Case Report
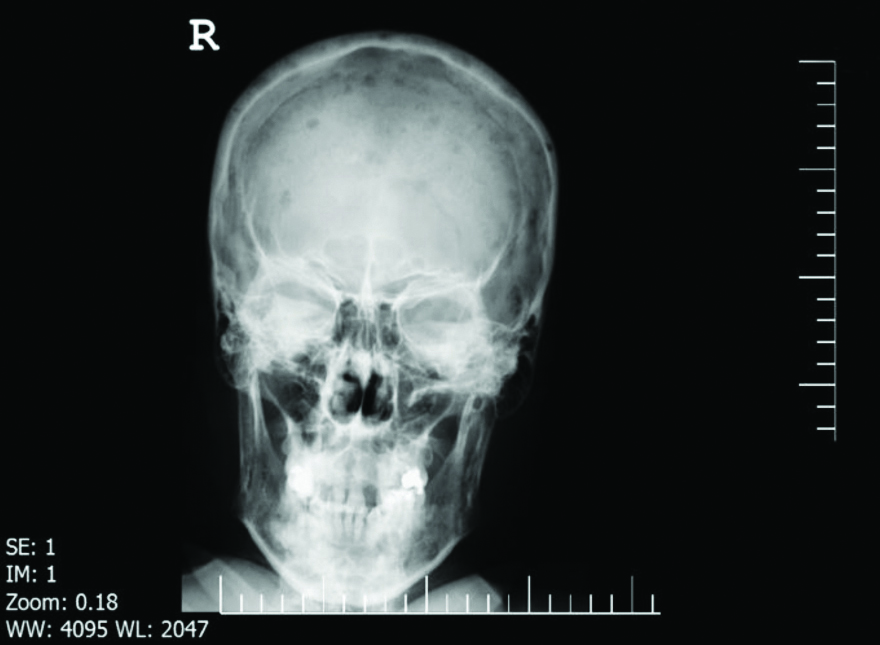
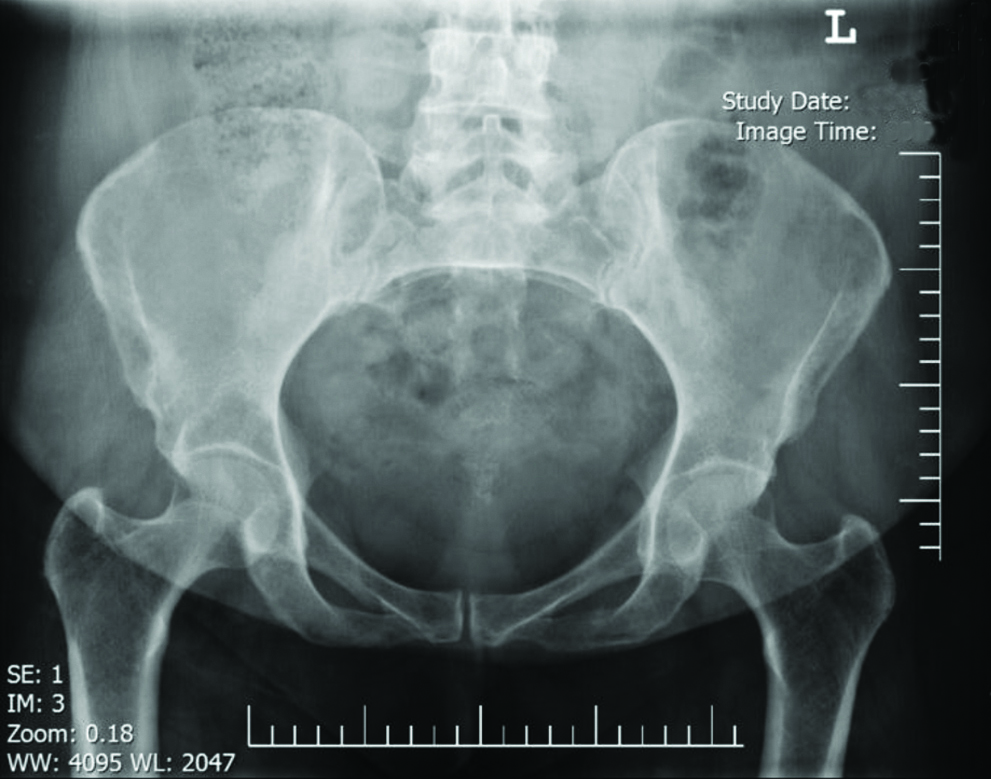
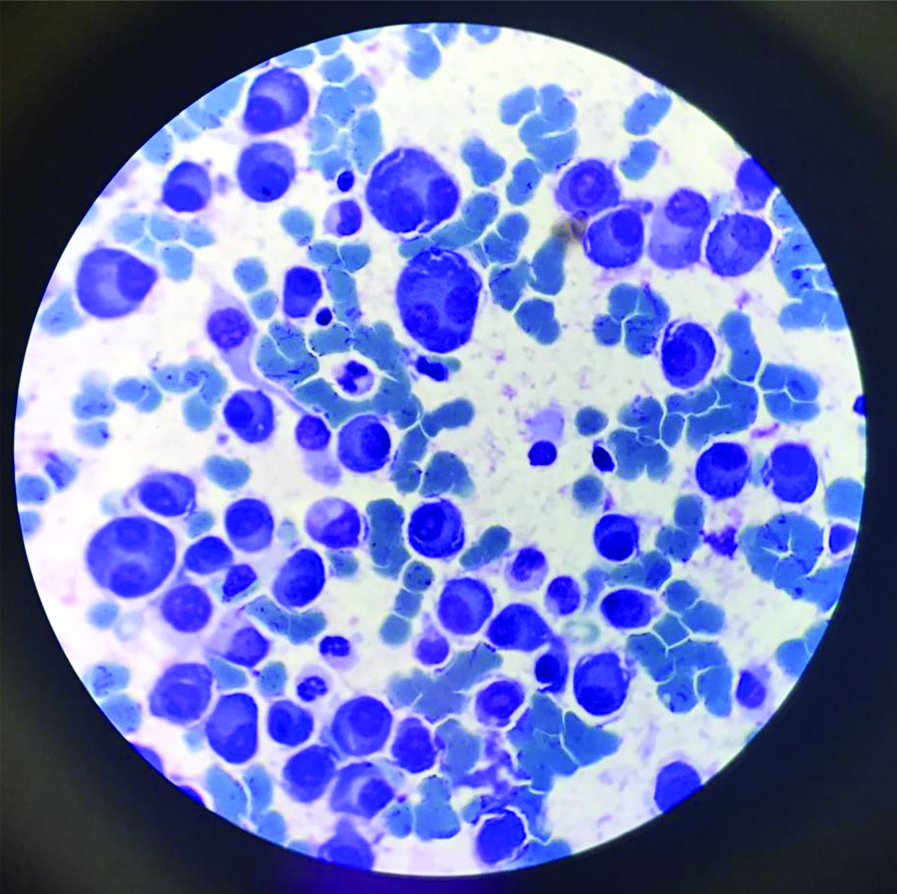
A 44-year-old woman, known case of sarcoidosis since 2013, with below presentations: fever, erythema nodosum, and arthritis of both ankles, bilateral hilar lymphadenopathy and maculopapular skin lesions on her forehead in which, the pathologic evaluation revealed granulomatous inflammation without caseation. She also suffers from proteinuria about 2 g/day, which reported as Focal Segmental Glomerulosclerosis (FSGS) secondary to sarcoidosis after renal biopsy and thorough evaluation. She received a moderate dose of steroid (20 mg of prednisolone), with gradual tapering and angiotensin receptor blocker (100 mg of losartan) for 18 months and both sarcoidosis involvements and proteinuria were completely relieved. Differential diagnosis for multiple lytic leisions were Myeloma, Fibrose dysplasia, Eosinophilic granuloma, Enchondroma, Metastatic disease, Hyperparathyroidism (brown tumors), infection based on multiple bone sites pain that worsen with activity, whole body scan was noted for high abnormal uptake at the skull regions, both shoulders, half proximal of right humerus shaft, ribs and lumbar vertebras at multiple levels as well as both sacroiliac joints. Skeletal survey showed multiple lytic lesions in her skull [Table/Fig-1,2], ribs, vertebras and iliac bone [Table/Fig-3]. A typically normochromic normocytic anaemia, proteinuria, presence of monoclonal protein in urine electrophoresis [Table/Fig-4], and presence of more than 90% plasma cells in bone marrow biopsy, the patient was diagnosed with Multiple Myeloma (MM) and was treated accordingly.
Anterior view of the skull shows multiple well defined lytic lesions.
Lateral view of the skull shows multiple well defined lytic lesions.

Anterior view of the pelvis shows a large great lytic lesion on wing of left iliac bone.
Monoclonal protein was found in urine electrophoresis.
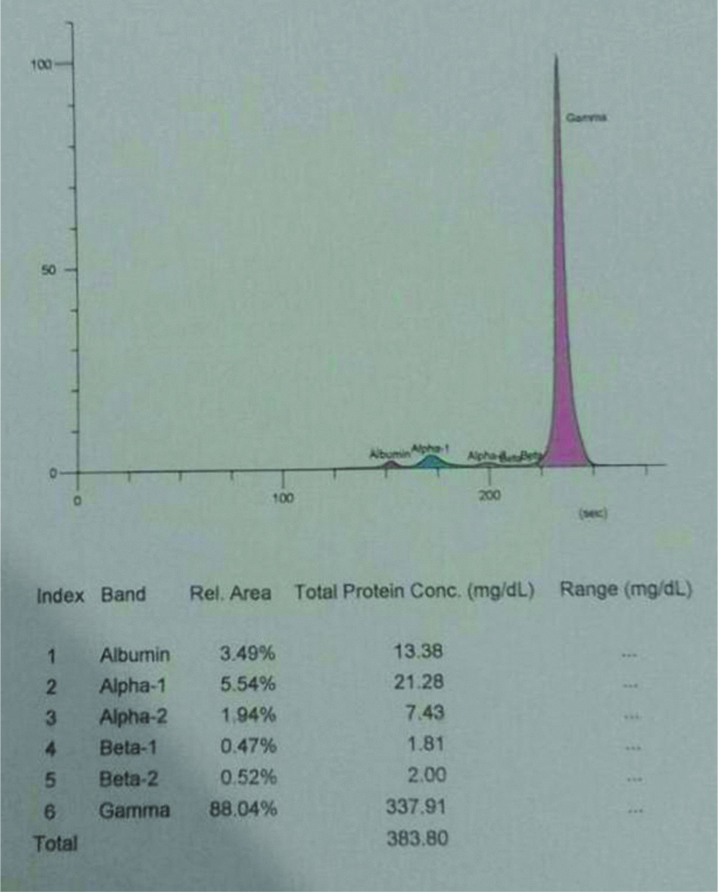
However, after two years of remission, during her routine follow-up, she developed pain in spinal vertebras, ribs, pelvis, besides pitting oedema over the legs, normochromic and normocytic anaemia (Hb: 9.3), ESR of 110 and proteinuria more than 3 g/day, presence of monoclonal protein in urine electrophoresis, serum protein electrophoresis showed high alpha 1, alpha 2, beta 1 proteins but lower percentages of gamma proteins. The rest of laboratory exams were unremarkable.
The patient received cyclophosphamide (150 mg/m2/d) for four consecutive days Bortezomib (1.3 mg/m2) and dexamethsasone (20 mg/m2) for four doses at 1st, 4th, 8th and 11th days of treatment.
Having completed chemotherapy, bone marrow plasma cells reached 8% and there were no peak of the serum or urine protein.
On physical examination, the patients was febrile (38.5°C), there were maculopapular lesions on her forehead and erythema nodosum as well as arthritis in both ankles. Additionally, a pitting oedema was noticed over legs. There was pain in multiple bone sites such as spinal vertebras, ribs and pelvis.
As MM was suspected, further evaluation was done and more than 90%, CD 138+ plasma cells were detected in bone marrow biopsy [Table/Fig-5].
In bone marrow biopsy, more than 90% plasma cells were detected.
The patient fully met diagnostic criteria for symptomatic MM and chemotherapy was begun for her with Velcade, cyclophosphamide and dexamethasone.
Discussion
Sarcoidosis is an inflammatory disease with characteristic pathological feature of noncaseating granuloma [1]. MM is a dyscrasias of bone-marrow plasma cells which can lead to end organ damage, in form of lytic bone lesions, hypercalcaemia, renal failure and recurrent infection [2].
Although the concurrence of sarcoidosis and MM has been reported in other case reports in literature, the coincidence is still rare [3-5]. Thirteen cases of MM and sarcoidosis have been reported in literature [6,7]. Besides, familial type of MM with a history of sarcoidosis has also been reported [8]. As the incidence of MM is relatively high, about five cases per 100,000 each year, there is no discrete trial in estimating this disease in sarcoidosis patients [9].
Immune system impairment in sarcoidosis may predispose patients to develop MM and other haematologic malignancies. Besides, genetic instability due to aneuploidy of sarcoidosis granuloma cells and peripheral blood lymphocytes may predispose patients to develop malignancies [6].
Kidney impairment occurs in 10-20% of patients with sarcoidosis. Sarcoidosis involve kidney in different ways, the most common cause of kidney injury is abnormality in calcium hemostasis, including hypercalciuria and hypercalcaemia in 50% and 10% of patients, respectively, nephrocalcinosis and nephrolithiasis [10,11]. Granulomatosis tubulointerstitial nephritis is less common and involves about 20% of patients and glomerular involvement is heterogenic, rare and exclusively few case reports were published. Wide spectrum of glomerular lesions were reported including Membranous Nephropathy (MN), Minimal Change Disease (MCD), Focal Segmental Glomerulosclerosis (FSGS), Immunoglobulin A Nephropathy (IgA N), amyloidosis and proliferative Glomerulonephritis (GN). MN is the most frequent glomerular disease and FSGS is rare in sarcoidosis [12-14]. In one study, simultaneous occurrence of sarcoidosis and glomerular lesion was only 35% [11].
Sarcoidosis is an inflammatory disease with increased infiltration of Th1 cells and increased Th1/Th2 cytokines level, these changes in immune system may be a predisposing factor for GN.
Kidney involvement is common in MM. Light chain deposition disease, cast nephropathy (myeloma kidney) and amyloidosis are some of its types, but GN is a rare manifestation. Different types of GN, FSGS, MN, fibrillary GN, immunotactoid glomerulopathy, membranoproliferative GN, C3 glomerulopathy and cryoglobulinemia were reported [15,16]. GN can occur several months before diagnosis of MM, however in most cases, MM may be diagnosed during evaluation for proteinuria and GN [17]. Occurrence of MM and FSGS either simultaneously or sequentially is rare. Furthermore, there are some reports that FSGS had been presented several months before MM [18,19].
Our patient was a 44-year-old woman with documented sarcoidosis based on clinical presentation and pathologic findings together with biopsy proven FSGS for four years. After two years of remission, she was revaluated because of proteinuria, bone pain, high ESR and the diagnosis of MM was developed based on skeletal lytic lesion in radiologic survey and detection of more than 90% CD 138+ plasma cells in bone marrow biopsy. There are few case reports of concurrence of sarcoidosis and MM together and FSGS is reported as a rare kidney presentation of both sarcoidosis and MM, our patient is the first report of correlation of these three diseases and immune system impairment may be main predisposing factor.
Previous studies showed, renal involvement in sarcoidosis can occur in 50% of patients, while glomerular disease occurs in 7% of the patients consist of membranous GN, FSGS, Minimal change disease and IgA nephropathy [16,19]. FSGS is rare presentation of both MM and sarcoidosis and 13 cases of occurrence of MM with sarcoidosis have been reported in literature [20,21]; however, concurrence of sarcoidosis with MM and FSGS have not been reported.
The patient complained of proteinuria five years ago. We found that the reason may be because that sarcoidosis treatment (corticosteroid with high dosage) did not work in this case and the symptom of proteinuria improved. Meanwhile, the patient showed proteinuria symptoms, light chain and some other symptoms two months before treatment. We can conclude that the first kidney disorder was not related to MM. Now, the question is whether there is a possibility to have proteinuria with multiple myeloma?
Conclusion
In this article, we present a case of sarcoidosis, who suffered from proteinuria through biopsy proven FSGS and subsequent occurrence of MM through the course of disease. Although there is no obvious elucidation for this coherence, immune system dysfunction and genetic instability may be incorporated. It is appropriate that clinicians to be conscious of possibility of coincidence of MM and FSGS in patients with sarcoidosis who be afflicted by proteinuria and bone pain.
Declaration
Ethical approval and consent to participate: The ethics committee approved this study.
Consent for publication: Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Availability of data and material: All data generated or analysed during this study are included in this published article.
Funding: This study was granted by Tehran University of Medical Science, Tehran, Iran.
Authors’ contributions: BA, being the first author, drafted the initial manuscript and EA were involved in the care of the patient and edited and approved the final manuscript. SA, being the corresponding author made the pathological diagnosis and provided the figures for the manuscript and reviewed and revised the manuscript and approved the final manuscript as submitted. All authors read and approved the final manuscript and agree to be accountable for all aspects of the work.
Abbreviations
Membranous Nephropathy (MN)
Minimal Change Disease (MCD)
Focal Segmental Glomerulosclerosis (FSGS)
Immunoglobulin A Nephropathy
Amyloidosis and Proliferative Glomerulonephritis (APG)
Glomerulonephritis (GN)
Multiple Myeloma (MM)
[1]. Larici AR, Glaudemans AW, Del Ciello A, Slart RH, Calandriello L, Gheysens O, Radiological and nuclear medicine imaging of sarcoidosisQ J Nucl Med Mol Imaging 2018 62(1):14-33. [Google Scholar]
[2]. Loffler C, Bergner R, Sarcoidosis: Renal manifestationsZ Rheumatol 2017 76(5):398-407.10.1007/s00393-017-0301-928405755 [Google Scholar] [CrossRef] [PubMed]
[3]. Blankstein R, Kramer CM, Chandrashekhar Y, The challenges of diagnosing cardiac sarcoidosisJACC Cardiovascular Imaging 2017 10(12):1534-36.10.1016/j.jcmg.2017.11.00629216980 [Google Scholar] [CrossRef] [PubMed]
[4]. PDQ Adult Treatment Editorial BoardPlasma Cell Neoplasms (Including Multiple Myeloma) Treatment (PDQ®): Patient Version. 2018 Jun 19In: PDQ Cancer Information Summaries [Internet] 2002 Bethesda (MD)National Cancer Institute (US) [Google Scholar]
[5]. Sen F, Mann KP, Medeiros LJ, Multiple myeloma in association with sarcoidosisArch Pathol Lab Med 2002 126(3):365-68. [Google Scholar]
[6]. Brown G, Shapeero LG, Weiss BM, Roschewski M, Multiple myeloma with lacrimal gland amyloidosis and sarcoidosisAm J Hematol 2010 85(7):506-09.10.1002/ajh.2169520575017 [Google Scholar] [CrossRef] [PubMed]
[7]. Kusaba K, Kojima K, Naito S, Taba M, Kai K, Ureshino H, Paraneoplastic sarcoidosis in multiple myelomaIntern Med 2017 56(15):2049-51.10.2169/internalmedicine.56.833128768979 [Google Scholar] [CrossRef] [PubMed]
[8]. Nair V, Prajapat D, Talwar D, Sarcoidosis and multiple myeloma: Concurrent presentation of an unusual associationLung India 2016 33(1):75-78.10.4103/0970-2113.17306826933313 [Google Scholar] [CrossRef] [PubMed]
[9]. Dachs R, Horn A, Koornhof H, de Jager L, Maqungo S, Roche S, Double pathology, sarcoidosis associated with multiple myeloma: A case reportJ Bone Oncol 2014 3(2):61-65.10.1016/j.jbo.2014.02.00226909299 [Google Scholar] [CrossRef] [PubMed]
[10]. Ozet A, Guran S, Beksac M, Familial multiple myeloma associated with disorders of chronic inflammation: first report from TurkeyClin Lymphoma Myeloma 2008 8(4):246-48.10.3816/CLM.2008.n.03318765313 [Google Scholar] [CrossRef] [PubMed]
[11]. Kazandjian D, Multiple myeloma epidemiology and survival: A unique malignancySemin Oncol 2016 43(6):676-81.10.1053/j.seminoncol.2016.11.00428061985 [Google Scholar] [CrossRef] [PubMed]
[12]. Al-Kofahi K, Korsten P, Ascoli C, Virupannavar S, Mirsaeidi M, Chang I, Management of extrapulmonary sarcoidosis: challenges and solutionsTher Clin Risk Manag 2016 12:1623-34.10.2147/TCRM.S7447627853374 [Google Scholar] [CrossRef] [PubMed]
[13]. Stehlé T, Joly D, Vanhille P, Boffa JJ, Rémy P, Mesnard L, Clinicopathological study of glomerular diseases associated with sarcoidosis: A multicenter studyOrphanet J Rare Dis 2013 8:6510.1186/1750-1172-8-6523631446 [Google Scholar] [CrossRef] [PubMed]
[14]. Peces R, de la Torre M, Sanchez-Fructuoso A, Escalada P, Focal segmental glomerulosclerosis associated with pulmonary sarcoidosiNephron 1993 65(4):656-57.10.1159/0001875918302436 [Google Scholar] [CrossRef] [PubMed]
[15]. Veronese FJ, Henn Lde A, Faccin CS, Mussatto AV, Paiva Neto A, Edelweiss MI, Pulmonary sarcoidosis and focal segmental glomerulosclerosis: case report and renal transplant follow-upNephrol Dial Transplant 1998 13(2):493-95.10.1093/oxfordjournals.ndt.a0278559509472 [Google Scholar] [CrossRef] [PubMed]
[16]. Altiparmak MR, Oygar D, Bilir M, Kilicarslan I, Serdengecti K, A rare cause of focal segmental glomerulosclerosis: sarcoidosisNephron 2002 90(2):211-12.10.1159/00004904411818707 [Google Scholar] [CrossRef] [PubMed]
[17]. Doshi M, Lahoti A, Danesh FR, Batuman V, Sanders PW, Paraprotein-related kidney disease: Kidney injury from paraproteins-what determines the site of injury?Clin J Am Soc Nephrol 2016 11(12):2288-94.10.2215/CJN.0256031627526707 [Google Scholar] [CrossRef] [PubMed]
[18]. Motwani SS, Herlitz L, Monga D, Jhaveri KD, Lam AQ, Paraprotein-related kidney disease: glomerular diseases associated with paraproteinemiasClin J Am Soc Nephrol 2016 11(12):2260-72.10.2215/CJN.0298031627526706 [Google Scholar] [CrossRef] [PubMed]
[19]. Vakili Sadeghi M, Akbari R, Glomerulonephritis as a type of kidney injury in multiple myeloma: a report of 2 casesIran J Kidney Dis 2017 11(3):249-52. [Google Scholar]
[20]. Dong ZY, Xing HT, Wang YD, Zhang W, Qiu Q, Chen XM, Multiple myeloma with a previous diagnosis of focal segmental glomerulosclerosis: A case report and review of the literatureOncol Lett 2015 10(5):2821-27.10.3892/ol.2015.366926722248 [Google Scholar] [CrossRef] [PubMed]
[21]. Valizadeh N, Makhdomi K, Noroozinia F, Behzadi F, Multiple myeloma presenting with focal segmental glomerulosclerosisSouth Asian J Cancer 2013 2(3):16810.4103/2278-330X.11414624455610 [Google Scholar] [CrossRef] [PubMed]