Introduction
Soil Transmitted Helminth (STH) infections affect some of the poorest countries in the world. India is one of the most severely affected countries by these parasitic infections. They primarily affect children by impairing nutritional status, cognitive ability and overall development. Lower haemoglobin levels are a very common symptom associated with Helminth infections.
Aim
The present study was conducted to analyse the effect of STH infections on haemoglobin levels in India.
Materials and Methods
A systematic search of PubMed and Web of Science was carried out. We systematically reviewed the literature to identify studies reporting data on STH infection associated anaemia without any bar on language or date of publication. Full text studies reporting data on STH infection associated anaemia in humans were considered for final analysis.
Results
Careful screening resulted in 16 publications that met the eligibility criteria out of which six were case reports and ten were cross-sectional studies that reported data on helminth infections and haemoglobin levels. Odds ratio analysis of five cross-sectional reports indicated that Helminth infections are three times (OR-2.8, CI-95%, 2.4-3.4) more likely to be associated with lower haemoglobin levels as compared to uninfected population. An analysis of case reports indicated severe to moderate anaemia in all patients.
Conclusion
Helminth infections are often associated with lower haemoglobin levels resulting in lower cognitive development. We have found evidence that helminth infections are associated with lower haemoglobin levels in Indian population.
Implications of Key Findings
This study can provide a guideline to clinicians and healthcare professional in identifying a baseline for haemoglobin level associated with STH infection associated anaemia and might lead to more comprehensive analysis of reasons for anaemia, growth stunting and cognitive impairment in at risk Indian population.
Introduction
Soil Transmitted Helminth (STH) infections affect nearly 2 billion people across the world. Most of these infection are reported in children. WHO estimate puts nearly 870 million children under high-risk zones [1]. Most intense Infection has been observed in children aged 5-15 years possibly due to differential exposure to contaminated soil, lack of sanitation and an immature acquired immune response [2]. The prevalence pattern indicates that maximum cases are reported from South America, Africa and Asia [3-5]. India is the one of the largest contributor of STH infection cases with nearly 220.7 million children in need of preventive chemotherapy [6]. These infections are caused by four different species of helminths, Ascaris lumbricoides (roundworm), Trichuris trichiura (whipworm), Ancylostoma duodenale and Necator americanus (hookworm) [3]. The parasite eggs survive in warm and moist climate of tropical countries where they are deposited in soil and can infect via feco-oral transmission in case of roundworm and whipworm and by penetrating the skin of feet in case of hookworm. Prevalence of these infections is often associated with lower socio-economic status, lack of personal and community hygiene, open defecation practices and poor maternal education [7,8]. Consistent infections with any of the three parasites can lead to impaired nutritional status, school performance and irreversible cognitive deficits in the long run [9]. These infections can be treated by a single dose of either Mebendazole or Albendazole and policy makers in India have targeted the school going population by massive deworming programs [10]. WHO recommends annual deworming for areas with higher that 20% prevalence and biannual deworming for areas with higher than 50% prevalence [11]. STH infections are also associated with iron deficiency anaemia with infected individuals reporting lower haemoglobin levels as compared to uninfected individuals [12]. Hookworm infections are particularly of concern as they cause damage to the mucosa of small intestine causing 0.3-0.5 mL of blood loss every day [13]. Initial symptoms at the site of skin penetration appear as pruritic erythematous papular rash known as ground itch followed by eosinophilia and increased IgE levels. Heavy infections of hookworm are associated with abdominal pain, diarrhea, loss of appetite, weight loss, fatigue and anaemia. Roundworm and Trichuris infection results in atrophy of the intestinal villus and creation of mechanical barrier to nutrient absorption resulting in poor intake of food and malabsorption. Children with increased STH infection are shown to have lower mean haemoglobin, haematocrit and serum ferritin levels as compared to non-infected children [3,14]. Iron deficiency anaemia in children is associated with impaired psychomotor skills and reduced work capacity as adults and in pregnant women it is associated with increased maternal mortality [15]. Several studies have been published that show the effect of anti-helminthic drugs on haemoglobin levels. Two studies published by Stoltzfus RJ et al., indicate that anti-helminthic treatment can improve moderate to severe anaemia in children as young as two-year-old [16,17]. Other studies show similar effects in school going children complemented with hygiene education programs [18]. However, their role in improving anaemia during pregnancy is still debatable [19]. Given the prevalence of STH infections in India and its close association with anaemia, the aim of the present study was to comprehensively analyse the published literature on the topic and provide current information on the correlation of STH infections with anaemia in India.
Materials and Methods
Search Strategy
We did a literature search based on PRISMA guidelines to identify all relevant literature pertaining to anaemia due to helminth infections in India. We systematically search PubMed and Web of Science with the following search terms anywhere in the article: (helminth or hookworm) AND (anemia or anaemia or hemoglobin or haemoglobin) AND India. We searched the databases without any bar on language, date or nature of study from inception upto December 2017. To identify additional studies, reference list of publications were carefully screened.
Eligibility Criteria
Studies that were published from inception upto December 2017 in English language were considered. Initial assessment was based on review of title and abstract of all studies. Full texts of potentially relevant studies were further analysed for soil transmitted helminth related anaemia. Cross-sectional studies and case reports with full text availability and reporting data about STH related anaemia were included in the study. We excluded studies carried out in animals, reviews and studies reporting anaemia due to other parasitic infections.
Data Extraction
The data extracted from the selected publications included first author, date of publication, date of survey, place where the study was carried out, sample size and age, type of diagnostic test performed, study design, percentage anaemic and haemoglobin levels. All the data was entered in excel file and double-checked.
Meta-Analysis
Odds ratio with 95% Confidence Interval (CI) was used as a measure of association for STH infection related anaemia. Odds ratio is considered in this study, since it can inform about the probability of anaemia among patients due to STH infection as a causative factor. The values of odds ratio were calculated from the data extracted from the included studies comparing the frequency of anaemia cases in STH infected patients verses non infected cases; and also by comparing the frequency of non anaemia cases having STH infection with non anaemia cases without STH infection. More value of odds ratio represents more probability of anaemia induced by STH infection. Raw data for anaemia in STH infected and uninfected patients were extracted from tables, figures, texts or summary data from the selected articles. Odds ratio was calculated using online resources (https://www.medcalc.org/calc/odds_ratio.php).
Results
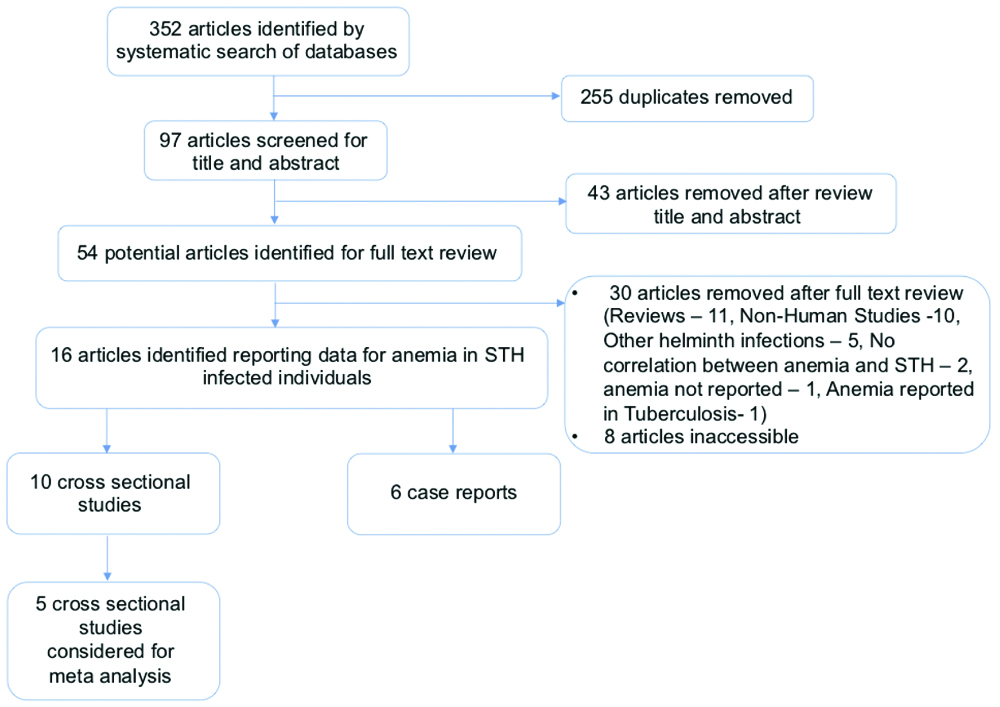
Initial search of the databases with keywords resulted in 352 references [Table/Fig-1]. A total of 97 studies were identified for screening after removal of duplicates. After initial reviewing of title and abstract 54 studies were identified for full text screening out of which 38 studies were excluded with reason (Reviews-11, Non-Human Studies-10, articles inaccessible-8, Other helminth infections-5, No correlation between anaemia and STH-2, anaemia not reported-1, Anaemia reported in Tuberculosis-1). Sixteen potentially relevant studies were identified that reported STH infections along with anaemia or haemoglobin levels from India [20-35]. Out of these references 10 were community based cross-sectional studies and 6 were case reports [Table/Fig-2,3]. Five cross-sectional studies were included in the final qualitative synthesis [Table/Fig-4].
Schematic representation of the study selection process.
General characteristic of cross sectional studies considered for data extraction [20-29].
| S. No. | Author | Date of publication | Age | Method of parasite detection | Parasite detected | N | Infected | Infected | Uninfected | Uninfected | Haemoglobin levels (g/dl) Mean/Median* |
|---|
| Anaemic | Non anaemic | Anaemic | Non anaemic |
|---|
| 1 | Srinivasan V et al., [20] | 1987 | 5-59 | Microscopy | HW | 1113 | 1040 | 894 | 146 | 73 | 49 | 24 | 10.3 |
| 2 | Rao VG et al., [21] | 2003 | Adolescents | Microscopy | HW | 783 | 466 | 410 | 56 | 317 | 235 | 82 | 9.19 |
| 3 | Wani SA et al., [22] | 2008 | 5-15 yrs | Microscopy | AL, TT | 382 | 299 | NR | NR | 83 | NR | NR | 10.54 |
| 4 | Tengse VG et al., [23] | 2011 | 10-20 yrs | Microscopy | AL, TT, HW | 122 | 45 | 35 | 10 | 77 | NR | NR | 10.95* |
| 5 | Sharma SK et al., [24] | 2012 | Adolescent female | Microscopy | AL, TT, HW | 2499 | 424 | NR | NR | 2075 | NR | NR | 11.02 |
| 6 | Shrinivas K et al., [25] | 2014 | 18-35 yrs Pregnant female | Microscopy | AL, HW | 500 | 62 | 55 | 7 | 438 | 245 | 193 | 9.5 |
| 7 | Ramyasree A et al., [26] | 2015 | 1-90 yrs | Microscopy | AL, HW | 238 | 34 | NR | NR | 204 | NR | NR | 13.7 |
| 8 | Ajwani KD et al., [27] | 1974 | 0-10 yrs | Microscopy | AL, TT, HW | 3200 | 435 | 318 | 117 | 2765 | NR | NR | 8.5* |
| 9 | Kumar V et al., [28] | 2003 | 6-10 yrs girls | NR | AL, TT, HW | 716 | 511 | 334 | 177 | 205 | 101 | 104 | 8.2 |
| 10 | Nallam NR et al., [29] | 1998 | 7-13 yrs | Microscopy | AL, TT, HW | 217 | 177 | 157 | 20 | 40 | 32 | 8 | 9.7 |
AL-Ascaris lumbricoides; TT-Trichuris trichiura; HW-Hookworm, *median were reported from these studies
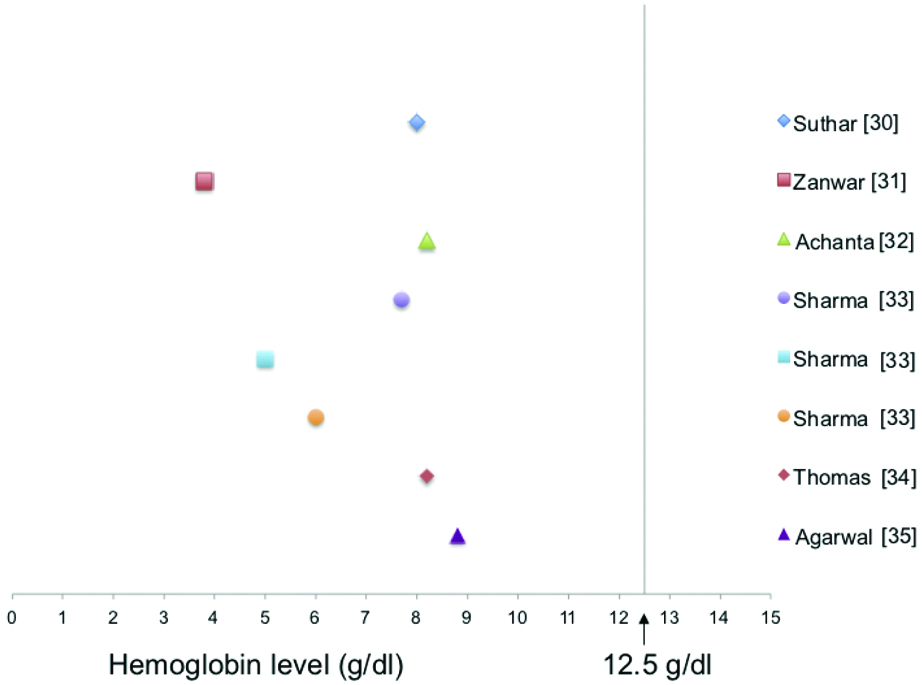
General characteristic of case reports considered for data extraction.
| S. No. | Author | Year of Publication | Age | Method of parasite detection | Parasite detected | Haemoglobin levels (g/dL) |
|---|
| 1 | Suthar PP et al., [30] | 2015 | 10 y | Ultrasound | AL | 8 |
| 2 | Zanwar VG et al., [31] | 2016 | 7 y female | Colonoscopy | TT | 3.8 |
| 3 | Achanta CR, [32] | 2016 | 65 y male | Endoscopy | HW | 8.2 |
| 4 | Sharma V et al., [33] | 2017 | 25 y male | Endoscopy | HW | 7.7 |
| 5 | Sharma V et al., [33] | 2017 | 19 y male | Endoscopy | HW | 5 |
| 6 | Sharma V et al., [33] | 2017 | 62 y female | Endoscopy | HW | 6 |
| 7 | Thomas V et al., [34] | 2006 | 35 y male | Colonoscopy | HW | 8.2 |
| 8 | Agarwal P et al., [35] | 2012 | 6 y female | Microscopy | HW | 8.8 |
AL-Ascaris lumbricoides; TT-Trichuris trichiura; HW-Hookworm
Studies considered for meta analysis.
| S. No. | Author | N | Infected | Infected | Uninfected | Uninfected | Haemoglobin levels (g/dL) | Odds ratio 95% CI |
|---|
| Anaemic | Non anaemic | | Anaemic | Non anaemic | | |
|---|
| 1 | Srinivasan V et al., [20] | 1113 | 1040 | 894 | 146 | 73 | 49 | 24 | 10.3 | 2.992 (1.8, 5.03) |
| 2 | Rao VG et al., [21] | 783 | 466 | 410 | 56 | 317 | 235 | 82 | 9.19 | 2.55 (1.8, 3.72) |
| 3 | Shrinivas K et al., [25] | 500 | 62 | 55 | 7 | 438 | 245 | 193 | 9.5 | 6.2 (2.8, 13.9) |
| 4 | Kumar V et al., [28] | 716 | 511 | 334 | 177 | 205 | 101 | 104 | 8.2 | 1.94 (1.4, 2.7) |
| 5 | Nallam NR et al., [29] | 217 | 177 | 157 | 20 | 40 | 32 | 8 | 9.7 | 1.3 (0.5, 3) |
| Total | | 3329 | 2256 | 1850 | 406 | 1073 | 662 | 411 | | 2.8 (2.4, 3.4) |
Case Reports
The six case reports reported the data from eight individuals, four male, three females and one whose gender wasn’t mentioned, with ages ranging from 7-65 years. Abdominal discomfort, melena, weakness and fatigue were common symptoms reported by the patients. The diagnosis of helminth infection was made by endoscopy in four cases, two cases were diagnosed by colonoscopy and one case each was diagnosed by ultrasound and microscopy. Hookworm was the predominant STH found with six cases reporting the parasite. A. lumbricoides and T. trichiura was reported by one individual each. All of the cases reported severe to moderate anaemia with very low levels of haemoglobin ranging from 3.8-8.8 g/dL [Table/Fig-3,5]. Lowest level of anaemia was found in a seven-year-old girl with Trichuris dysentery syndrome and reported haemoglobin level of 3.8 g/dL.
Haemoglobin levels in case reports.
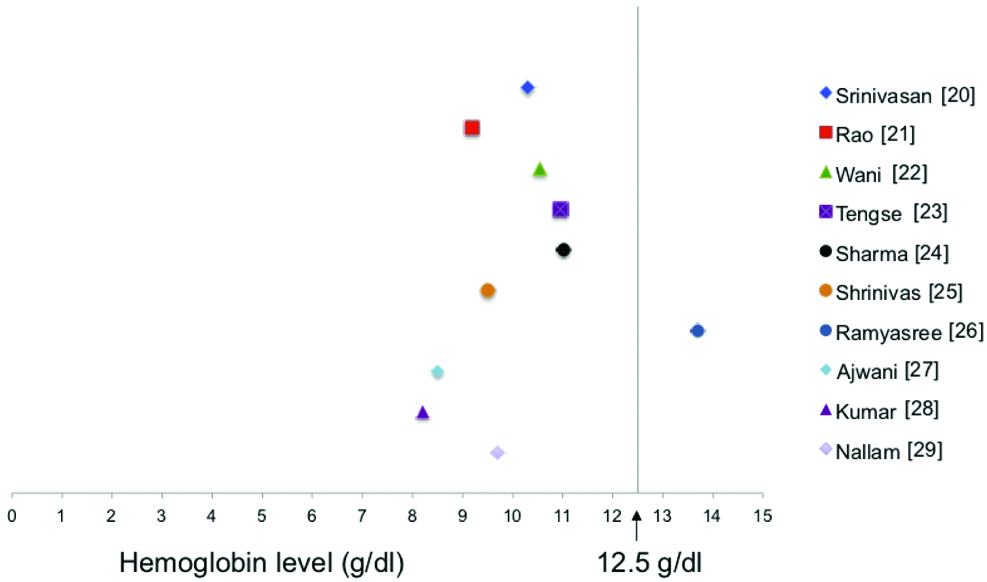
Cross-sectional Studies
Ten cross-sectional studies, reported the data for STH infections and haemoglobin both. Three studies reported the data from children, one study reported the data for female child, two studies reported the data from adolescents, another study reported the data from adolescent female only, two studies reported the data from all age groups, and one study reported the data from pregnant females only. Microscopy was the preferred method of parasite detection. Five studies reported all three STH in the same population; three studies reported either A. lumbricoides and hookworm or A. lumbricoides and T. trichiura in the same populations, while two studies reported hookworm infection only. The percent of infections ranged from 12-93%. Nine studies reported moderate to severe anaemia and low haemoglobin levels which correlates with STH infection [Table/Fig-2,6]. One study reported low haemoglobin levels however they did not found a correlation between STH infection and anaemia in infected verses non infected samples.
Haemoglobin levels in cross-sectional studies.
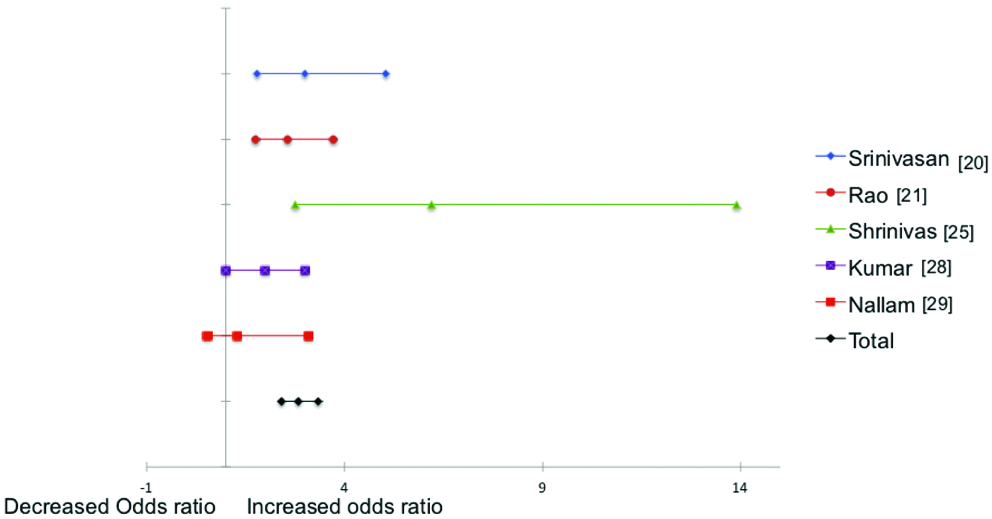
Meta-Analysis
Only five studies had reported data regarding the anaemia levels in infected and uninfected population. These five studies were included in meta-analysis. A total of 3329 patients provided the data on the association between STH infection and anaemia. Higher STH infection was correlated with threefold higher anaemia in patients (OR-2.8 2.4-3.4) [Table/Fig-4,7]. Out of the 10 cross-sectional studies five studies (Wani SA et al., Tengse VG et.al., Sharma SK et al., Ramyasree A et al., and Ajwani KD et al.,) provided no information about anaemia in non-infected population hence they were excluded from the final meta-analysis [22-24,26,27].
Forest plot showing the effect of STH infection on the odds ratio for haemoglobin levels. (OR-2.8, CI-95%, 2.4-3.4). All the studies considered for meta analysis show an increased odds.
Discussion
STH infections constitute significant disease burden in developing parts of the world. Children below the age of 18 are the most affected demographic. Ascaris and Trichuris gain access to human host by ingestion of eggs while hookworm larvae infects human by skin penetration. Once inside the human host they develop into full adult worms. Hookworm parasitizes the upper part of small intestine, Ascaris worms parasitizes small intestine and Whipworm parasitizes the large intestine. Heavy worm infection can cause pain and abdominal distension. They may also lead to malabsorption of vitamin A and other micronutrients. STH infections contribute to anaemia through blood loss and micronutrient deficiency. Hookworm infections particularly, cause blood loss due to its penetration and attachment of mucosa and submucosa and once the blood loss exceed the nutritional reserve of host it leads to iron-deficiency anaemia. The infection can be treated with a single doze of Albendazole and Mebendazole, which inhibit parasite microtubule polymerisation. The global strategy for control of STH infection is based on regular anthelminthic treatment, sanitation and personal hygiene and health education [3,36]. In a previously published study we have looked at the prevalence of STH infections in India by systematically reviewing the published literature and found nearly 30% of India’s population living with more than 50% prevalence [37]. In the current study we have tried to assess the prevalence of anaemia due to STH infections in India based on published literature.
A systematic literature search identified 10 cross-sectional studies and 6 case reports that reported anaemia in STH infected patients. The case reports noted severe STH infection with patients reporting to clinic only after symptoms of gastric pain, melena and fatigue. These are extreme cases with patients reporting in most cases severe hookworm infection, which could be visualised via endoscopy. In four of these cases patients reported severe anaemia and in other four they reported moderate anaemia. In all of these cases anaemia was corrected with Albendazole/Mebendazole therapy indicating damaging effects of STH infections on haemoglobin levels and overall health of the patients. One of the case reports reported the data in a seven-year-old girl presented with Trichuris dysentery syndrome and haemoglobin levels of 3.8 g/dL, indicating that heavy infection with T. trichiura could also lead to anaemia. Another five cross-sectional studies establish a correlation between STH infections and anaemia. In all of these studies mild to moderate anaemia was reported with haemoglobin level ranging from 8.2-11.02 g/dL. However, none of these studies have reported any data about therapeutic approaches and post-therapy haemoglobin levels. An odds ratio analysis of five studies for which complete data on anaemic and non-anaemic population in infected verses uninfected population was available, indicated that STH infected individuals are three times more likely to develop anaemia as compared to uninfected individuals. Ajwani KD et al., and Kumar V et al., also reported severe anaemia in some of the STH infected cases they observed, with haemoglobin levels below 8 g/dL [27,28].
Literature search and data extraction is prone to bias, to this effect we have comprehensively searched the databases with broad search queries, nonetheless two relevant studies from Assam and West Bengal were unavailable due to lack of full text availability. Furthermore, association of STH infection with anaemia is widely reported phenomenon, however there aren’t many studies reporting statistical correlation of STH infection with anaemia. In the cross-sectional studies considered for this meta analysis, none reported the data on socioeconomic status, risk factors, therapeutic approaches or post treatment haemoglobin levels. The aetiology of anaemia could be multifactorial with poor nutrition, STH infections, gender, and socioeconomic status being some of the causes of anaemia. Establishing a statistical correlation with all of these factors will be helpful in tackling the problem.
Limitation
The study had certain limitations. Socio-economic status, risk factors, therapeutic approaches and post-therapy haemoglobin levels were not reported in any of the studies. Further cross-sectional studies and controlled trials should be conducted considering the mentioned parameters.
Conclusion
In the present study we have attempted to analyse the effects of STH infections on anaemia. An analysis of five cross-sectional studies indicates that STH infection is three times more likely to be associated with anaemia as compared to non anaemic individuals. Also, in cases of severe infections as reported by several case reports haemoglobin levels may drop down to abnormally low levels that can be life threatening. The growth stunting and cognitive impairment associated with STH infection is well documented and so does the effect of anti-helminthic drugs in alleviating this problem. This study can provide insights to public health officials and clinicians in establishing a baseline of haemoglobin levels to identify STH associated anaemia and therefore help in establishing robust deworming, iron supplementation and hygiene education programs.
Availability of data and materials: The datasets analysed during the current study is available from the corresponding author on reasonable request.
Authors’ contributions: NS and MF extracted the data. NS and MF analysed the data. NS wrote the manuscript. All the authors read and approved the final manuscript.
AL-Ascaris lumbricoides; TT-Trichuris trichiura; HW-Hookworm, *median were reported from these studies
AL-Ascaris lumbricoides; TT-Trichuris trichiura; HW-Hookworm
[1]. Savioli L, Albonico M, Soil-transmitted helminthiasisNat Rev Microbiol 2004 2(8):618-19.10.1038/nrmicro96215303271 [Google Scholar] [CrossRef] [PubMed]
[2]. Bethony J, Brooker S, Albonico M, Geiger SM, Loukas A, Diemert D, Soil-transmitted helminth infections: Ascariasis, trichuriasis, and hookwormLancet 2006 367(9521):1521-32.10.1016/S0140-6736(06)68653-4 [Google Scholar] [CrossRef]
[3]. Lobo DA, Velayudhan R, Chatterjee P, Kohli H, Hotez PJ, The neglected tropical diseases of India and South Asia: Review of their prevalence, distribution, and control or eliminationPLoS Negl Trop Dis 2011 5(10):e122210.1371/journal.pntd.000122222039553 [Google Scholar] [CrossRef] [PubMed]
[4]. Chammartin F, Scholte RG, Guimaraes LH, Tanner M, Utzinger J, Vounatsou P, Soil-transmitted helminth infection in South America: A systematic review and geostatistical meta-analysisLancet Infect Dis 2013 13(6):507-18.10.1016/S1473-3099(13)70071-9 [Google Scholar] [CrossRef]
[5]. Karagiannis-Voules DA, Biedermann P, Ekpo UF, Garba A, Langer E, Mathieu E, Spatial and temporal distribution of soil-transmitted helminth infection in sub-Saharan Africa: a systematic review and geostatistical meta-analysisLancet Infect Dis 2015 15(1):74-84.10.1016/S1473-3099(14)71004-7 [Google Scholar] [CrossRef]
[6]. World health organisation [Internet] Geneva: Preventive chemotherapy to control soil-transmitted helminth infections in at-risk population groups: 2017 [Cited 15th April 2019] Available from https://www.who.int/neglected_diseases/preventive_chemotherapy/lf/en/ [Google Scholar]
[7]. Ziegelbauer K, Speich B, Mausezahl D, Bos R, Keiser J, Utzinger J, Effect of sanitation on soil-transmitted helminth infection: Systematic review and meta-analysisPLoS Med 2012 9(1):e100116210.1371/journal.pmed.100116222291577 [Google Scholar] [CrossRef] [PubMed]
[8]. Strunz EC, Addiss DG, Stocks ME, Ogden S, Utzinger J, Freeman MC, Water, sanitation, hygiene, and soil-transmitted helminth infection: A systematic review and meta-analysisPLoS Med 2014 11(3):e100162010.1371/journal.pmed.100162024667810 [Google Scholar] [CrossRef] [PubMed]
[9]. Taylor-Robinson DC, Maayan N, Soares-Weiser K, Donegan S, Garner P, Deworming drugs for soil-transmitted intestinal worms in children: effects on nutritional indicators, haemoglobin, and school performanceCochrane Database Syst Rev 2015 (7):CD00037110.1002/14651858.CD000371.pub626202783 [Google Scholar] [CrossRef] [PubMed]
[10]. National Health Portal of India [Internet] Delhi: National Deworming Day. 2019. [Cited 15th April 2019] Available from https://www.nhp.gov.in/national-deworming-day_pg [Google Scholar]
[11]. World health organisation [Internet] Geneva: Deworming in children. 2017 [Cited 15th April 2019] Available from https://www.who.int/elena/titles/deworming/en/ [Google Scholar]
[12]. Foy H, Nelson GS, Helminths in the etiology of anemia in the tropics, with special reference to hookworms and schistosomesExp Parasitol 1963 14:240-62.10.1016/0014-4894(63)90029-8 [Google Scholar] [CrossRef]
[13]. Hotez PJ, Brooker S, Bethony JM, Bottazzi ME, Loukas A, Xiao S, Hookworm infectionN Engl J Med 2004 351(8):799-807.10.1056/NEJMra03249215317893 [Google Scholar] [CrossRef] [PubMed]
[14]. Hesham MS, Edariah AB, Norhayati M, Intestinal parasitic infections and micronutrient deficiency: A reviewMed J Malaysia 2004 59(2):284-93. [Google Scholar]
[15]. Dickson R, Awasthi S, Williamson P, Demellweek C, Garner P, Effects of treatment for intestinal helminth infection on growth and cognitive performance in children: Systematic review of randomised trialsBMJ 2000 320(7251):1697-701.10.1136/bmj.320.7251.169710864543 [Google Scholar] [CrossRef] [PubMed]
[16]. Stoltzfus RJ, Chway HM, Montresor A, Tielsch JM, Jape JK, Albonico M, Low dose daily iron supplementation improves iron status and appetite but not anemia, whereas quarterly anthelminthic treatment improves growth, appetite and anemia in Zanzibari preschool childrenJ Nutr 2004 134(2):348-56.10.1093/jn/134.2.34814747671 [Google Scholar] [CrossRef] [PubMed]
[17]. Stoltzfus RJ, Albonico M, Chwaya HM, Tielsch JM, Schulze KJ, Savioli L, Effects of the Zanzibar school-based deworming program on iron status of childrenAm J Clin Nutr 1998 68(1):179-86.10.1093/ajcn/68.1.1799665112 [Google Scholar] [CrossRef] [PubMed]
[18]. Sufiyan MB, Sabitu K, Mande AT, Evaluation of the effectiveness of deworming and participatory hygiene education strategy in controlling anemia among children aged 6-15 years in Gadagau community, Giwa LGA, Kaduna, NigeriaAnn Afr Med 2011 10(1):6-12.10.4103/1596-3519.7656121311148 [Google Scholar] [CrossRef] [PubMed]
[19]. Salam RA, Haider BA, Humayun Q, Bhutta ZA, Effect of administration of antihelminthics for soil-transmitted helminths during pregnancyThe Cochrane Database Syst Rev 2015 (6):CD00554710.1002/14651858.CD005547.pub3 [Google Scholar] [CrossRef]
[20]. Srinivasan V, Radhakrishna S, Ramanathan AM, Jabbar S, Hookworm infection in a rural community in south India and its association with haemoglobin levelsTrans R Soc Trop Med Hyg 1987 81(6):973-77.10.1016/0035-9203(87)90369-5
[Google Scholar] [CrossRef]
[21]. Rao VG, Aggrawal MC, Yadav R, Das SK, Sahare LK, Bondley MK, Intestinal parasitic infections, anaemia and undernutrition among tribal adolescents of Madhya PradeshIndian J Community Med 2003 28(1):26-29. [Google Scholar]
[22]. Wani SA, Ahmad F, Zargar SA, Dar ZA, Dar PA, Tak H, Soil-transmitted helminths in relation to hemoglobin status among school children of the Kashmir ValleyJ Parasitol 2008 94(3):591-93.10.1645/GE-1400.118605794 [Google Scholar] [CrossRef] [PubMed]
[23]. Tengse VG, Baghel MS, Vyas SN, Joshi JR, A survey on etiopathological correlation of Krimi (intestinal helminths) and Pandu (anemia)Ayu 2011 32(2):165-70.10.4103/0974-8520.9254322408296 [Google Scholar] [CrossRef] [PubMed]
[24]. Sharma SK, Narain K, Devi KR, Mohapatra PK, Phukana RK, Mahanta J, Haemoglobinopathies-major associating determinants in prevalence of anaemia among adolescent girl students of Assam, IndiaWHO South East Asia J Public Health 2012 1(3):299-308.10.4103/2224-3151.20702628615556 [Google Scholar] [CrossRef] [PubMed]
[25]. Shrinivas K, Radhika Sreelatha R, Kavitha K, Study of helminthiasis in pregnancy and its correlation with haemoglobin levelJ Clin Diagn Res 2014 8(10):OC07-09. [Google Scholar]
[26]. Ramyasree A, Prakash R, Kumar S, Kathleen G, Shilpa K, Occurrence of Intestinal Parasitic Infections and its correlation with haemotological Parameters in a tertiary care centreJournal of International Medicine and Dentistry 2015 2(1):47-52. [Google Scholar]
[27]. Ajwani KD, Saxena H, Kumar A, A coprological survey of parasitism in children in KanpurIndian J Pediatr 1974 41(317):209-13.10.1007/BF028748984443027 [Google Scholar] [CrossRef] [PubMed]
[28]. Kumar V, Kumar AH, Sunita V, Kapur I, Prevalence of anemia and worm infestation in school going girls at Gulbarga, KarnatakaIndian Pediatr 2003 40:70-72. [Google Scholar]
[29]. Nallam NR, Paul I, Gnanamani G, Anemia and hypoalbuminia as an adjunct to soil-transmitted helminthiasis among slum school children in Visakhapatnam, South IndiaAsia Pac J Clin Nutr 1998 7(2):164-69. [Google Scholar]
[30]. Suthar PP, Doshi RP, Mehta C, Vadera KP, Incidental detection of ascariasis worms on USG in a protein energy malnourished (PEM) child with abdominal painBMJ Case Rep 2015 2015:pii:bcr201420666810.1136/bcr-2014-20666825766437 [Google Scholar] [CrossRef] [PubMed]
[31]. Zanwar VG, Pawar SV, Jain SS, Rathi SP, Contractor QQ, Rathi PM, An unusual cause of overt gastrointestinal bleeding in a malnourished childTrop Doct 2016 46(2):100-02.10.1177/004947551559866726264463 [Google Scholar] [CrossRef] [PubMed]
[32]. Achanta CR, Image diagnosis: gastric migration of hookworms in a patient with anemiaPerm J 2016 20(3):15-201.10.7812/TPP/15-20127352415 [Google Scholar] [CrossRef] [PubMed]
[33]. Sharma V, Gunjan D, Chhabra P, Sharma R, Rana SS, Bhasin DK, Gastrointestinal bleeding in the tropics: Look for the hookwormTrop Doct 2017 47(1):48-51.10.1177/004947551664019227075012 [Google Scholar] [CrossRef] [PubMed]
[34]. Thomas V, Harish K, Tony J, Sunilkumar R, Ramachandran TM, Anitha PM, Colitis due to Ancylostoma duodenaleIndian J Gastroenterol 2006 25(4):210-11. [Google Scholar]
[35]. Agarwal P, Singh D, Sinha G, Sharma N, Titiyal JS, Bilateral Mooren’s ulcer in a child secondary to helminthic infestation of the gastrointestinal tractInt Ophthalmol 2012 32(5):463-66.10.1007/s10792-012-9520-x22661075 [Google Scholar] [CrossRef] [PubMed]
[36]. Mascarini-Serra L, Prevention of soil-transmitted helminth infectionJ Glob Infect Dis 2011 3(2):175-82.10.4103/0974-777X.8169621731306 [Google Scholar] [CrossRef] [PubMed]
[37]. Salam N, Azam S, Prevalence and distribution of soil-transmitted helminth infections in IndiaBMC Public Health 2017 17(1):20110.1186/s12889-017-4113-228209148 [Google Scholar] [CrossRef] [PubMed]