Cirrhosis of liver is the final common histological pathway for a wide range of chronic liver diseases. The pathological hallmark of cirrhosis is the development of scar tissue replacing the normal parenchyma, which blocks the portal blood vessels through the organ and thus disturb the normal function of the liver [1]. Clinically, it is one of the chronic liver diseases of varied aetiology, which attains a course of manifestations of hepatic insufficiency and portal hypertension. Though the epidemiology of cirrhosis is not fully established in the developing countries, it is one of the leading causes of death among the productive age groups in the developed countries [2]. It was the 10th leading cause of death in men and the 12th in women in the United States in 2001 [3]. Aetiology of cirrhosis is seen to be broad, such as alcoholic, post viral hepatitis (hepatitis B and C), Non-Alcoholic Fatty Liver Disease (NAFLD, NASH), cryptogenic, metabolic (haemochromatosis or Wilson’s disease), biliary, autoimmune hepatitis, toxins and therapeutic agents (e.g., methotrexate, amiodarone) and hepatic venous outflow obstruction (Veno occlusive disease, Budd Chiari syndrome, Constrictive pericarditis). Most of the times, cirrhosis may remain clinically asymptomatic until decompensated [4]. Patients with decompensated liver disease present with complications such as ascites, spontaneous bacterial peritonitis, jaundice, autonomic neuropathy etc. Scanty literature on various complications associated with cirrhosis in NE India prompted us to conduct the study in Gauhati Medical College and Hospital (GMCH) which represents the patients from diverse NE communities [5,6]. Hence the present study was conducted with the aim to determine the clinical spectrum of patients with chronic liver disease with reference to its aetiology, clinical manifestations, complications and causes of death in Gauhati Medical College & Hospital.
Materials and Methods
This cross sectional study was done in the Department of Medicine in Gauhati Medical College and Hospital from September 2016 to December 2017. After obtaining the Ethical clearance from the Institutional Ethical Committee, informed written consent was taken from each patient enrolled in the study. The sample size was calculated using the formula n=4 (pq/L2) where p=population proportion of positive character, q=1-p and L=allowable error [7]. For the present study, L was taken to be 3% and the minimum known overall prevalence at 4.5% [8]. Putting these values in the formula, the sample size was calculated to be 191 and we enrolled 200 patients above 12 years of age and both sexes having features of cirrhosis of liver. A detailed history, thorough clinical examination and relevant investigations were done in these patients to confirm the diagnosis and also to determine the presence of various complications in them.
Diagnostic Criteria for Various Complications
Cirrhosis was diagnosed on the basis of Ultrasonography and diagnosis was confirmed by biopsy whenever possible. Patients with Cirrhosis were classified using Child Turcotte Pugh Score (CTP score) into Grade A, B, and C. Child-Pugh score has been widely used to assess the severity of liver dysfunction in clinical work [9].
NASH was diagnosed on the basis of the presence of metabolic syndrome in patients without a significant alcohol history and exclusion of the other known causes of cirrhosis together with the presence of 4 or 5 of the following features- total cholesterol >200 mg/dL, ALT >30 U/L, AST/ALT ≤1, y- GT >30 U/L and abnormal ultrasound (bright echogenecity of liver, vascular blurring and deep attenuation of the ultrasound signal) [10].
Spontaneous Bacterial Peritonitis- An ascitic fluid neutrophil count greater than 250 cells/ mm3 in the absence of a primary source of infection [11]. An ascitic fluid ADA level of above 39 U/L was taken as a marker for tuberculousascitis [12].
Hepatic Encephalopathy was diagnosed and graded on the basis of the West Haven Criteria [13].
UGI endoscopy was done to detect the presence of gastroesophageal varices/Portal Hypertensive Gastropathy (PHG). Varices were classified as small and large. PHG was identified by the presence of a mosiac like pattern with small polygonal areas surrounded by a whitish yellow depressed border on endoscopy [14].
Hyponatremia was defined by a serum sodium level less than 130 mEq/L in the setting of ascites and/or oedema in the absence of a precipitating factor like drugs (diuretics) or GI losses (vomiting, diarrhoea etc.,) [15].
Coagulopathy was identified on the basis of a low platelet count (<150,000/μL) and/or a prolonged PT.
Statistical Analysis
The data was collected and tabulated as percentage of the values obtained using Microsoft Excel 2013 SPSS version 21.
Results
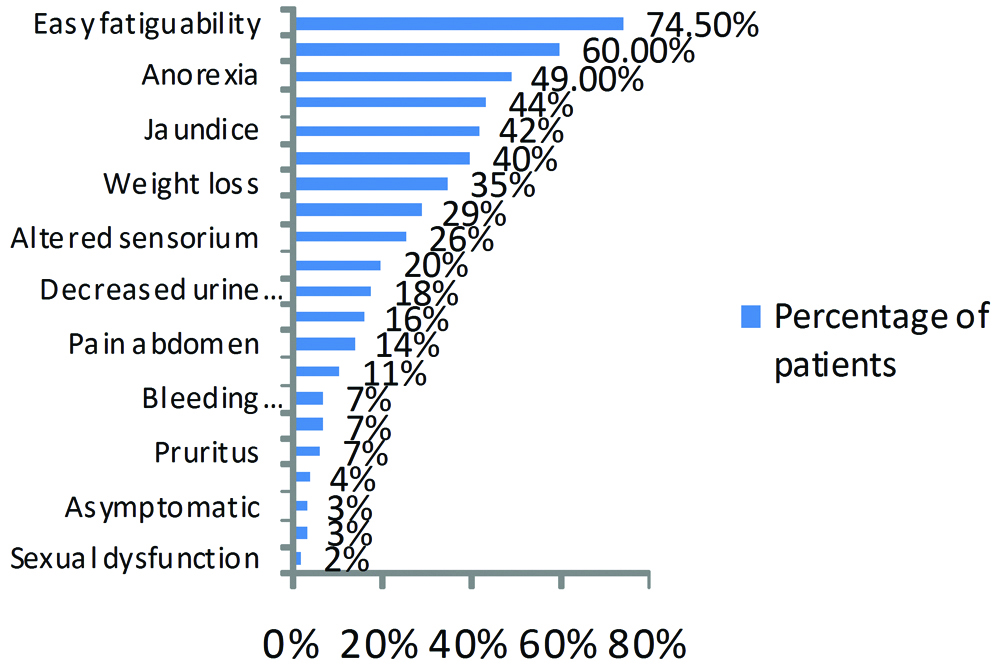
The maximum number of patients of cirrhosis were between 40-59 years of age (57.5%) with the lowest age as 13 years whereas the oldest one was 87 years in the present study. An 80.5% of the study population were males. A 60% of the cases presented within 6 months of the onset of symptoms. In 2% cases the diagnosis of cirrhosis was incidentally done during routine evaluation. A 49.21% of patients in the study gave history of alcohol intake for 5-15 years, 82.81% of them consumed alcohol daily and majority of them consumed between 601-900 mL/day (35.15%). In the present study, easy fatigability was the most common presenting symptom (74.5% of the cases) followed by abdominal distension (60%) and anorexia (49%). 40% of the patients presented with sleep disturbances and 29% had UGI bleed. Pain abdomen (14%), fever (11%) and bleeding manifestations (7%) were other presenting symptoms. A 3% of patients were found to be asymptomatic and many patients presented with multiple symptoms [Table/Fig-1].
Percentage of multiple symptoms among the patients in the study.
On examination, Pallor was the most common finding present in 82% of the patients, followed by splenomegaly in 64% and ascites in 62% patients. 44% patients had pedal oedema. Icterus was present in 40% of the patients, asterixis in 37%, hepatomegaly in 23% and abdominal tenderness in 15.5% of the patients. Many patients had more than one examination finding. Alcohol was the most common aetiological factor for cirrhosis followed by Hepatitis B, cryptogenic, NASH and Hepatitis C [Table/Fig-2].
Aetiology of cirrhosis as observed in the study.
| Cause | No. of Patients | Percentage (%) |
|---|
| Alcohol | 125 | 62.5 |
| Hepatitis B | 22 | 11 |
| Hepatitis C | 7 | 3.5 |
| Alcohol+ Hepatitis B | 3 | 1.5 |
| NASH | 18 | 9 |
| Wilson’s disease | 2 | 1 |
| Haemochromatosis | 2 | 1 |
| Autoimmune hepatitis | 2 | 1 |
| Cryptogenic | 19 | 9.5 |
*NASH: Non alcoholic steato hepatitis
Laboratory Findings
Findings of the blood investigations and biochemical tests are represented in the [Table/Fig-3].
Laboratory findings of the patients.
| Investigations | Blood levels | No. of patients (n) | Percentage (%) |
|---|
| Blood picture | Haemoglobin (gm/dL) | <6 | 29 | 14.5 |
| 6-12 | 139 | 69.5 |
| 12.1-15 | 22 | 11 |
| >15 | 10 | 5 |
| TLC (per mm3 of blood) | Normal | 99 | 49.5 |
| <4,000 | 54 | 27 |
| >11,000 | 47 | 23.5 |
| Platelet count (per mm3 of blood) | Normal | 44 | 22 |
| <1,50,000 | 156 | 78 |
| Prothrombin Time (no. of seconds prolonged than normal) | Normal | 36 | 18 |
| 1-6 | 99 | 49.5 |
| 6-10 | 44 | 22 |
| >10 | 21 | 10.5 |
| Biochemical findings | Bilirubin (mg/dL) | < 2 | 102 | 51 |
| 2-15 | 77 | 38.5 |
| > 15 | 21 | 10.5 |
| AST (U/L) | <40 | 34 | 17 |
| 41-100 | 98 | 49 |
| 101-200 | 48 | 24 |
| >200 | 20 | 10 |
| ALT (U/L) | <40 | 99 | 49.5 |
| 41-100 | 56 | 28 |
| 101-200 | 32 | 16 |
| >200 | 13 | 6.5 |
| AST/ALT ratio | >2 | 75 | 37.5 |
| Albumin (gm/dL) | <3 | 153 | 76.5 |
| 3-3.5 | 33 | 16.5 |
| >3.5 | 14 | 7 |
| Creatinine (mg/dL) | Normal | 183 | 91.5 |
| >3 | 17 | 8.5 |
| Sodium (mmol/L) | Normal | 116 | 58 |
| <130 | 84 | 42 |
| Potassium (mmol/L) | Normal | 158 | 79 |
| <3.6 | 42 | 21 |
| Ammonia (mmol/L) | <20 | 48 | 24 |
| >20 | 152 | 76 |
Ultrasonography: An 82% of patients had evidence of splenomegaly, 77.5% had features suggestive of chronic hepatic parenchymal disease and 64% patients had ascites. Pleural effusion was detected in 16.5% of the patients and in 42.42% of the patients it was right sided. A 3.5% of the patients had evidence of hepatic SOL and in 2.5% of the patients had evidence of portal vein thrombosis.
Upper GI endoscopy: The most common finding detected on an upper gastrointestinal endoscopy was the presence of gastroesophageal varices in 74.5%, of which 55.03% had large varices. There was also evidence of the presence of PHG in 41% of the patients. A 2% of the patients had a normal UGI endoscopy [Table/Fig-4].
Upper Gastrointestinal Endoscopy of the 200 study patients from the study.
| UGI endoscopy findings | No. of patients | Percentage (%) |
|---|
| Normal | 4 | 2 |
| Varices (n=149) | Large | 82 | 55.03 |
| Small | 67 | 44.96 |
| Congestive gastropathy | 82 | 41 |
| Ulcers/Erosions | 66 | 33 |
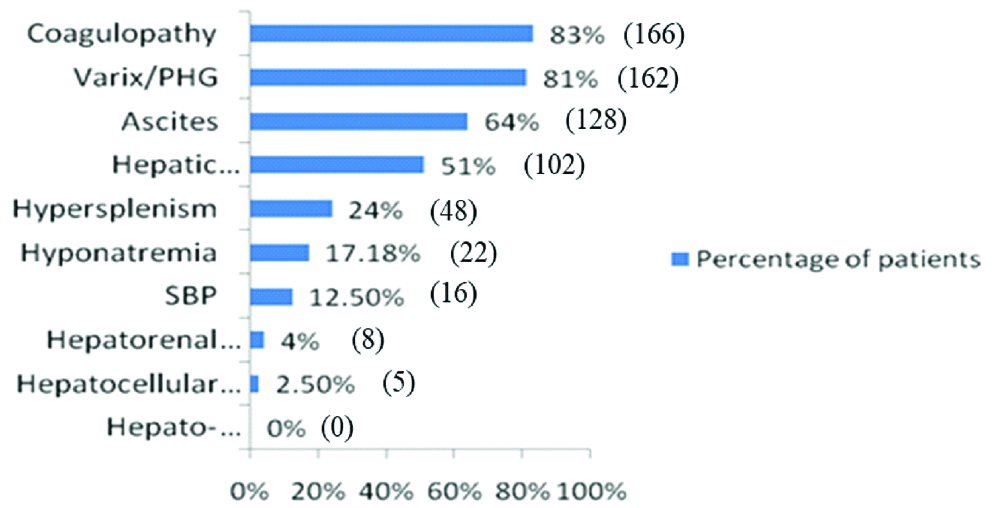
Complications: Coagulopathy and gastroesophageal varices/PHG were the most common complications detected in cirrhotic patients (83% and 81% patients, respectively). Ascites was present in 64% of the patients, hepatic encephalopathy in 51% (mostly Grade I and Grade II encephalopathy according to the West Haven Criteria), hypersplenism in 24%, hyponatremia in 17.18%, SBP in 12.5% (diagnosed SBP if the ascitic fluid polymorphonuclear count >250 cells/mm3. The most common organisms detected in ascitic fluid cultures of SBP patients were E. coli and Klebsiella), hepatorenal syndrome in 4% and hepatocellular carcinoma in 2.5% of the patients [Table/Fig-5].
Complications observed in the study. The numbers in the brackets indicate the number of patients with various complications of cirrhosis of liver.
The CTP score was calculated on the basis of the values of serum albumin, serum bilirubin, prothrombin time (expressed as number of seconds elevated), degree of hepatic encephalopathy and ascites. On this basis, the score was found to be less than 7 in 6.5% (Child Pugh A), 7-9 in 41% (Child Pugh B) and >9 in 52.5% (Child Pugh C) of the patients respectively [Table/Fig-6].
Figure showing the CTP score of the study population. Here, A denotes Child Pugh-A (score of 5-6) which was found to be less than 7 in 6.5%, B denotes Child Pugh-B (score of 7-9) which was found to be less than 7-9 in 41% and C denotes Child Pugh-C (10 or above) which was found to be more than 9 in 52.5% of the patients.
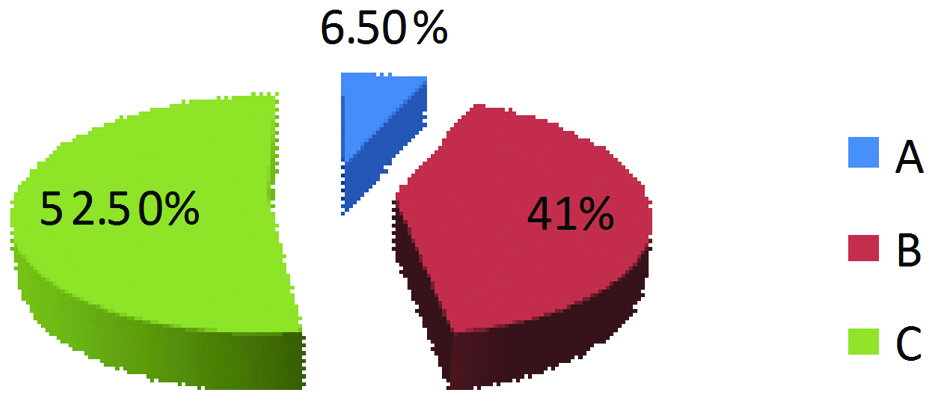
The average length of hospital stay was 11 days (SD±8) and 13% patients died during this period. An 83% of the patients were discharged whereas in 4% patients the outcome was not known. Majority (88.46%) of the patients who died during the hospital stay had Child Pugh C cirrhosis. The hospital stay was uneventful in all the patients with Child Pugh A cirrhosis.
Worsening hepatic encephalopathy was the most common cause of death encountered in 50% of the patients followed by UGI bleed in 26.92% of the patients. An 11.53% of patients died due to sepsis and 7.69% patients due to CLD unrelated causes.
Discussion
In the present study, alcohol was identified as the most common cause of cirrhosis (62.5%) followed by Hepatitis B (11%), cryptogenic (9.5%), NASH (9%) and Hepatitis C (3.5%). We report here that cirrhosis due to wilson’s disease, haemochromatosis and autoimmune hepatitis was found to be 1% each. The susceptibility to develop cirrhosis due to alcohol abuse varies from country to country and the genetic make-up of the patients as shown by the HLA studies in different countries [16-18]. The major aetiological factor in cirrhosis of liver was alcohol followed by cryptogenic or post viral [19]. In contrast, Eun-Kyung H et al., reported HBV related cirrhosis in 73% cases followed by alcohol (6.8%) [20]. In another study, viral aetiology was reported as the most common cause of cirrhosis followed by alcohol [21].
All the clinical presentation in the present study is consistent with those of previous studies [22-24]. The most common observation in the present study is easy fatigability (74.5%) followed by abdominal distention (60%) which is comparable to the reports of Khoonsari M et al., with bloating in 70.4%, morning heaviness in 69.9% and delayed sleep onset in 63.1%of patients [24]. Anorexia is another common presentation among the cirrhotic patients as 49% of our study population showed anorexia while previous studies had reports of 27.2% of the cirrhotic patients presenting with decreased appetite [24].
The most common examination finding in our study was Pallor in 82% of patients followed by splenomegaly in 64%, ascites in 62%, pedal oedema in 44%, icterus in 40%, asterixis in 37%, hepatomegaly in 23% and abdominal tenderness in 15.5% of the patients. This can be compared to many previous study reports [25]. Other physical signs like muscle wasting, abdominal tenderness, umbilical hernia, gynaecomastia, vascular spiders, parotid enlargement, testicular atrophy, dupuytren’s contracture etc can be attributed to the metabolic, endocrinal and circulatory derangements caused by the declining liver function in cirrhosis. The findings of the present study are compared to those of other similar studies [Table/Fig-7] [19-24,26-33].
Comparison of present study with other similar studies [19-33].
| Studies | Place of the study | Commonest aetiology of cirrhosis | Most common clinical presentation | Most common examination findings | Blood picture | Biochemical findings | Radio findings | UGIE picture | Ascitic fluid study | CTP score |
|---|
| Present study | Guwahati, Assam, India | Alcohol 62.5%, HBV (11%), cryptogenic (9.5%), NASH (9%) and HCV (3.5%) | Easy fatiguability (74.5%), abdo distention (60%), anorexia (49%) | Pallor (82%), SplenoMegaly (64%), ascites (62%), pedal oedema (44%), icterus (40%), asterixis (37%), hepatomegaly(23%), abdo tenderness (15.5%) | Mean Hb 8.034 g/dL, Mean Platelet 111700/ uL | Mean serum creatinine 0.92 mg/dL, The venous ammonia level: >20 μmol/L in 76% of the study population, 84.31% of the patients with hepatic encephalopathy had elevated serum ammonia levels. The mean level of serum ammonia in our study was 53.76 μmol/L (SD±50.52). | Abdo USG: splenomegaly (82%), chronic hepatic parenchymal changes (77.5%), ascites (64%), pleural effusion (16.5%) | UG varices (74.5%), Portal hypertensive gastropathy (41%) | >1.1 g/dL serum ascitic albumin gradient (95.3%), Ascitic fluid neutrophil count w >250 cells/ uL (12.5%), Positive ascitic fluid culture report (9.3%), most common organism E. Col (50%) and Klebsiella (33.33%.), Also, positive ascitic fluid for AFB in 2.34% and for malignant cells in 2.34%. | Child Pugh A 6.5% Child Pugh B 41% Child Pugh C 52.5% |
| Mendez-Sanchez N et al., [19] | Maxico | Cryptogenic/Post viral | - | - | - | - | - | - | - | - |
| Eun- Kyung H et al., [20] | Korea | HBV (73%) | - | - | - | - | - | - | - | - |
| Behera A et al., [21] | Cuttack, Odisa, India | Viral | - | - | - | - | - | - | - | - |
| Vijayan M et al., [22] | Kerela, India | - | Abdo pain+oedema+ vomiting (29.7%) | - | - | - | - | - | - | A 11%, B 35%, C 50% |
| Berzigotti A [23] | A review paper published from Switzerland | - | - | - | - | - | - | - | - | - |
| Khoonsari M et al., [24] | Iran | - | Bloating (70%), morning heaviness(69.9%), anorexia (27.2%) | - | - | - | - | - | - | - |
| Sidiq T et al., [26] | Kashmir, India | - | - | - | Mean Hb rural male and female- 7.0912 & 7.242 g/dL and urban male and female- 7.099 & 7.379 g/dL | mean serum creatinine 4.769 mg/dL (male) and 5.46 mg/dL (female) | - | - | - | - |
| AL-Dewachi SO et al., [27] | Mosul, Iraq | - | - | - | Mean Platelet counts 132.6/uL | - | - | - | - | - |
| Zaman A [28] | United States of America | - | - | - | Mean Platelet counts 104.7/uL | - | - | UGI varices (67.66%) | - | - |
| Cioni G et al., [29] | Italy | - | - | - | - | - | Used Duplex Doppler ultrasonography | - | SBP prevalence 3.5% | - |
| Harchand P et al., [30] | Ludhiana, Punjab, India | - | - | - | - | - | - | - | SBP prevalence 51.3%Culture positive 37.9%-Gram neg (77.3%), Gram positive (22.7%).The most common organisms E.Coli (68.1%), Strepto agalactiae (9.09%) and others. | - |
| Filik L et al., [31] | Ankara, Turkey | - | - | - | - | - | - | - | SBP mostly due to Gram neg (76.2%) | - |
| Varghese JS et al., [32] | Chennai, India | - | - | - | - | - | - | - | - | Majority of patients were Child Pugh B |
| Wang X et al., [33] | Southern China | - | - | - | - | - | - | - | - | Majority of patients were Child Pugh B |
The haematological picture of the present study including the mean Haemoglobin level, mean Platelet count and mean Prothrombin level is found to be grossly deranged and is comparable to that of other studies. The present study found a mean Haemoglobin level of 8.034 g/dL (SD±2.395) which is comparable to reports of Sidiq T et al., [26]. In their report, the mean haemoglobin value of rural male and female respondents was found to be 7.0912±1.4507 and 7.242±1.419 and urban male and female respondents 7.099±1.566 and 7.379±1.839, respectively [26]. The Platelet count was found to be 111700/ uL (SD±59.33) in the present study which was comparable to the mean Platelet counts of 132.6 (SD±100.56) and 104.7/ uL (SD±66.5) as reported by AL-Dewachi SO et al., and Zaman A et al., respectively [27,28].
The biochemical findings in our study are consistent with those of Sidiq T et al., and Zaman A et al., [26,28]. The mean Serum albumin, the AST and ALT levels and the serum bilirubin level were shown to be deranged in most of the patients which suggest the declining liver function. The mean serum creatinine was found to be 0.92 mg/dL (SD±0.32) in our study which is comparable to 4.769±8.168 (male) and 5.46±8.61 (female) as reported by Sidiq T et al., [26]. It may be because of the fact that only 4% of our cases had evidence of hepatorenal syndrome. The venous ammonia level was more than 20 μmol/L in 76% of the study population and 84.31% of the patients who had clinical features of hepatic encephalopathy had elevated serum ammonia levels. The mean level of serum ammonia in our study was 53.76 μmol/L (SD± 50.52).
An abdominal ultrasonography has a major role in evaluation of cirrhotic patients. It was done in all the cases of the present study which revealed splenomegaly in 82% cases, chronic hepatic parenchymal changes in 77.5%, ascites in 64% and pleural effusion in 16.5% patients. Cioni G et al., used Duplex-Doppler ultrasonography for the evaluation of cirrhotic patients with portal hypertension and to analyse their response to drugs [29].
In this study, Gastroesophageal varices were found in 74.5% of the patients and portal hypertensive gastropathy in 41%. Only 2% patients showed normal endoscopic reports which are similar to reports of Zaman A et al., showing presence of varices in 67.66% [28]. As a total of 64% patients were detected with ascites either clinically or radiologically, Analysis of the ascitic fluid was performed which showed >1.1 g/ dL serum ascitic albumin gradient (serum albumin- ascitic fluid albumin) in 95.3% patients. The ascitic fluid neutrophil count was more than 250 cells/uL in 12.5% of the patients [9]. A 91.4% patients had an ADA level <39 U/L. A total of 9.3% of the patients gave a positive ascitic fluid culture report, the most common organism being E. Coli in 50% and Klebsiella in 33.33%. Other findings included a positive ascitic fluid for AFB in 2.34% and for malignant cells in 2.34%. The prevalence of SBP varied in different studies from 3.5% Cioni G et al., to 51.3% Harchand P et al., [29,30]. In ascitic fluid culture, Filik L et al., found gram negative organisms to be the most frequently isolated organism (76.2 %) in SBP patients [31]. Harchand P et al., reported that 37.9% SBP cases were culture positive, among which Gram’s negative isolates were more prevalent (77.3%) than Gram’s positive (22.7%) [30]. The most common organisms were Escherichia coli (68.1%), Streptococcus agalactiae (9.09%) and others.
The CTP score was calculated in all the cirrhotic patients. 6.5% of the patients were Child Pugh A, 41% Child Pugh B and 52.5% were Child Pugh C cirrhosis in the present study which was in contrast to Varghese JS et al., and Wang X et al., who reported that majority of their patients were with Child Pugh B cirrhosis [32,33]. It may be due to ignorance and negligence of most of our cirrhotic patients thereby delaying hospital visit in North-East region with advancement of the disease to Child Pugh C.
Limitation
The present study findings were mostly limited to the advanced stage, decompensated liver cirrhosis. The spectrum of complications might have been different if a multi-centric study enrolling patients with initial and compensated stages of cirrhosis would have been performed.
Conclusion
Alcohol is the most common aetiological factor for chronic liver disease followed by Hepatitis B, NASH and Hepatitis C. It is a condition with protean manifestations. Unfortunately, in North East India, patients present in a fairly advanced stage of cirrhosis. The ill effects of alcohol consumption are not taken seriously because the enjoyment of alcohol is socially accepted and even encouraged in many cultures. Gastroesophageal varices, coagulopathy, ascites and hepatic encephalopathy are the most common complications. Spontaneous bacterial peritonitis is fairly common in cirrhotic patients with gram negative organisms E. coli and Klebsiella as the most common causative organisms. Most of the patients die of Hepatic encephalopathy, UGI bleed and septicaemia.
Future recommendation: However, larger studies with long duration follow-up is necessary to throw more light on the exact trend in aetiology, clinical features, complications and causes of death in patients with chronic liver disease.
*NASH: Non alcoholic steato hepatitis