Significance of Cytological Diagnosis in Benign Salivary Gland Lesion
Asif Baliyan1, Ruchi Nagpal2, Harshi Dhingra3, Arnav Kr Roychoudhury4
1 Consultant Pathologist, Department of Pathology, Focus Imaging and Research Centre Pvt. Ltd, Delhi, India.
2 Assistant Professor, Department of Pathology, Bhaskar Medical College and General Hospital, Hyderabad, Telangana, India.
3 Assistant Professor, Department of Pathology, Adesh Institute of Medical Sciences and Research, Bathinda, Punjab, India.
4 Assistant Professor, Department of Pathology, Adesh Institute of Medical Sciences and Research, Bathinda, Punjab, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Ruchi Nagpal, Assistant Professor, Bhaskar Medical College and General Hospital, Yenkapally Moinabad, Hyderabad, Telangana, India.
E-mail: ruchi2001@gmail.com
A diffuse, chronic, non-inflammatory, non-neoplastic usually bilateral, enlargement of major salivary glands is termed as Sialadenosis or sialosis. It is an uncommon cause for enlargement of the parotid gland. We here by describe two patients with history of unilateral painless swelling of parotid glands. Fine-Needle Aspiration (FNA) specimens showed highly cellular smears comprising of clusters of enlarged acini and numerous naked nuclei. A diagnosis consistent with sialadenosis was made. It is important to recognise this underestimated entity cytologically in the work-up of salivary gland swellings to avoid the unnecessarily surgical intervention.
Fine needle aspiration, Parotid gland, Sialadenosis
Case Report
Case 1: A 50-year-old male presented with a swelling in right retroauricular region measuring 2.5×2.0 cm. The swelling was firm, mobile and nontender. It was gradually enlarging in size over a period of two months. The overlying skin was normal and no other swelling was noted on either side. Laboratory tests revealed Random Blood Sugar level (RBS) 220 mg/dL. All the other investigations were within normal limits. Ultrasonography (USG) showed single, well-circumscribed swelling measuring 2×1.8 cm in the right retroauricular region which was suggestive of benign salivary gland lesion.
Case 2: A 20-year-old female presented with a swelling in right infraauricular region measuring 2.0×1.5 cm. The swelling was firm, mobile, nontender and gradually increasing in size since past one month. The overlying skin was normal and no other swelling was noted on either side. The patient was underweight for age and had lean built. Complete blood count showed haemoglobin 9.5 gm/dL, microcytic hypochromic red blood cells with normal total and differential leucocyte count. However, all other routine investigations were within normal limits. USG suggested benign lesion.
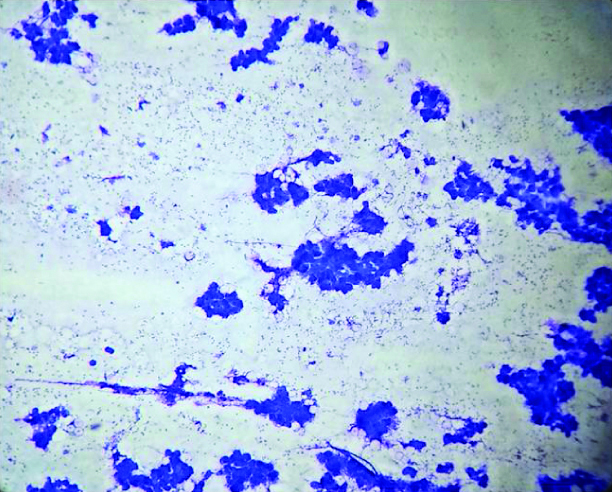
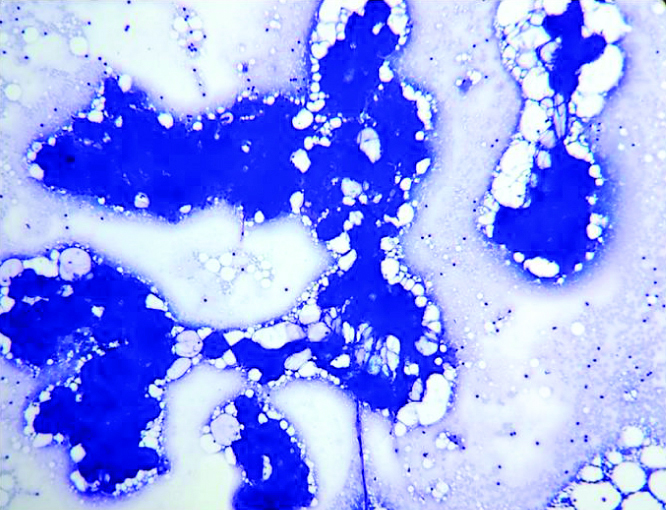
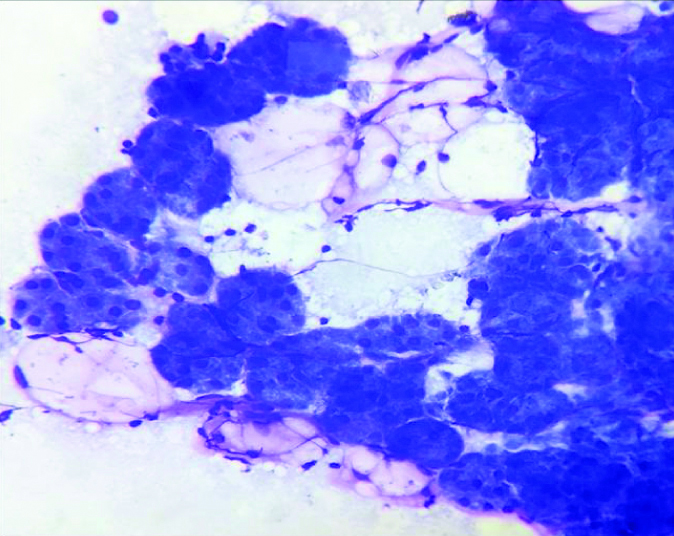
FNAC in both the cases was performed using a 22-gauge needle attached to a 10-mL plastic syringe mounted on a syringe holder for a single hand grip. Blood mixed aspirated material was deposited onto five clean glass slides. FNAC air-dried smears were stained with Giemsa stain and the slides were then examined under a light microscope (Labomed Lx 400) on 4X, 10X, and 40X magnification. Smears prepared from the swelling of both the patients show similar cytological features. Smears were moderately cellular, having acinar epithelial cells arranged in clusters, papillae, and glandular pattern as well as scattered singly [Table/Fig-1]. Within the clusters, acini were extremely crowded and appeared fused [Table/Fig-2]. The acinar cells appeared swollen and exhibit round, small, peripherally located nuclei. The cytoplasm was either vacuolated or finely granular [Table/Fig-3]. Background showed numerous naked epithelial cell nuclei, few adipocytes and red blood cells. Inflammatory cells were not seen in the background. FNA findings were correlated clinically and radiologically, there was no suspicion for any other benign or malignant tumour. Thus, cytological diagnosis of sialadenosis of parotid gland was given in both cases.
Acinar epithelial cells arranged in clusters, papillae, and glandular pattern as well as scattered singly (MGG stain, 10x).
Extremely crowded and fused acini (MGG stain, 10x).
Swollen acinar cells having round, small, peripherally located nuclei with vacuolated or finely granular cytoplasm (MGG stain, 40x).
Discussion
Sialadenosis can be defined as a non-inflammatory, non-neoplastic, symmetrical, soft, painless, persistent enlargement of the parotid glands. It is generally the result of an autonomic neuropathy which results in either excessive stimulation or inhibition of acinar protein secretion and/or synthesis, with secondary cytoplasmic swelling and enlargement of the parotid gland [1]. Sialadenosis does not have a sex predilection and the highest rate of incidence is reported between 30 and 69 years of age [2,3]. A variety of conditions such as alcoholism, endocrine disorders particularly diabetes mellitus, malnutrition, pregnancy, drugs, bulimia, eating disorders have been associated with sialadenosis [4-6]. It is often bilateral and recurrent [7]. But few cases with unilateral sialadenosis were reported as well. Both of our cases had unilateral presentation. Pape SA et al., also reported four cases of unilateral sialadenosis in their case series [7].
Sialadenotic glands diverge from the appearance of normal FNA salivary gland specimens with the presence of high cellularity and the architectural pattern. Another important feature is the marked enlargement of single acini. The cytoplasm is swollen because of a numerical increase of secretory granules and shows either a dark pattern or a clear, vacuolar transformation. Abundant naked nuclei are found due to the extreme delicacy of acinar cytoplasm [1]. Sialadenosis is distinguished from chronic sialadenitis by the abundance of acinar elements, absence of inflammatory cells and proteinaceous debris in the background. Lymphoepithelial Sialadenitis (LESA) is also one of the differentials but sialadenosis lack lymphoepithelial islands and germinal center fragments, which are the characteristic features of LESA [8]. A neoplasic condition that can mimic sialadenosis on cytology is low grade acinic cell tumour. Acinic cell tumours generally yield abundant cellular material with poorly formed microacinar groupings. Naked nuclei are absent in acinic cell tumours whereas these are numerous in sialadenosis. Atypical nuclear features are more prominent in acinic cell tumours as compared to sialadenosis [9]. Another differential is Warthin tumour which also have bilateral presentation. The typical aspirate is composed of lymphocytes, oncocytes, and granular debris, which are not seen in sialadenosis. The non-neoplastic entities such as oncocytosis associated with aging, parotitis, and benign epithelial lesions, which may occur in Acquired Immune Deficiency Syndrome (AIDS) should also be excluded [1,9]. Morphologic characteristics of sialoadenosis are however typical to make the diagnosis. Moreover, oncocytes and inflammatory cells are distinctly absent in sialadenosis [9].
Thus, FNAC is a reliable and minimally invasive diagnostic method with a high sensitivity in the diagnosis of parotid gland lesions. Sensitivity of FNAC for malignant parotid tumours is low because of the deep location. However, 100% accuracy can be achieved if ultrasound guidance is taken [10].
The treatment of sialadenosis is unsatisfactory but the emphasis should be given at the correction of the underlying disorder. In our case, one patient was diabetic and other was malnourished. So no surgical treatment was given, only symptomatic treatments were followed up.
We presented these cases for the rarity of its unilateral presentation and its differentiation on cytology smears from other parotid lesions.
Conclusion
FNAC provides the valuable information for further therapeutic management and is preferred for its high diagnostic accuracy with minimal invasive nature and avoiding unwarranted surgery. It must be emphasised that appropriate clinical history of underlying predisposing diseases is essential in order to establish a correct diagnosis of sialadenosis. However, few cases may be inaccurately diagnosed on cytology due to overlapping features and in these cases histopathology is the only modality for final diagnosis.
[1]. Ascoli V, Albedi FM, De Blasiis R, Nardi F, Sialadenosis of the parotid gland: Report of 4 cases diagnosed by fine-needle aspiration cytologyDiagn Cytopathol 1993 9(2):151-55.10.1002/dc.2840090208 [Google Scholar] [CrossRef]
[2]. Droese M, Cytologic diagnosis of sialadenosis, sialadenitis, and parotid cysts by fine needle aspiration biopsyAdv Otorhinolaryngol 1981 26:49-96.10.1159/0003952907020373 [Google Scholar] [CrossRef] [PubMed]
[3]. Smith WP, Disorders of salivary glands. In: Williams NS, Bulstrode CJ, O’Connell PR, editorsBailey and Love’s Short Practice of Surgery 2013 26th edNew YorkCRC Press:723-40. [Google Scholar]
[4]. Scully C, Bagán JV, Evesan JW, Barnard N, Turner FM, Sialosis: 35 cases of persistent parotid swelling from two countriesBr J Oral Maxillofac Surg 2008 46(6):468-72.10.1016/j.bjoms.2008.01.01418343544 [Google Scholar] [CrossRef] [PubMed]
[5]. Mandel L, Hamele-Bena D, Alcoholic parotid sialdenosisJ Am Dent Assoc 1997 128(10):1411-15.10.14219/jada.archive.1997.00609332142 [Google Scholar] [CrossRef] [PubMed]
[6]. Mignogna MD, Fedele S, Lo Russo L, Anorexia/bulimia-related sialadenosis of palatal minor salivary glandsJ Oral Pathol Med 2004 33(7):441-42.10.1111/j.1600-0714.2004.00208.x15250838 [Google Scholar] [CrossRef] [PubMed]
[7]. Pape SA, MacLeod RI, McLean NR, Soames JV, Sialadenosis of the salivary glandsBr J Plast Surg 1995 48(6):419-22.10.1016/S0007-1226(95)90233-3 [Google Scholar] [CrossRef]
[8]. Cibas Edmund S, Ducatman Barbara S, Cytology: Diagnostic principles and clinical correlates 2014 4th editionPhiladelphia, PAElsevier Inc.:299-322. [Google Scholar]
[9]. Jagtap SV, Aramani SS, Mane A, Bonde V, Sialosis: Cytomorphological significance in the diagnosis of an uncommon entityJ Cytol 2017 34(1):51-52.10.4103/0970-9371.19762028182067 [Google Scholar] [CrossRef] [PubMed]
[10]. Gudmundsson JK, Ajan A, Abtahi J, The accuracy of fine-needle aspiration cytology for diagnosis of parotid gland masses: a clinicopathological study of 114 patientsJ Appl Oral Sci 2016 24(6):561-67.10.1590/1678-77572016021428076460 [Google Scholar] [CrossRef] [PubMed]