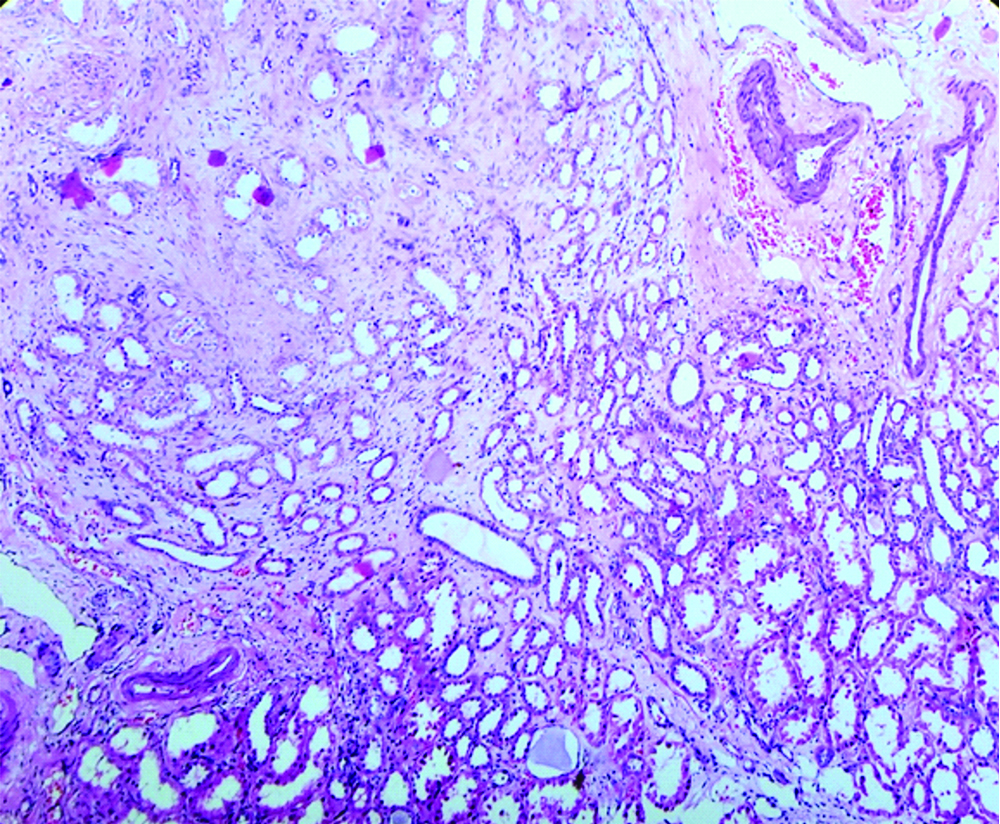
Immature and sclerosed glomeruli, H&E stain, 100x.
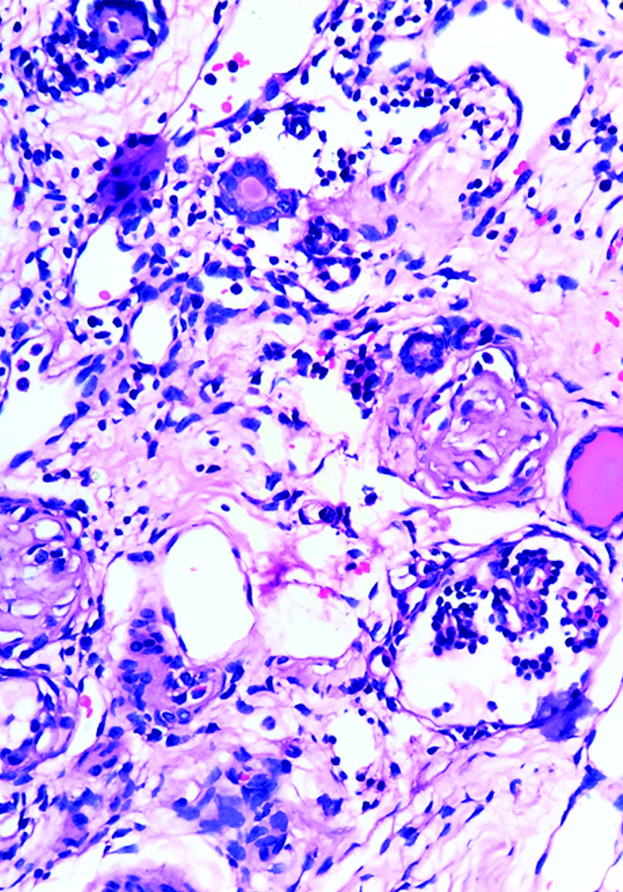
Germinal centre and chronic inflammation underneath urotheliual lining, H&E stain, 100x.
Dilated ureter, thinned urothelium, H&E stain, 100x.
Discussion
Renal hypoplasia, dysplasia and agenesis are considered as heterogeneous disorders, coming under group of Congenital Anomalies of the Kidney and Urinary Tract (CAKUT) [1]. Incidence is reported to be one in 3640-4300 live births; though most often sporadic, familial cases do occur [2]. It may be associated with cysts as in Multicystic Dysplastic Kidney (MCDK), reflux nephropathies, Ureteral /urethral atresia, Uretero-Pelvic Junction (UPJ) obstruction, Uretero-Vesicular Junction (UVJ) obstruction, Mega-ureter, Posterior urethral valves and Anterior urethral diverticulum [3-5].
Upper urinary tract (glomeruli and tubules) is derived from the Metanephric Mesenchyme (MM), and the lower urinary tract (collecting duct, renal pelvis, ureter) develops from the ureteric bud [6]. Diagnostic criteria of primary renal hypoplasia is: (a) A reduction of renal size by 2 standard deviations (SDS) from the mean size for age; (b) Exclusion of renal scarring due to secondary causes by DMSA scan; and (c) Presence of compensatory hypertrophy of the contralateral kidney. Vesicoureteral Reflux (VUR) and/or Ureteropelvic Junction Obstruction (UPJO) are frequently associated with renal hypoplasia. Presence of renal cysts should be detected by USG as primary renal hypoplasia may be associated with fibrosis and cysts, as in nephronophthisis. The various types of hypoplasia are oligonephric hypoplasia, congenital oligonephropathy, unirenicular/unipapillary hypoplasia and simple renal hypoplasia [7,8].
Dysplastic kidneys result from failed coordination between developing metanephros and the branching ureteric bud. It contains primitive ducts, considered to be ‘frustrated’ branches of the ureteric bud, surrounded by sheaths of undifferentiated mesenchymal cells [1,9,10]. Renal dysplasia may be associated with variable number of cysts and urinary tract obstruction. Though mostly unilateral, it may be bilateral which is incompatible with life. It is important to distinguish cystic dysplastic kidney disease from autosomal recessive or dominant polycystic kidney disease for prognosis and counselling [11]. The severity and type of renal dysplasia is affected by the pattern of malformation and degree of urinary tract obstruction. Based on this, renal dysplasia has been broadly subdivided into four groups. Group I: classical MCDK resulting from ureteral atresia at pelviureteric junction, Group II: focal and segmental cystic renal dysplasia due to obstruction related to ectopic uretrocele with ureteral duplication, Group III: cystic renal dysplasia associated with lower urinary tract obstruction e.g., posterior urethral valves and Group IV: renal dysplasia without any obstructive uropathy.
Regarding aetiopathogenesis, several hypotheses are proposed like abnormalities of reciprocal induction between the ureteric bud and metanephric blastema, obstruction of urinary tract during nephrogenesis, in-utero viral infections and antiepileptic medications [8]. Clinical course of these cases may vary. Hiraoka M et al., have reported that non-cystic dysplastic kidneys can involute. So, many patients diagnosed in later childhood or adulthood as having ‘unilateral renal agenesis’ may actually have regressed dysplastic kidneys, rather than renal agenesis [12,13]. Many cases present with renal failure due to repeated ascending infections and VUR causing pyelonephritis and secondary nephrolithiasis. Hypertension and malignancies like wilms’ tumour, renal cell carcinoma and urothelial carcinoma has also been reported in dysplastic kidneys. Hypertension is considered to be due to abnormal renin secretion. Nephrectomy of the affected kidney normalises the blood pressure [14].
Hypoplastic dysplasia of kidney can be similar clinically, radiologically and histologically with chronic pyelonephritis associated with obstructive nepthropathy and renal segmental hypoplasia or Ask-upmark kidney. Though chronic pyelonephritis associated reflux nephropathy may present with small atrophic kidney and hydroureter like hypoplastic dysplasia cases; the typical history of repeated ascending infection in urinary tract, radiological evidence of obstruction, i.e., mostly stones and no histological features of dysplasia or chronic infection helps in ruling out this possibility. Similarly in ask-upmark kidney, patients present with hypertension which subsides after nephrectomy and show segmental hypoplasia of kidney with atretic ureter. Both the patients in the study were normotensive, lacked history of recurrent infections, their kidneys were shrunken at both poles with dilated ureters, histological study revealed presence of dysplasia in both cases and metaplastic cartilage in one case with minimal features of chronic inflammation. So the differentials could be ruled out easily.
Literature search in the PubMed database was performed using the MESH terms multicystic dysplastic kidney, hypoplasia kidney [Table/Fig-13]. Three hundred ninety five manuscripts described patients with hypoplastic dysplasia in kidneys with other urogenital anomalies [Table/Fig-14] [15-21].
Search of literature conducted on 26th April, 2019 for case reports and papers on Hypoplastic dysplasia of kidney.
| Database | Search strategies | Case reports found | Number of papers related |
|---|
| MEDLINE (Via PubMed) | Hypoplasia kidney (Mesh), Multicystic dysplastic kidney (Mesh), case report (Mesh) | 124 | 395 |
PubMed-indexed papers in English reporting on hypoplastic dysplasia of kidney (MESH terms used: multicystic dysplastic kidney, hypoplasia kidney) [15-21].
| Author and year | Number of patients |
|---|
| Scala C et al., 2017 [15] | 144 |
| Sharda S et al., 2014 [16] | 34 |
| Dogan CS et al., 2014 [17] | 59 |
| Moralioglu S et al., 2014 [18] | 68 |
| Schreuder MF et al., 2009 [19] | 3500 |
| Narchi H, 2005 [20] | 26 |
| Feldenberg LR et al., 2000 [21] | 35 |
Conclusion
Renal functions in children with hypoplastic dysplastic kidney depend on the status of contralateral functioning kidney; so long term nephrological follow-up is needed. These abnormalities should be detected early for proper management.
[1]. Winyard P, Feather S, Genetics of human kidney malformationsNephrol Dial Transplant 1996 11:976-78.10.1093/ndt/11.6.9768671954 [Google Scholar] [CrossRef] [PubMed]
[2]. Rukmangadha N, Chowhan AK, Patnayak R, Radhika K, Phaneendra BV, Lakshmi AY, Multicystic dysplastic kidney: A retrospective study with clinicopathological correlationJournal of Clinical Science Research 2013 2:88-93.10.15380/2277-5706.JCSR.12.045 [Google Scholar] [CrossRef]
[3]. Debnath J, Singh H, Kapur K, Bhattacharya TK, Multicystic dysplastic kidneys: Antenatal diagnosisMJAFI 2004 60:310-11.10.1016/S0377-1237(04)80076-5 [Google Scholar] [CrossRef]
[4]. Aytac B, Şehİtoğlu I, Vuruska H, Multicystic dysplastic kidney: Four-year evaluationTurk Patoloji Derg 2011 27(3):210-14.10.5146/tjpath.2011.0107721935870 [Google Scholar] [CrossRef] [PubMed]
[5]. Ylinen E, Ahonen S, Ala-Houhala M, Wikstrom S, Nephrectomy for multicystic dysplastic kidney: if and when?Urology 2004 63:768-71.10.1016/j.urology.2003.11.05315072898 [Google Scholar] [CrossRef] [PubMed]
[6]. Susan EI, McHugh KM. Congenital Obstructive Nephropathy: Clinical Perspectives and Animal Models, Novel Insights on Chronic Kidney Disease, Acute Kidney Injury and Polycystic Kidney Disease, Dr. Soundarapandian Vijayakumar (Ed.), ISBN: 978-953-51-0234-32 [Google Scholar]
[7]. Sanna-Cherchi S, Caridi G, Weng P, Scolari F, Genetic approaches to human renal agenesis/hypoplasia and dysplasiaPediatr Nephrol 2007 22:1675-84.10.1007/s00467-007-0479-117437132 [Google Scholar] [CrossRef] [PubMed]
[8]. Boissonnat P, What to call hypoplastic kidney?Arch Dis Child 1962 37:142-48.10.1136/adc.37.192.14213870698 [Google Scholar] [CrossRef] [PubMed]
[9]. Woolf AS, Unilateral multicystic dysplastic kidneyKidney Int 2006 69:190-93.10.1038/sj.ki.500001516374443 [Google Scholar] [CrossRef] [PubMed]
[10]. Nagata M, Shibata S, Shu Y, Pathogenesis of dysplastic kidney associated with urinary tract obstruction in uteroNephrol Dial Transplant 2002 17:37-38.10.1093/ndt/17.suppl_9.3712386283 [Google Scholar] [CrossRef] [PubMed]
[11]. Al-Khaldi N, Watson AR, Zuccollo J, Twining P, Rose DH, Outcome of antenatally detected cystic dysplastic kidney diseaseArch Dis Child 1994 70:520-22.10.1136/adc.70.6.5208048824 [Google Scholar] [CrossRef] [PubMed]
[12]. Nepple K, Cooper CS, Multicystic dysplastic kidneyPediatric Urology For Primary Care Physician, Current Clinical Urology 2014 19:11-16.10.1007/978-1-60327-243-8_2 [Google Scholar] [CrossRef]
[13]. Sugimoto T, Tanaka Y, Nitta N, Uzu T, Nishio Y, Kashiwagi A, Renal segmental hypoplasia, Ask-Upmark kidney, in a patient with adult-onset hypertensionIntern Med 2006 45(19):1101-02.10.2169/internalmedicine.45.185817077574 [Google Scholar] [CrossRef] [PubMed]
[14]. Hiraoka M, Tsukahara H, Ohshima Y, Kasuga K, Ishihara Y, Mayumi M, Renal aplasia is the predominant cause of congenital solitary kidneysKidney Int 2002 61:1840-44.10.1046/j.1523-1755.2002.00322.x11967035 [Google Scholar] [CrossRef] [PubMed]
[15]. Scala C, McDonnell S, Murphy F, Leone Roberti Maggiore U, Khalil A, Bhide A, Diagnostic accuracy of mid-trimester antenatal ultrasound for multicystic dysplastic kidneysUltrasound Obstet Gynecol 2017 50(4):464-69.10.1002/uog.1730527643400 [Google Scholar] [CrossRef] [PubMed]
[16]. Sharada S, Vijayakumar M, Nageswaran P, Ekambaram S, Udani A, Multicystic dysplastic kidney: a retrospective studyIndian Pediatr 2014 51(8):641-43.10.1007/s13312-014-0467-z [Google Scholar] [CrossRef]
[17]. Doğan ÇS, Torun-Bayram M, Aybar MD, Unilateral multicystic dysplastic kidney in childrenTurk J Pediatr 2014 56(1):75-79. [Google Scholar]
[18]. Moralıoğlu SS, Cerrah-Celayir A, Bosnalı O, Zeki-Pekta ş O, Kaplan-Bulut I, Single center experience in patients with unilateral multicystic dysplastic kidneyJ Pediatr Urol 2014 10(4):763-68.10.1016/j.jpurol.2014.03.00824873872 [Google Scholar] [CrossRef] [PubMed]
[19]. Schreuder MF, Westland R, van Wijk JAE, Unilateral multicystic dysplastic kidney: a meta-analysis of observational studies on the incidence, associated urinary tract malformations and the contralateral kidneyNephrol Dial Transplant 2009 24(6):1810-18.10.1093/ndt/gfn77719171687 [Google Scholar] [CrossRef] [PubMed]
[20]. Narchi H, Risk of hypertension with multicystic kidney disease: a systematic reviewArch Dis Child 2005 90(9):921-24.10.1136/adc.2005.07533315871982 [Google Scholar] [CrossRef] [PubMed]
[21]. Feldenberg LR, Siegel NJ, Clinical course and outcome for children with multicystic dysplastic kidneysPediatr Nephrol 2000 14(12):1098-101.10.1007/s00467000039111045394 [Google Scholar] [CrossRef] [PubMed]