The lung is a unique organ because it has direct and constant exposure to the surrounding atmosphere [1]. The pathologic and toxicological findings can often be correlated with the specific circumstances of the terminal event [2]. Their correlations in forensic scientific investigations form an important component of the investigator’s skills [2]. Hence, the interpretation of postmortem findings may assist in illuminating the circumstances of death [2]. An autopsy, self-study of a dead body, is carried out for medical as well as medico-legal purposes [3]. It is a method to detect diagnostic errors, understand limitations of therapy, a useful source of knowledge in future cases, influencing the data on local epidemiology of diseases and quality control for technical investigations [4,5].
The World Health Organisation has predicted that traffic fatalities are going to be the sixth leading reason behind death worldwide and also the second leading reason behind disability-adjusted life-years lost in developing countries by the year 2020 [6,7]. The main causes of death in RTA autopsies were lung injuries, bronchopneumonia and undiagnosed chest infections [6]. Respiratory dysfunction after burns is multi-factorial, where Acute Respiratory Distress Syndrome (ARDS) and inhalation injuries are the most important [8]. Medicolegal poison cases are usually suicidal and rarely accidental [9].
Organ-specific pathological changes, seen during the autopsy, give a richer picture of the cause of death and help to recreate the clinical scenario on what went wrong. Pulmonary pathological alterations seen at autopsy remain a relatively unstudied domain of forensic pathology and hence the need for such a study. The objectives of this study were to study the histomorphological lung changes seen at autopsy and to correlate the clinical cause of death with the pathological findings.
Materials and Methods
This was a prospective study in which bilateral lung specimens were collected from 120 medicolegal autopsies performed at a tertiary care hospital in coordination with the Department of Forensic Medicine during a two-year period. Relevant clinical data like age, clinical diagnosis, relevant medical history and cause of death was obtained in each case. Each autopsy subject was identified, examined and a post-mortem examination was done after obtaining requisition from the police and consent from the next of kin. Both the lungs were weighed with the pleura and dimensions were noted. In a few cases, only one lung was received. The lungs were fixed by the wet inflation fixation method (10% buffered formalin) [10].
The following autopsies were excluded: Autopsies on poorly preserved bodies that were more than three days old where autolytic changes would have taken place, perinatal deaths, and infants under one year. Approval from the Institute Ethics Committee (IEC no. DMC/KLR/MEU/IEC-CER/225/2011-12), was obtained to conduct this study.
Lungs and pleura were examined for gross morphological changes like collapse, inflation, consolidations, and scarring. For the histomorphological study, two bits each of 1 cm thickness were taken from each lobe of both lungs amounting to 10 bits and each bit labelled. One bit from the bronchus of either side was also taken and labelled. Additional bits were taken from pathological lesions wherever necessary. These bits were fixed in 10% formalin and subjected to routine tissue processing. Paraffin-embedded tissue sections were then stained for routine haematoxylin and eosin stain.
The sections were examined for congestion, oedema, haemorrhage, inflammation, alveolar collapse and/or thinning, alveolar wall disturbances, Diffuse Alveolar Damage (DAD), capillary dilatation, haemosiderotic changes, anthracotic changes, bronchial changes, bronchiolar and pulmonary vessel pathologies or any other changes if any. Special stains like PAS stain, Gram’s stain, and Ziehl-Neelsen Stain were done wherever micro-organisms were seen.
Statistical Analysis
Descriptive data were summarised by frequencies and percentages for categorical variables using SPSS IBM software Version 22.0.
Results
The mean (range) age of the patients in this study was 36.25±15.71 years (8 to 85 years). Majority of patients belonged to the 3rd decade (27%), followed by the 5th decade (20%) and 4th decade (17%) [Table/Fig-1]. The number of males and females was 85 (71%) and 35 (29%) respectively with a male to female ratio of 2.4:1 [Table/Fig-2,3].
Cause of death and age distribution.
| Clinical cause of death | Age groups (years) | Total |
|---|
| 0-9 | 10-19 | 20-29 | 30-39 | 40-49 | 50-59 | 60-69 | >70 |
|---|
| RTA | 2 | 1 | 16 | 9 | 16 | 8 | 1 | 0 | 53 |
| Poisoning | 0 | 11 | 11 | 8 | 4 | 3 | 6 | 1 | 44 |
| Drug anaphylaxis | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 |
| Alcohol intoxication | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 1 |
| Snake bite | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 2 |
| Burns | 0 | 1 | 1 | 2 | 2 | 1 | 1 | 0 | 8 |
| Uterine rupture | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 |
| Sudden death | 0 | 0 | 1 | 0 | 0 | 3 | 0 | 0 | 4 |
| Suicidal cut throat | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 |
| Fall from height | 0 | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 2 |
| Hypertensive encephalopathy | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 1 |
| Sandblaster fall | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 1 |
| Natural death | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 1 |
| Total | 2 | 14 | 32 | 20 | 24 | 17 | 9 | 2 | 120 |
Cause of death and gender distribution.
| Cause of death | Gender | Total |
|---|
| Male | Female |
|---|
| RTA | 48 | 5 | 53 |
| Poison | 26 | 18 | 44 |
| Drug anaphylaxis | 1 | 0 | 1 |
| Alcohol intoxication | 1 | 0 | 1 |
| Snake bite | 1 | 1 | 2 |
| Burns | 0 | 8 | 8 |
| Uterine rupture | 0 | 1 | 1 |
| Sudden death | 3 | 1 | 4 |
| Suicidal cut throat | 1 | 0 | 1 |
| Fall from height | 1 | 1 | 2 |
| Hypertensive encephalopathy | 1 | 0 | 1 |
| Sandblaster fall | 1 | 0 | 1 |
| Natural death | 1 | 0 | 1 |
| Total | 85 | 35 | 120 |
Age and gender distribution.
| Age group (years) | Male | Female | Total |
|---|
| 0-9 | 0 | 2 | 2 |
| 10-19 | 10 | 4 | 14 |
| 20-29 | 24 | 8 | 32 |
| 30-39 | 12 | 8 | 20 |
| 40-49 | 21 | 3 | 24 |
| 50-59 | 13 | 4 | 17 |
| 60-69 | 4 | 5 | 9 |
| >70 | 1 | 1 | 2 |
| Total | 85 | 35 | 120 |
The most common cause of death was RTAs (53 cases, 44%), followed by poisoning (44 cases, 36%) and burns (8 cases, 7%). The other rare causes included sudden death, snake bites, drug anaphylaxis, alcohol intoxication, uterine rupture, suicidal cut throat and fall from height. Maximum cases of RTAs were seen in the third decade (30%) and fifth decade (30%) [Table/Fig-1]. Maximum victims of RTAs were males (90%). The highest frequency of poisoning was seen in the second decade (25%) and third decade (25%) and more common among men (60% of poison cases). All burns victims were females. The most frequent manner of deaths was accidents (49%), followed by suicides (45%) and sudden deaths (3%).
Out of 120 autopsy cases, right lungs were studied in 116 and left lungs were studied in 111.
The mean (range) weight of the right lung in males was 425.56±135.09 gm (120 to 1200 gm) and that in females was 410±99.41 gm (150 to 700 gm). The mean (range) weight of the left lung in males was 376.6±111.32 gm (100 to 900 gm) and that in females was 387.1±87.06 gm (140 to 600 gm). 2% of the right and left lung cases had thickened pleura. The [Table/Fig-4] enumerates all the histological features in autopsy cases. On gross examination of the external surface and cut section of the right lungs, it was found that 41 had anthracotic changes, 28 had grey-white consolidated areas, eight had emphysematous changes including bullae [Table/Fig-5], three had bronchiectatic changes, two had thromboembolus in the pulmonary artery and its branches [Table/Fig-6], two had absence of the right horizontal fissure [Table/Fig-7], and remaining were unremarkable.
| S. No. | Feature | Right lung | Rt lung (%) | Left lung | Lt lung (%) |
|---|
| 1 | Pulmonary congestion | 91 | 77.7 | 82 | 73.8 |
| 2 | Alveolar haemorrhage | 44 | 37.6 | 44 | 39.6 |
| 3 | Pulmonary oedema | 55 | 47 | 53 | 47.7 |
| 4 | Haemosiderosis | 16 | 32.5 | 17 | 34.2 |
| 5 | Diffuse alveolar damage | 16 | 13.6 | 15 | 13.5 |
| 6 | Regional alveolar damage | 6 | 5.1 | 2 | 1.8 |
| 7 | Pneumonia changes | 15 | 12.8 | 15 | 13.5 |
| 8 | Thromboembolus | 2 | 1.7 | 2 | 1.8 |
| 9 | Emphysematous changes | 14 | 12 | 16 | 14 |
| 10 | Pulmonary vessel thickening | 16 | 13.6 | 12 | 10.8 |
| 11 | Bronchiolar dilatation | 10 | 8.5 | 6 | 5.4 |
| 12 | Bacteria-cocci, Bacilli | 8 | 6.8 | 4 | 3.6 |
| 13 | Bronchiolitis with starch/vegetable matter | 4 | 3.4 | 1 | 1 |
| 14 | Acute bronchiolitis | 11 | 9 | 8 | 7 |
| 15 | Interstitial fibrosis | 3 | 2.5 | 0 | 0 |
| 16 | Bronchial congestion | 68 | 58 | 67 | 60 |
| 17 | Squamous metaplasia | 3 | 2.5 | 0 | 0 |
| 18 | Raised reid’s index | 4 | 3.4 | 6 | 5.4 |
| 19 | Bronchitis changes | 3 | 2.5 | 4 | 3.6 |
Gross photograph depicting an emphysematous bulla (arrow) in the upper lobe.
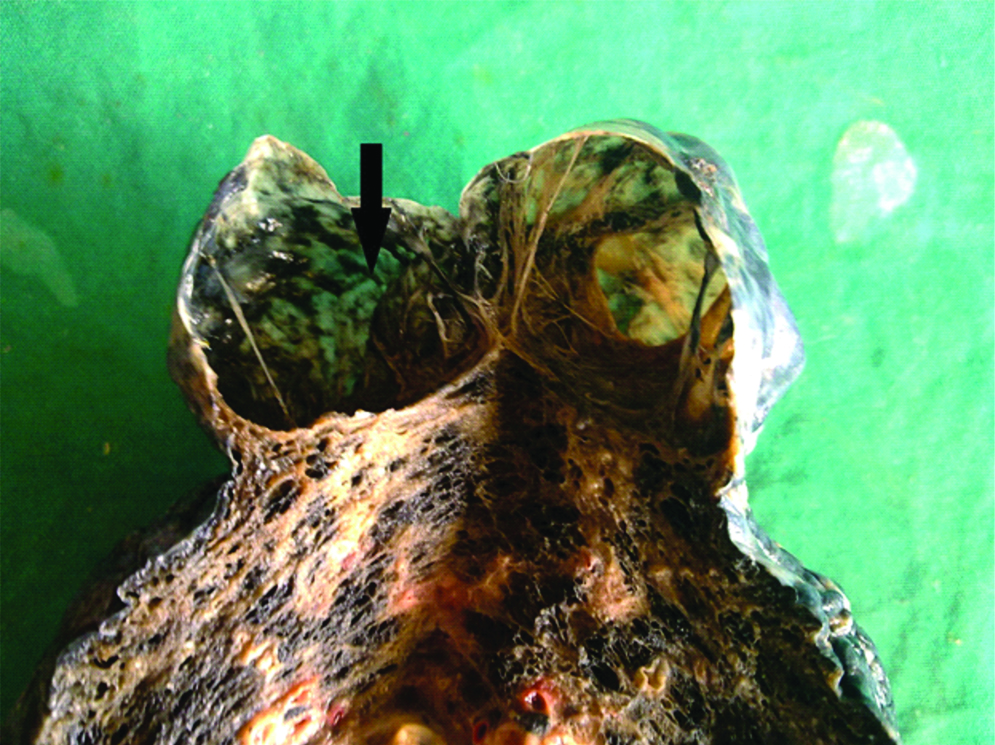
Gross photograph showing a thromboembolus (arrow) in the pulmonary artery.

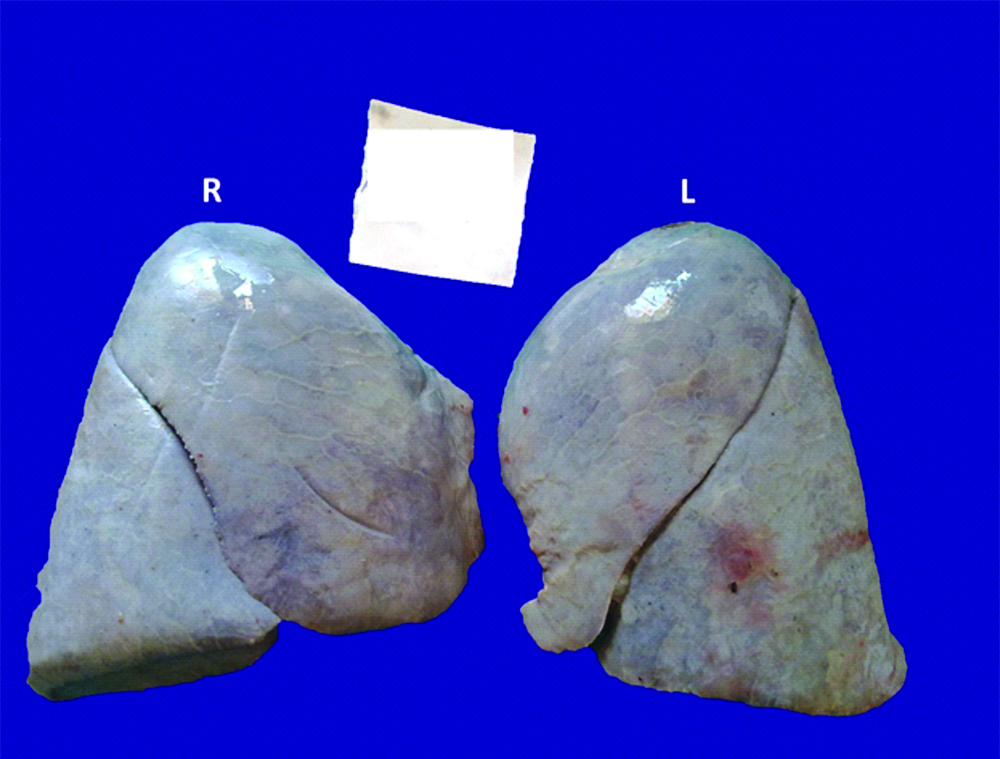
Gross photograph showing absent horizontal fissure in the right lung.
On gross examination of the external surface and cut section of the left lungs, it was found that 40 had anthracotic changes, 23 had grey-white consolidated areas, six had emphysematous changes including bullae, two had bronchiectatic changes, two had thromboembolus in the pulmonary artery and its branches, one had lacerations in the lower lobe, and remaining were unremarkable.
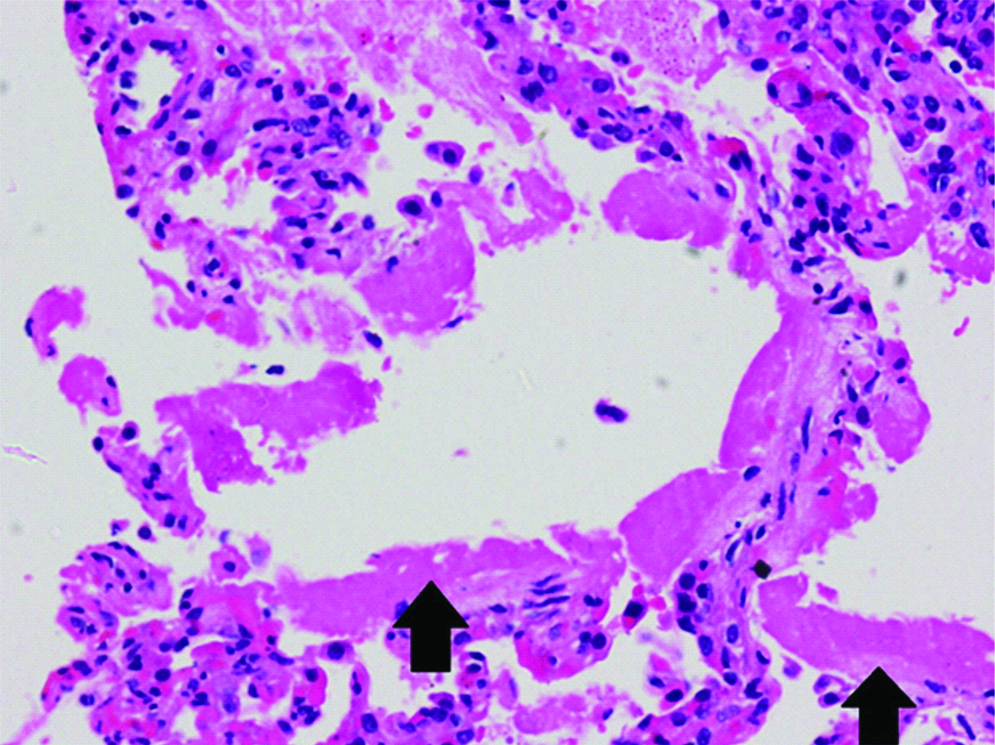
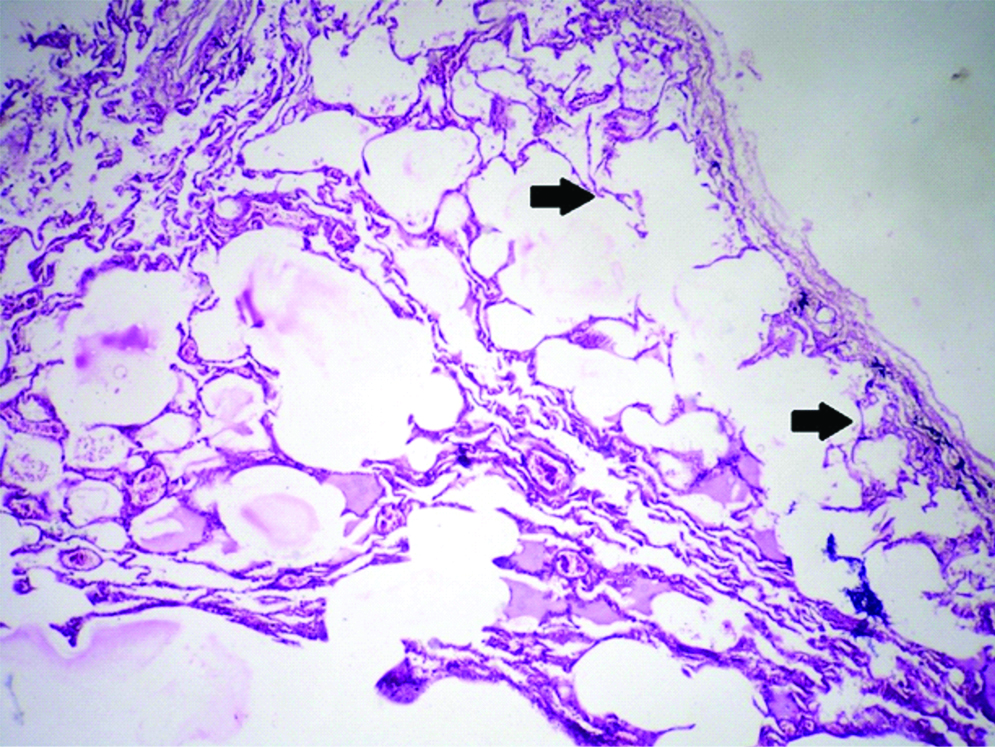
On microscopy [Table/Fig-4], the majority of cases had pulmonary congestion (77.7%), followed by bronchial congestion, anthracosis, pulmonary oedema (47.7%) [Table/Fig-8], and alveolar haemorrhage (39.6%) [Table/Fig-9]. DAD [Table/Fig-10] was seen in 13.5% of right and left lungs each. Regional Alveolar Damage (RAD) was seen in 5% of right lungs and 2% of left lungs. Pneumonia was observed in 13% of right lungs and 13.5% of left lungs. Acute bronchiolitis was seen in 9% of the right lungs and 7% of left lungs. The main histological findings seen in RTA cases were pulmonary congestion, pulmonary oedema, alveolar haemorrhage, haemosiderotic changes, and coincidental obstructive pulmonary disease changes [Table/Fig-11]. DAD was seen in 5.5% of right and left lungs each. RAD was seen in 7.5% of right lungs and 4% of the left lungs. Acute bronchiolitis was observed in 4% of cases.
Photomicrograph showing oedematous fluid (black arrow) within the alveolar spaces in pulmonary oedema (H&E; X100).
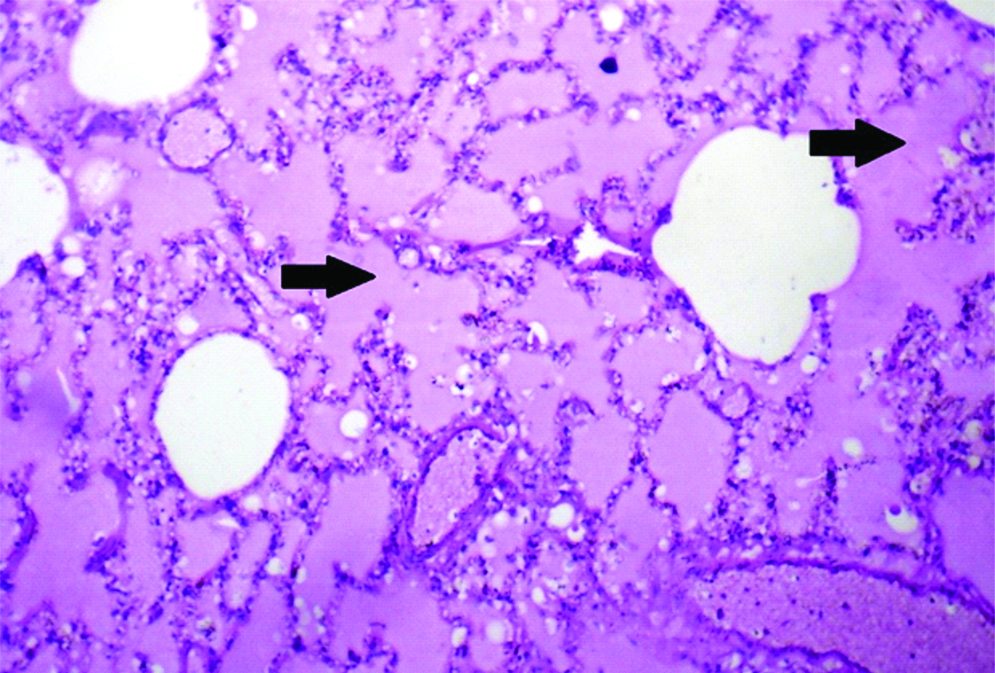
Photomicrograph showing haemorrhage (black arrow) within the alveolar spaces in intra-alveolar haemorrhage (H&E; X100).
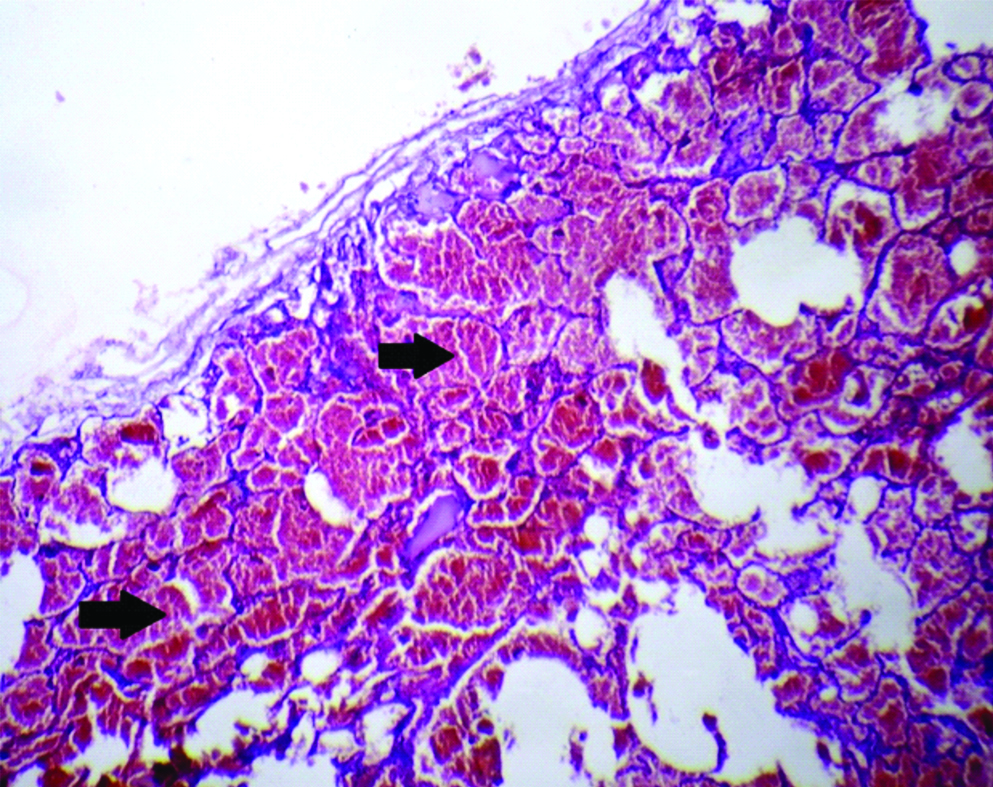
Photomicrograph showing dense eosinophilic hyaline membrane (black arrow) in diffuse alveolar damage (H&E; X 200).
Photomicrograph showing features of thinned out and broken alveolar septae (black arrow) in emphysema with focal pulmonary oedema (H&E; X100).
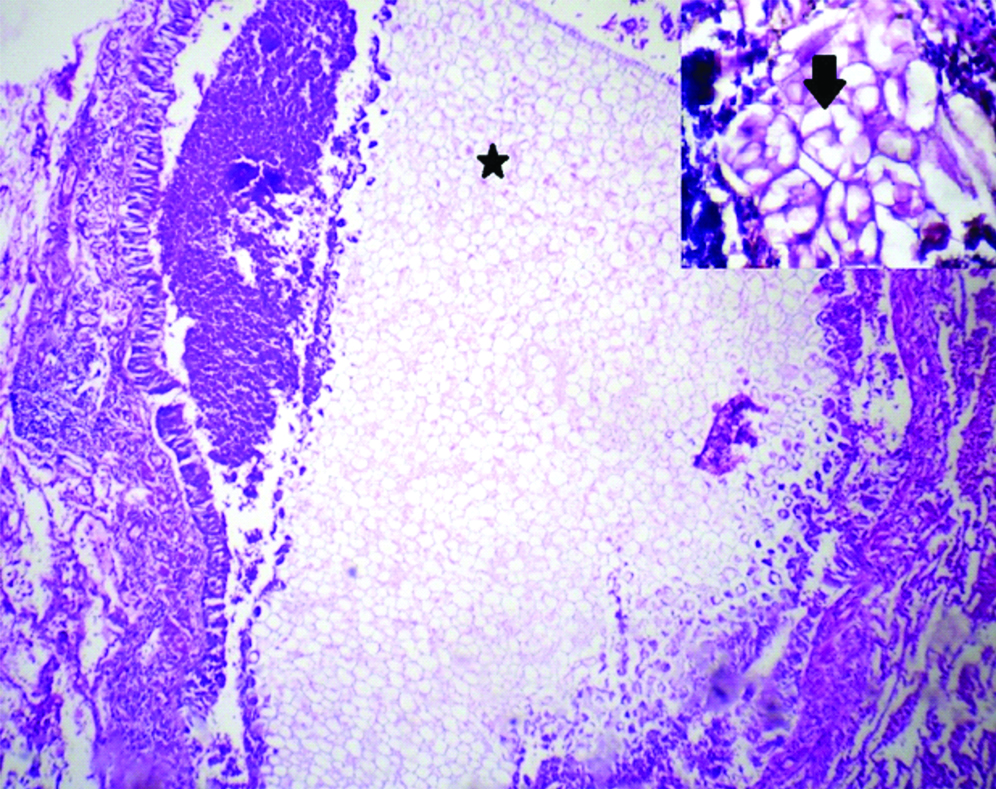
The main histological findings seen in the cases of poisoning were pulmonary congestion, pulmonary oedema, alveolar haemorrhage, haemosiderotic changes, DAD and pneumonia. Four poisoning cases (9%) had aspirated vegetable matter within bronchioles [Table/Fig-12]. The aspirated vegetable matter was characterised by large, non-polarizable, multi-septate elongate to round structures with thick cell walls, honeycomb like internal septation with compartments and occasional pigmentation. Acute bronchiolitis was observed in 18% of right lungs and 11% of left lungs. DAD was seen in 20.5% of right and left lungs each. RAD was seen in 2% of right and left lungs each. Acute bronchiolitis was noted in 18% of right lungs and 11% of left lungs. One case of organophosphorus poisoning with pulmonary embolism had infarct changes in the lung lobes.
Photomicrograph showing foreign vegetable matter (black star) inside a bronchiole (H&E; X100). Inset: Photomicrograph showing vegetable matter with septation (black arrow) (H&E; X400).
The main histological findings seen in the cases of burns victims were pulmonary congestion, anthracosis, pulmonary oedema and alveolar haemorrhage. DAD was seen in 25% of the right and left lungs each.
Discussion
Autopsy is the gold standard for quality check of discrepancies in clinicopathological studies [11]. Majority of the medicolegal autopsies in the present study were of subjects in the third decade, similar to previous studies [3,12-14]. The number of male autopsies outnumbered the female ones (ratio of 2.4:1) and this similar trend was seen in few other studies [3,12-15]. Men are more at risk than women in all types of injuries due to cultural norms and a higher level of outdoor activities [16].
The most frequent manner of deaths were accidents (49%) similar to previous studies [12,13,15]. Suicides (45%) contributed to the second most frequent manner of deaths in contrast to homicidal deaths of the studies done by Molina DK et al., and Mandong BM et al., [12,15].
A major share of autopsy deaths was contributed by RTA (44%) as was seen in studies done by Garg V et al., (59.4%) and Madong BM et al., (39%) [14,15]. RTA trauma is considered as a major cause of morbidity and mortality among young population worldwide [16]. In India, road traffic fatalities have been increasing at about 8% annually for the last ten years and show no signs of declining [17].
In the semi-urban area around the present tertiary hospital, the poor socioeconomic status of the individual and easy availability could have contributed to the high frequency of deaths due to suicidal poisoning (36%). In the present study, among all the 44 poison cases, 10 were due to organophosphorus compounds, one was due to rat killer poison (aluminium phosphide), one was due to paraquat poison (herbicide) and in the remaining 32 cases, the poison was unknown. Among the poisoning cases in the current study, organophosphorus poisoning was the most commonly used known chemical for suicide, as compared, to vehicle exhaust gas in England and Wales, and carbon monoxide poisoning in Japan [18].
Respiratory dysfunction after burns is multi-factorial, where ARDS and inhalation injuries are the most important [8]. The early onset of Acute Respiratory Distress Syndrome (ARDS), together with the changes in white blood cell count and organ dysfunction, favour a syndrome in which respiratory distress is induced by an inflammatory process mediated by the impact of the burns instead of being secondary to sepsis [8]. All burns victims in the present study were females.
Four cases had died due to sudden death (three males with atherosclerosis; of which two had myocardial infarction).
Two cases had an absence of horizontal fissure in the right lung (1.7%) which was much lower than that seen in other various other studies by Quadros LS et al., and Meenakshi S et al., [19,20]. The horizontal fissure separates the superior and middle lobes [1]. If pulmonary development is defective, it will give rise to variations in lobes and fissures [20-22]. A four stage fissural classification has been described [20,23]. In the present study, both cases had Grade III stage with the visceral cleft seen along a part of the fissure [Table/Fig-7].
Saddle thromboembolus in the pulmonary artery was seen in one case of organophosphorus poisoning with a long hospital immobilised stay and in one other case of RTA. The usual source of pulmonary emboli is thrombi in the deep veins of the leg in more than 95% of cases. Large emboli lodge in the main pulmonary artery or its major branches or at the bifurcation as a saddle embolus [24].
Pulmonary congestion was observed in most cases (77.7% of right lungs and 73.8% of left lungs), similar to what was seen in the previous study [3].
Pulmonary oedema can result from hemodynamic disturbances or from direct increases in capillary permeability, due to alveolar septal microvascular injury [24]. Histologically, intra-alveolar granular pink precipitate and engorged alveolar capillaries are seen [24]. It was observed in 47% of right lungs and 47.7% of left lungs in the current study, which was higher than that seen in the study done by Pathak A [3]. The high incidence could be attributed to the microvascular injury from circulatory failure associated with inciting causes like RTAs, burns, chemicals and snake bites. DAD from a respiratory insult like poison could also have contributed to the microcirculatory injury. Alveolar micro-haemorrhages and haemosiderin-laden macrophages may be present in cases where there is haemorrhage into the alveoli [24].
Alveolar haemorrhage, resulting due to an injury to the alveolar microcirculation was observed in 37.6% of right lungs and 39.6% of left lungs in the present study, which was higher than that seen in the study (9.2%) done by Soiero A et al., [25,26].
Most of the time, haemosiderosis could be due to recurrent alveolar haemorrhage. In the present study, it was observed in 32.5% of right lungs and 34.2% of left lungs.
ARDS is associated with inflammation-related increase in pulmonary vascular permeability and epithelial and endothelial cell death. DAD is the histologic manifestation and derived from severe injury to the alveolocapillary unit [27,28]. DAD is not always uniform in severity or appearance from one microscopic field to another [28]. The acute phase is characterised by hyaline membranes [27]. In the present study, DAD was observed in 13.6% of right lungs and 13.5% of left lungs, similar to that seen in the study done by Yazdy AM et al., [29]. However, in a study done by Soeiro A et al., which was performed in all cases of acute respiratory failure, DAD was observed in 45.3% of the cases [26]. The lower rate of DAD in the present study could be due to the fact that most of the cases (86.5%) did not die of acute respiratory failure. Instead, these cases could have died due to circulatory failure from inciting causes of RTA, burns, chemicals, trauma and snake bite.
RAD or regional DAD is defined as one or more macroscopically visible discrete areas of consolidation that had the macroscopic and histologic characteristics of DAD and occupied <50% of the bilateral cut surface [29]. It was speculated that it could result from irregular blood flow related to vascular occlusion, irregularly distributed microvascular injury, or from a combination of factors [29]. In the present study, RAD was observed in 5% of the right lung cases (6) and 2% of the left lung cases (2), which was slightly higher compared to a previous study (1.2%) [29]. In injured lungs, Type 2 pneumocyte hyperplasia is a universal reaction [30-32]. In the present study, gram-positive and negative bacteria were observed in 6.8% of right lungs and 3.6% of left lungs. This could be due to the normal anatomical structure of the right bronchus. This occurrence of coccobacilli/bacilli/cocci could have been due to the aspiration of the normal oropharyngeal flora during the traumatic event. Aspiration pneumonitis is defined as acute lung chemical injury after the inhalation of regurgitated sterile gastric contents [33]. This occurs in patients who have a marked disturbance of consciousness resulting from a drug overdose, seizures, a massive cerebrovascular accident, or the use of anaesthesia [33]. Bacterial infection may occur at a later stage of lung injury [33]. The inflammatory response in the lungs probably results from both bacterial infection and from the inflammatory response to the particulate gastric matter [33]. Histologically, the presence of multinucleated giant cells, foreign-body granulomas, the finding of foreign material and/or acute bronchopneumonia/ bronchiolitis in the background of fibroblastic foci should favour the diagnosis [34]. In the present study, aspirated food identified by starch/vegetable matter was seen inside the bronchioles in 3.4% of right lungs (4) and 1% of left lungs (1). All were cases of poisoning. This again could be due to the normal anatomical structure of the right bronchus. These structures of vegetable matter were similar to the description in the study done by Mukhopadhyay S and Katzenstein AL, [34]. All these cases had acute bronchiolitis (18% right lungs and 11% left lungs of poisoning cases) and changes of pneumonia, which were probably due to aspiration of the normal oropharyngeal flora.
Lung changes in poisoning cases are characterised by acute lung injury in the form of DAD, BOOP, Diffuse Alveolar Haemorrhage (DAH) and acute pulmonary oedema. Poisoning from agrochemical agents like organophosphates, organochlorine compounds, paraquat and aluminium phosphides can cause death by many mechanisms like paralysis of respiratory muscles, respiratory arrest due to a failure of the respiratory centre, intense bronchoconstriction, ARDS or CNS toxicity [35,36]. Rat killer poison (aluminium phosphide) can cause death by cardiovascular toxicity like arrhythmias, cardiogenic shock and ARDS [36]. In the present study, 9 out of 44 poison cases had DAD (20.5%). So, the remaining cases could have died due to the other reasons mentioned above.
In most cases (86.5%), the cause of death was not because of DAD or acute respiratory failure. It was probably due to microvascular circulatory failure as evidenced by alveolar haemorrhage, congestion and oedema due to RTA, burns, snake bites or trauma. Circulatory failure could have led to hypoxic injuries to the other organs like brain, kidney, and liver.
Until alternatives to autopsy are fully established, autopsy, including histology, remains the most accurate method of concluding the cause of death and other significant diagnoses [37].
Autopsies will only decrease the discrepancy rates, enabling clinicians to understand the different spectrums of various diseases, and also allowing audit for diagnostic accuracies [38].
Studies regarding the correlation of clinical diagnosis and autopsy diagnosis point out the value of the postmortem examination as an educational-cum-audit tool in the hospital environment [5]. The highest frequencies of discrepancies between the gross and microscopic findings were found in the lung [11]. With respect to emphysema diagnosis in the right lungs, 57% (eight cases) of emphysema cases were grossly seen and 43% (six cases) were grossly missed. Whereas in the left lungs, 37.5% (six cases) of emphysema cases were grossly seen and 62.5% (10 cases) were grossly missed. In the study by Molina DK et al., the grossly correct cases were 60% [12]. There are some entities that maybe are similar at gross examination such as bronchopneumonia and DAD [11]. Therefore, histology is still essential to confirm or refute the macroscopic diagnosis [37].
Limitation
Few of the limitations in this study included autolysis and lack of clinical and drug history.
Conclusion
The histological findings seen in the RTA cases were associated with circulatory failure manifesting in the lungs as alveolar haemorrhage, congestion and oedema, microvascular damage and eventually multi-organ injury. DAD was more commonly observed in cases of poison and burns than in RTAs. The most frequent manner of deaths was accidents (RTA), followed by suicides (poisoning and burns) and sudden death. Autopsy including histology plays an important role in the evaluation of the cause of death.