Case Report
Case 1
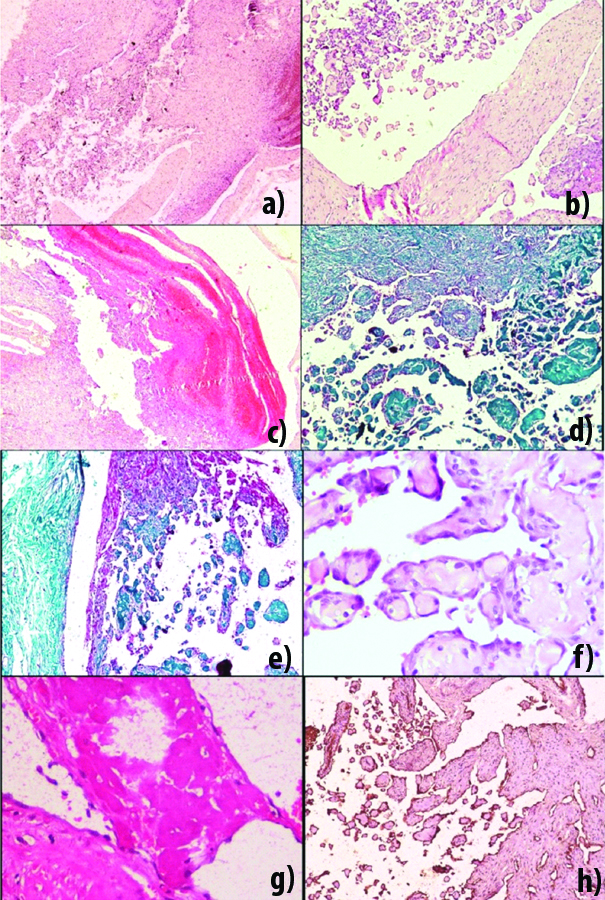
A 25-year-old female presented with slow growing lesion measuring 1×1 cm, on left index finger causing recurrent pain since four months. There were no overlying skin changes. There was history of prior excision of the lesion elsewhere. It was grey white, firm in consistency. On microscopic examination there was a multicystic lesion comprising of thrombus surrounded by smooth muscle. There was ingrowth of endothelial cells along the contours of the thrombus forming small papillae projecting into the lumen. Papillae comprised of collagenised core surrounded by single layer of endothelial cells [Table/Fig-1a-g]. Therewas no evidence of atypia or malignancy. Immunohistochemistry revealed positivity for CD31 [Table/Fig-1h]. It was diagnosed as primary Masson’s tumour. The case was lost to follow-up.
a-c: Section showing papillary structures formed by ingrowth of endothelial cells along the thrombus and with areas of haemorrhage. (4x, 10x, 10x H&E). d,e: Section highlighting fibrin thrombi. (4x,10x, Masson’sTrichrome). f: Section showing high power view of papillary structures lined by endothelial cells. (40x, H&E). g: Section showing high power view of fibrin thrombi. (40x, H&E). h: Section demonstrating CD31 positivity along the lumen and papillary structures. (10x, IHC).
Case 2
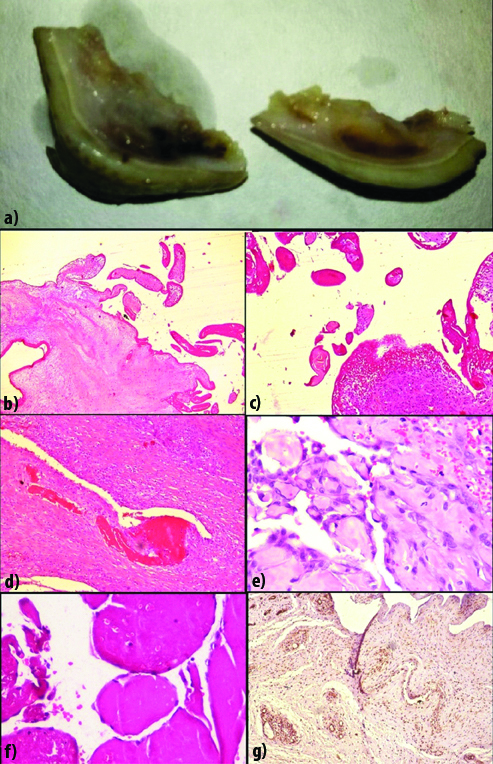
A 30-year-old female presented with swelling over left foot measuring 2×2 cm since 18 months. It was slow growing and painful. There were no overlying skin changes. There was previous history of trauma. Grossly, it was skin covered and firm in consistency. On cut section it was grey white with haemorrhagic and cystic areas [Table/Fig-2a]. Section showed proliferation of numerous capillaries, displacing adjacent normal tissues along with thrombus formation. There was proliferation of endothelial cells along the thrombi giving rise to numerous papillary structures [Table/Fig-2b-f]. The tumour was reaching upto the resected margins; however there was no evidence of atypia or malignancy. Immunohistochemistry revealed positivity for CD 31 [Table/Fig-2g]. Final diagnosis of Masson’s tumour with angiomatosis was rendered (secondary Masson’s tumour). The case was followed up for six months without any recurrence after which the patient did not report back. For both the cases differential diagnoses considered were: arteriovenous malformation, angiomatosis and hamartoma.
a: Gross image showing skin covered lesion with hemorrhagic and cystic areas. b: Section showing capillary and venous channels. (10x, H&E). c: Section showing numerous papillary structures, with capillary proliferation and extravasation of RBCs in periphery. (10x, H&E). d: Section showing fibrin thrombi. (10x, H&E). e: Section showing papillary structures lined by endothelial cells. (40x, H&E). f: Section showing papillary structures formed by fibrin thrombi. (40x, H&E). g: Section showing CD31 positivity.(10x, IHC). CD 31 (Dako, RTU, QBEnd 10, Mouse monoclonal).
Discussion
Masson’s tumour (Intravascular papillary endothelial hyperplasia) is an uncommon benign vascular proliferative lesion occurring in either a normal blood vessel, or vascular malformation. It is characterised by intraluminal papillary proliferation lined by endothelial cells [1-3].
It was first described by Masson in infected haemorrhoidal vessels of a 68-year-old male in 1923. He termed it as it as “Haemagioendotheliomevégétant intra-vasculaire and defined it as a benign neoplasm that overgrows its blood supply leading to necrosis and thrombosis [4].
Subsequently, it was termed as Intravascular Papillary Endothelial Hyperplasia (IPEH) by Clearkin KP et al., [5]. An alternate hypothesis of slowing of blood flow, stasis, and thrombosis providing a matrix for papillary proliferation was suggested. It came to be known as “L’ endovasculite proliferante thrombopoietique”, or Masson’s intravascular vegetant haemangioendothelioma [5].
Subsequent researchers concluded that this entity is a vascular proliferative reaction usually after traumatic vascular stasis, and not a true neoplasm. This hypothesis of local disturbed haemodynamics, inducing progression of thrombus formation, with subsequent endothelial proliferation, has been widely accepted. The term IPEH, first used by Clearkin and Enzinger in 1976, is preferred instead of the misleading definition of Masson’s pseudoangiosarcoma [6-9].
Levere SM et al., however, proposed an autocrine etiology of post-traumatic IPEH, involving the Fibroblast Growth Factor (FGF) secretion. The macrophages that reach the site of trauma release the FGF, which triggers IPEH; the endothelial proliferating cells, on their turn, release more FGF, thus activating a positive feedback loop of endothelial proliferation [10]. Contribution of minor trauma has been highlighted in their pathogenesis in 4% of the cases [11]. It accounts for approximately 2% of vascular tumours of skin and subcutaneous tissues and may mimic sarcomas and be a cause of concern [2,6,7].
It is likely that many more IPEH exist but are diagnosed as organising thrombi [2]. The largest series were reported by Clearkin KP et al., followed by Hashimoto H et al., [5,8].
Subsequently, there have been sporadic case reports or small case series [Table/Fig-3] [1-3,5-23]. Unfortunately, there are no specific radiological features, which characterise IPEH/Masson’s tumour as a result; it is usually diagnosed after being removed surgically as another mass lesion [15].
Summary of previously published cases of Masson’s tumour [1-3,5-23].
| S. No. | Authors | No. of cases | Year | Age/Sex | Site | Features | Follow-up | IHC | Primary/Secondary |
|---|
| 1. | Cleakin KP et al., [5] | 44 | 1976 | N/A | 14: subcutis of fingers, 10: head and neck, 7: trunk. | Sarcoma like microscopic appearance in few cases. | 31 cases had benign clinical course | N/A | N/A |
| 2. | Hashimoto H et al., [8] | 91 | 1983 | N/A | 14: subcutis of fingers, 7: head and neck, 6: between elbows and hands | N/A | N/A | N/A | 30-pure 55-mixed 6-others |
| 3. | Tosios et al., [2] | 18 | 1994 | N/A | Oral (lip, buccal mucosa, tongue, angle of mouth, mandibular vestibule) | N/A | N/A | N/A | N/A |
| 4. | Levere et al., [10] | N/A | 1994 | N/A | Extremities | N/A | N/A | N/A | N/A |
| 5. | Moon WS et al., [19] | 1 | 2000 | 35/M | Ethmoid sinus | Erosion of cribriform plate, adhesion to dura. | No recurrence, followed upto 9 months. | Endothelial, CD 34, Factor VIII related antigen | Primary |
| 6. | Makos CP et al., [23] | 2 | 2004 | 45/M, 31/F | Lip, Buccal mucosa | | No recurrence followed upto 2 years. No recurrence, followed upto 6 years. | ULE X Europ aeus Agglu tinin (UEA-1) | Both Primary |
| 7. | Korkolis DP et al., [6] | 1 | 2005 | 60/M | Thigh | Presentation of soft tissue sarcoma radiologically. | No recurrence, followed upto 15 months. | N/A | Secondary |
| 8. | Jazaerly T et al., [20] | 1 | 2011 | 77/M | Bladder | Post irradiation for prostatic adenocarcinoma. | No recurrence, followed upto 1 year. | N/A | Secondary |
| 9. | Park KK et al., [15] | 1 | 2012 | 10/F | Skull | No history of trauma. | No recurrence, followed upto 8 months. | CD31, Vime ntin, weekl y positi ve for CD34 and CK, | Primary |
| 10. | Mokhtari M et al., [17] | 1 | 2012 | 39/M | Parotid | Atheroscleros is with superimposed thrombus. | N/A | N/A | Secondary |
| 11. | Akdur NC et al., [3] | 10 | 2013 | 21-71 years; 3 Males, and 7 Females | 5 upper extremity, 5 head and neck | 6 cases with associated organised thrombus. | | CD31, CD34, Factor VIII relate d antige n | N/A |
| 12. | Gill M et al., [18] | 1 | 2014 | 47/M | Scapula | No history of trauma. | No recurrence till date. | CD 34 | Primary |
| 13. | Sarode GS et al., [21] | 1 | 2015 | 54/F | Oral | History of trauma | No recurrence, followed upto 1 year. | N/A | Secondary |
| 14. | Breccia M et al., [13] | 1 | 2015 | 22/M | Foot | Large size, uncommon location, no h/o trauma. | No recurrence, followed upto 9 months. | CD 31, CD34, FL11. | Primary |
| 15.. | Al Qahtani KH [1]. | 1 | 2016 | 33/F | Nasal cavity | Extending into paranasal sinuses with pressure erosion of surrounding bones. | No recurrence, followed upto 4 years. | N/A | Primary |
| 16. | de Castro MS et al., [9] | 1 | 2016 | 53/M | Buccal mucosa | Slow growing. | No recurrence till date. | CD 34, Vime ntin, Glut- 1, lamini n | Primary |
| 17. | Fernandes D et al., [14] | 1 | 2016 | 76/F | Oral | Varices in legs and feet. | No recurrence, followed upto 6 months. | CD 34. | Secondary |
| 18. | Boukovalas S et al., [7] | 1 | 2017 | 64/M | Forehead | History of trauma, pulsatile mass. | No recurrence, followed upto 5 months. | N/A | Primary (despite history of trauma). |
| 19. | Liné A et al., [22] | N/A | 2017 | 2-6 years | Abdominal muscle, metatarsal, thigh, axilla | Paediatric cases. | N/A | N/A | N/A |
| 20. | Pountos I et al., [11] | 1 | 2018 | 22/F | Knee | History of trauma. | Recurrence after 2 years. | N/A | Secondary |
| 21. | Kakhandaki A et al., [12] | 1 | 2018 | 58/M | Orbit | No history of trauma. | No recurrence, followed upto 20 weeks. | N/A | Primary |
| 22. | Pesce V et al., [16] | 1 | 2018 | 61/M | Hand | No history of trauma, radiologically hemangioperi-cytoma. | No recurrence, followed upto 6 months. | N/A | Primary |
Hyperintense, with a low-signal internal septation and some hypointense areas reflecting thrombotic or haemorrhagic material are suggestive features on MRI [16]. The age of presentation varies from 26 to 60 years with a mean age of 42.6 years to even as young as 9 months. It is more common in females [6,22,23]. It usually occurs in skin as a subcutaneous tissue of fingers, trunk, head and neck, but has also been reported in unusual locations in scapula, oral cavity, heart, larynx, urinary bladder, orbit, skull and hypopharynx [1-20]. Foot is a very uncommon presentation and the present case qualifies for a rare large unusual location unlike smaller lesion reported by Breccia M et al., [13].
Three different forms of Masson’s tumour have been reported: a) Primary/pure form in normal preexisting dilated vessels: this form is seen more commonly in distal extremities; b) Secondary/mixed form in pre-existing vascular lesion like haemangiomas, varices, pyogenic granulomas, or arteriovenous malformations; c) Uncommon Extravascular form, possibly arising in a haematoma [8]. The pure form is more common than the mixed, and usually originates within veins rather than arteries [2]. Primary type (74.42%) was more common than the secondary (24.03%) and extra-vascular (1.55%) forms in literature review [9,21].
Our Case 1 and Case 2 were categorised as primary and secondary Masson’s tumours, respectively. Masson’s tumour commonly presents as firm or tender nodule/mass with slight elevation, sharp demarcation and red or blue colour of the overlying skin [23]. At other location the lesion may mimic sarcomas or even eosinophilic granuloma [15].
Histopathologically, it is characterised by small papillary structures with delicate stromal stalks, usually lined by single layer of hyperplastic endothelial cells that bulge into a vascular lumen [5,13]. Papillary formation, anastomosing vascular channels and plump endothelial cells can simulate angiosarcoma [17]. Features in favour of Masson’s tumour are circumscribed lesion, intraluminal lesion origin one or two covering layer of endothelial cells with less commonly pilling up, hyaline core of papillae, close association with organising thrombus absence of irregular or intertwining capillaries minimal necrosis, lack of pleomorphism and mitotic activity [2,3,5,13,23].
Immunohistochemistry is helpful to demonstrate the vascular origin and low proliferative index. On immunohistochemistry, CD31 and CD34 stain endothelium of Masson’s tumour with a high intensity and thus can be used to establish the vascular origin of the lesion. Both immature endothelium and mature well-formed vessels stain diffuse strongly with CD31 and CD34. Factor VIII related antigen positivity is a strong indicator of Masson’s tumour though there is maturity-based variation in staining with only mature lesions showing the positivity. Markers for basement membrane and pericytes associated with vascular proliferations likeType 4 collagen, SMA (Smooth Muscle Actin) and MSA (Muscle Specific Actin) show variable staining depending on stage of development of the lesion [3]. These can be utilised in distinguishing IPEH from angiosarcoma Kaposi’s sarcoma, and angiolymphoid hyperplasia [11].
CD 105 or endoglin, a transmembrane protein, has an important role in angiogenesis and is essential for the endothelial cell proliferation during the active phase of angiogenesis. Its expression is a salient feature of newly formed blood vessels but is minimally expressed in fully formed vessels. This can be utilised in identification of blood vessels surrounding IPEH lesions in extravascular locations. IPEH tissues are unlikely to be comprised of proliferative angiogenic tissues; whereas CD 105 is over expressed only in angiosarcoma associated endothelial cells [2]. It is essential to differentiate Masson’s tumour from angiosarcoma as latter is malignant with metastatic potential [3].
Its biological behaviour can be predicted by use of proliferation markers e.g., Ki67 (<10% usually). Although the lesion is benign but the chances of recurrence can be predicted using this marker [9]. No cases of malignant transformation have been reported till 2017 [7].
Expression of GLUT-1 can also be used to differentiate between juvenile haemangiomas and other oral benign vascular lesions [9].
Clinically, it can be mistaken for a wide range of diagnosis e.g., mucocele, haemangioma, lymphangioma, haematoma, Kaposi sarcoma, haemangioendothelioma, thrombosed vein, traumatic fibroma, pyogenic granuloma, angiosarcoma and salivary gland tumour and need to be identified with utmost care judiciously utilising IHC to avoid misdiagnosis [7,17,21].
Masson’s tumour usually presents as slow growing mass that can be cure by wide local excision. Incomplete excision can lead to recurrence. IPEH has known to act aggressively, in that it generally recurs when incompletely resected [15]. Use of sclerotherapy before surgery has been suggested to minimise intraoperative bleeding [21].
Conclusion
Accurate diagnosis is essential because although benign, it presents as a mass lesion and can mimic several other lesions like angiosarcoma. It also has the potential of being missed as pyogenic granuloma or even haemangioma. Hence, histopathological examination with IHC as an adjunct is mandatory to confirm the diagnosis and prevent aggressive treatment or under treatment.
[1]. Al-Qahtani KH, Intravascular papillary endothelial hyperplasia (Masson’s tumour) as a nasal mass: A case report and review of the literaturePan Arab J Rhinol 2016 6:33-35.10.4103/2090-7540.183731 [Google Scholar] [CrossRef]
[2]. Tosios K, Koutlas IG, Papanikolaou SI, Intravascular papillary hyperplasia of the oral soft tissues: Report of 18 cases and review of the literatureJ Oral Maxillofacial Surg 1994 52:1263-68.10.1016/0278-2391(94)90048-5 [Google Scholar] [CrossRef]
[3]. Akdur NC, Donmez M, Gozel S, Ustun H, Hucumenoglu S, Intravascular papillary endothelial hyperplasia: Histomorphological and immunohistochemical featuresDiagnPathol 2013 8:16710.1186/1746-1596-8-16724125024 [Google Scholar] [CrossRef] [PubMed]
[4]. Masson MP, Hémangioendothéliomevégétant intra-vasculaireBull MemSocAnat Paris 1923 93:517-23. [Google Scholar]
[5]. Clearkin KP, Enzinger FM, Intravascular papillary endothelial hyperplasiaArch Pathol Lab Med 1976 100:441-44. [Google Scholar]
[6]. Korkolis DP, Papaevangelou M, Koulaxouzidis G, Zirganos N, Psichogiou H, Vassilopoulos PP, Intravascular papillary endothelial hyperplasia (Masson’s haemangioma) presenting as a soft-tissue sarcomaAnticancer Res 2005 25:1409-12. [Google Scholar]
[7]. Boukovalas S, Dillard R, Qiu S, Cole EL, Intravascular papillary endothelial hyperplasia (Masson’s tumour): Diagnosis the plastic surgeon should be aware ofPlastReconstrSurg Glob Open 2017 5:e112210.1097/GOX.000000000000112228203491 [Google Scholar] [CrossRef] [PubMed]
[8]. Hashimoto H, Daimaru Y, Enjoji M, Intravascular papillary endothelial hyperplasia. A clinicopathologic study of 91 casesAm J Dermatopathol 1983 5:539-46.10.1097/00000372-198312000-00004 [Google Scholar] [CrossRef]
[9]. de Castro MS, de Carli ML, Giudice FS, de Sousa SCOM, Pereira AAC, Hanemann JAC, Oral intravascular papillary endothelial hyperplasia: Case report and review of literatureJ Oral MaxillofacSurg Med Pathol 2017 29:173-79.10.1016/j.ajoms.2016.08.001 [Google Scholar] [CrossRef]
[10]. Levere SM, Barsky SH, Meals RA, Intravascular papillary endothelial hyperplasia: A neoplastic ‘actor’ representing an exaggerated attempt at recanalization mediated by basic fibroblast growth factorJ Hand Surg Am 1994 19:559-64.10.1016/0363-5023(94)90256-9 [Google Scholar] [CrossRef]
[11]. Pountos I, Siddiqui A, Intravascular papillary endothelial hyperplasia (Masson’s tumour) involving the knee synoviumJ Orthop Case Rep 2018 8:23-25. [Google Scholar]
[12]. Kakhandaki A, Dinesh US, Akash B, Intravascular Papillary Endothelial Hyperplasia as an unusual diagnosis for peri-orbital tumour- A case reportIndian J Ophthalmol 2018 66:163-65.10.4103/ijo.IJO_645_1729283152 [Google Scholar] [CrossRef] [PubMed]
[13]. Breccia M, Novello M, Galli M, Coli A, Unusual presentation of intravascular papillary endothelial hyperplasia (Masson’s tumour)Hum Pathol 2015 2(1):16-19.10.1016/j.ehpc.2014.11.009 [Google Scholar] [CrossRef]
[14]. Fernandes D, Travassos CD, Ferrisse TM, Massucato EMS, Navarro CM, Onofre MA, Oral Intravascular papillary endothelial hyperplasia associated with an organizing thrombus: case report and immunohistochemical analysisCase Reports in Pathology 2016 2016:1908767https://doi.org/10.1155/2016/190876710.1155/2016/190876728053797 [Google Scholar] [CrossRef] [PubMed]
[15]. Park KK, Won YS, Yang JY, Choi CS, Han KY, Intravascular Papillary Endothelial Hyperplasia (Masson tumour) of the Skull: Case Report and Literature ReviewJ Korean Neurosurg Soc 2012 52:52-54.10.3340/jkns.2012.52.1.5222993679 [Google Scholar] [CrossRef] [PubMed]
[16]. Pesce V, Bizzoca D, Notarnicola A, Piazzolla A, Vicenti G, Cimmino A, An intravascular papillary endothelial hyperplasia of the hand radiologically mimicking a haemangiopericytoma: A case report and literature reviewSAGE Open Med Case Rep 2018 6:1-4.10.1177/2050313X1775285129348916 [Google Scholar] [CrossRef] [PubMed]
[17]. Mokhtari M, Azarpira N, Rasolmali R, Intravascular papillary endothelial hyperplasia (Masson’s tumour) of the parotid glandIndian J PatholMicrobiol 2011 54:226-28.10.4103/0377-4929.7742321393933 [Google Scholar] [CrossRef] [PubMed]
[18]. Gill M, Batra A, Jain D, Gupta V, Sen R, Gupta S, Intravascular papillary endothelial hyperplasia (Masson’s Haemangioma) presenting as soft tissue mass in left scapular region-an unusual presentationJ Interdiscipl Histopathol 2014 2(3):179-83.10.5455/jihp.20140312051546 [Google Scholar] [CrossRef]
[19]. Moon WS, Chung GH, Hong KH, Intravascular papillary endothelial hyperplasia in a vascular lesion of the paranasal sinusArch Pathol Lab Med 2000 124:1224-27. [Google Scholar]
[20]. Jazaerly T, Jaratli H, Sakr W, Almardini N, Urabi M, Dhar N, Intravascular papillary endothelial hyperplasia of the bladder: Case report and review of the literatureAvicenna J Med 2011 1:55-57.10.4103/2231-0770.9091723210010 [Google Scholar] [CrossRef] [PubMed]
[21]. Sarode GS, Sarode SC, Extra-vascular type of oral intravascular papillary endothelial hyperplasia (Masson’s tumour) of lower lip: A case report and review of the literatureIndian J Dent Res 2015 26:101-05.10.4103/0970-9290.15682525961626 [Google Scholar] [CrossRef] [PubMed]
[22]. Liné A, Sanchez J, Jayyosi L, Birembaut P, Ohl X, Poli-Mérol ML, François C, Papillary endothelial hyperplasia (Masson’s tumour) in childrenAnn Chir Plast Esthet 2017 62(3):232-37.10.1016/j.anplas.2016.05.01027346753 [Google Scholar] [CrossRef] [PubMed]
[23]. Makos CP, Nikolaidou AJ, Intravascular papillary endothelial hyperplasia (Masson’s tumour) of the oral mucosa. Presentation of two cases and reviewOral Oncol EXTRA 2004 40:59-62.10.1016/j.ooe.2003.11.001 [Google Scholar] [CrossRef]