Intertrochanteric fractures account for 50% of all fractures of the proximal femur, with women to men ratio ranging from 2:1 to 8:1, the average age of incidence being 66 to 77 years. Some of the factors associated with intertrochanteric fractures include advancing age, increased number of comorbidities, increased dependency in activities of daily living and a history of other osteoporosis related (fragility) fractures [1].
Operative stabilisation permits early mobilisation and minimises complications of prolonged recumbency [2]. The DHS was introduced by Clawson DK, in 1964 [3] and has been widely adopted as the implant of choice for these fractures [4]. With respect to failure mechanisms, a common form is cut-out i.e., migration of the implant through the cancellous bone of the femoral head, which significantly relates to the bone mineral density of the proximal femur [5]. The failure rates associated with the DHS vary between 5% [6] and 23% [7]. However, a more recent study reported improved results, with a failure rate of fixation of 3.2% and a cut-out rate of 1.9% [8]. The most common mode of failure with the DHS is collapse of the femoral neck into varus, leading to cut-out of the screw [4].
Recently, a helical shaped implant design was introduced in order to enhance implant anchorage. The DHS blade was developed in an attempt to enhance anchorage of the implant in the bone. The mechanical purchase mechanism of the DHS blade comprises four helical blades at the head of the implant [5]. Biomechanical studies [5,9] have shown improved resistance to cut-out and increased rotational stability of the femoral head fragment with helical implants when compared with traditional hip lag screws, but limited published studies are available on the clinical outcome of this implant [9].
In order to evaluate the above claimed biomechanical properties of the DHS blade, this study was carried out to analyse the outcome of the DHS blade in intertrochanteric fractures of femur in the elderly osteoporotic patients.
Materials and Methods
This descriptive observational study was carried out in the Departement of Orthopaedics, Himalayan Institute of Medical Sciences from October 2011 to September 2013. The inclusion criteria for the study were: Age over 60 years, AO classification-AO31A1 to A3, Singh’s Index Grade ≤3. Fractures were classified as per AO/ASIF classification. Osteoporosis was graded as per Singh’s Index [10] which was assessed from anteroposterior radiographs of the contralateral hip. In this study, 32 patients were enrolled, out of which two were excluded (one died due to causes unrelated to orthopaedics and one patient did not turn up for follow-up). So, overall 30 patients were included in the present study with a follow-up period of 24 weeks. Pre-operatively, all the patients were subjected to routine haematological investigations and pre-anaesthetic check-up.
Technique
After positioning the patient on the fracture table, closed reduction of the fracture was done under C-arm control. After painting and draping of the affected hip were done, a four inches long incision was given starting from the greater trochanter along the lateral aspect of thigh. The DHS guide wire was placed in the middle of the femoral head extending into the subchondral bone. After reaming with the triple reamer, appropriate size of DHS blade was inserted. The DHS plate was fixed to the blade and attached to the femoral shaft followed by locking of the DHS blade. Closure of the surgical wound was done in layers.
IV Antibiotics were given one hour prior to surgery as prophylaxis and continued for three days postoperatively. Physiotherapy was started on the 2nd day of surgery after removal of the drain. Toe touch weight bearing was allowed after one week, partial weight bearing after two weeks and full weight bearing once the signs of union were present. Follow-ups of the patients were done at 6, 12, 18 and 24 weeks with clinical and radiological evaluation. The patients were evaluated as per the Harris Hip Score [11] from 12th week onwards.
Statistical Analysis
Interpretation and analysis of obtained data were done using descriptive statistics. Data were entered and analysed on Microsoft Office Excel 2007.
Results
Thirty patients were operated with DHS blade and followed up for a minimum of six months. The male to female ratio was 1:2.75. The mean age of patients was 73.4±8.64 years (range 60-97 years) [Table/Fig-1].
Age and sex distribution of study subjects (n=30).
| Age group (in years) | Males | Females | Total |
|---|
| 60-69 | 2 (6.6%) | 8 (26.7%) | 10 (33.3%) |
| 70-79 | 5 (16.6%) | 8 (26.7%) | 13 (43.3%) |
| ≥80 | 1 (3.3%) | 6 (20%) | 7 (23.3%) |
| Total | 8 (26.7%) | 22 (73.3%) | 30 (100%) |
Trivial trauma due to domestic falls was the most common mode of injury accounting for 23 cases (76.7%). Road Traffic Accidents accounted for 5 cases (16.6%); 4 (13.3%) were males while 1 (3.4%) was female. Two cases (6.6%) were due to fall from height; both were females. The right hip was involved in 13 patients (43.3%) while left hip was involved in 17 cases (56.7%). Fractures were classified using AO/ASIF classification. There were 10 cases (33.3%) of AO-31A1 and 20 cases (66.7%) fell in AO-31A2. Pre-operatively, the patients were categorised as per Singh’s Index; 20 cases (66.7%) were in Grade 3 while 10 cases (33.3%) fell in Grade 2.
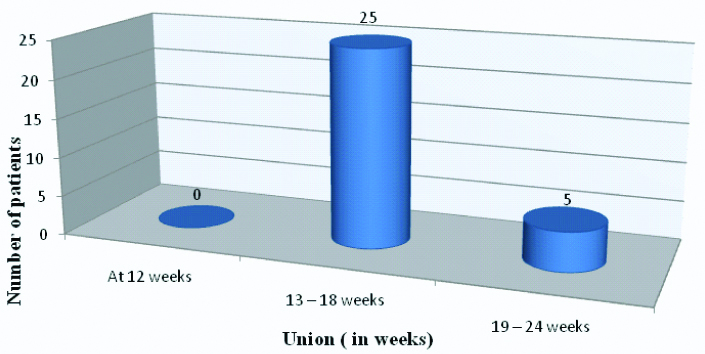
The mean operating time was 74.3 minutes. Post-operatively, the average TAD was 21.66 mm (range 18-28 mm). 25 cases (83.3%) had TAD <25 mm. Neck-shaft angle of the contralateral hip was measured for comparison. No change in neck-shaft angle was observed in 21 cases (70%) however varus collapse more than 4° was seen in 2 cases (6.6%). The patients were followed up for a minimum of 24 weeks. In most of the cases (83.3%), union was seen between 13-18 weeks while in 5 patients (16.6%) it was observed between 19-24 weeks [Table/Fig-2]. The mean Harris Hip Score (HHS) was 90.1. Most of the patients (24, 80%) had excellent results (HHS 90-100), while 13.3% (4) had a good result (HHS 80-89) and 6.7% (2) had a fair result (HHS 70-79) with none having poor result.
Union Time in operated cases (n=30).
In 2 cases (6.66%), the authors encountered screw penetration leading to varus collapse, shortening of the limb and medialization of the distal fragment. Both these cases were given the option of revision surgeries, but they opted for implant removal instead.
Discussion
In elderly patients with intertrochanteric fracture, any plan of treatment must consider the peculiarities of bone and soft tissues such as osteoporosis, impaired blood supply, poor healing potential and susceptibility to pressure sores. A careful evaluation of all these consideration is a prerequisite to the effective treatment of the elderly injured patients [12].
DHS is still the implant of choice for fixation of trochanteric fractures because of its low rates of implant failure and non-union however higher complication rates in unstable and osteoporotic fractures have led some surgeons towards DHS blade which theoretically decreases cut-out rates as it allows compaction in osteoporotic femoral head which improves anchorage [2].
Domestic fall or fall at home was the most common mode of trauma in the present study accounting for 23 cases (76.7%). These findings were coherent with findings of Al-Yassari G et al., [13]. In their study majority of the cases were due to fall at home (85.7%). Fractures were classified according to AO/OTA classification. Majority of the fractures (66.7%) fell in AO 31-A2 group. These findings were similar to the studies of Leung F et al., and Stern R et al., [14,15]. In their studies also majority of the cases (53% and 54% respectively) fell in AO31- A2 group. In the current study, osteoporosis was graded radiologically on the basis of Singh’s Index. In the present study, 66.7% of cases were in Grade 3. Siwach RC et al., in their study found 70.5% cases in Grade 3, Al Yassari G et al., in their study of trochanteric fractures in elderly age group reported 74% of cases in Grade 3 [2,13] Laohapoonrungsee A et al., in their clinical study to evaluate the role of dynamic hip screw in trochanteric fractures in elderly patients observed 70% of their cases in Singh’s Grade 3 [4]. These findings were coherent with the present study. Majority (73.3%) of the cases in the present study were females. Leung F et al., had 65% females, Stern R et al., in their study had 76.1% females, while Fitzpatrick DC et al., had 66.7% of female patients in their study [14-16]. This shows that the elderly females are more prone to intertrochanteric fractures, most probably due to post-menopausal osteoporosis.
The mean Harris Hip Score in the present study was 90.1 which was similar to the findings of Siwach et al., [2], who, in their study had a mean HHS of 92.87.80% of the patients in the present study had an excellent result (HHS 90-100), 13.33% had a good result (HHS 80-89) and 6.67% had a fair result (HHS 70-79) with none having poor result. Similarly, Siwach RC et al., observed 82.35% having an excellent result, 11.76% had a good result with 5.88% having a poor result [2]. The mean HHS in the present study was better than that reported by Wong TC et al., who reported a mean HHS of 86.2 in their study using DHS [17].
In this study, fracture united in all the cases and the time of the union ranged from 13 to 24 weeks. Majority of the cases (83.33%) showed union by 13 to 18 weeks. The union was defined radiologically as the presence of the bridging callus and the haziness of the fracture line on anteroposterior and lateral radiographs, while clinically it was defined by the absence of pain, tenderness and ability to bear weight. Siwach RC et al., [2] used DHS blade in unstable, osteoporotic trochanteric fractures and reported average time for union to be 13.14 weeks. Similarly, Laohapoonrungsee A et al., observed mean time to union to be 14.5 weeks [4]. These findings were coherent with the present study.
All the cases were fixed with DHS blade with Locking Compression Plate. Studies have shown superior implant anchorage of the DHS blade compared to DHS, which might reduce the cut-out risk [5] and provided better rotational stability [18]. Moreover, use of locking screws provided additional axial stability. Jewell DP et al., in a study concluded that a locking screw DHS would be particularly useful in patients with osteoporotic bone and in patients with less stable fracture configurations [19]. In spite of these advantages, in the present study, 2 cases (6.6%) out of 30 had screw penetration with varus collapse and medialization of the distal fragment.
Siwach RC et al., in their study had 7.8% of cases of mechanical failure of the DHS blade with cut-out rate of 2%. [2]. Similar results were reported by Fitzpatrick DC et al., in a randomised prospective study, comparing DHS and DHS blade, a failure rate of 7.4% in the DHS blade group while there was no failure in the DHS group [16]. However, O’Malley NT et al., in their comparative between DHS and DHS blade found comparable failure rates in both the groups (DHS-2%, DHS blade- 2.3%) [9]. In another prospective randomised study comparing screw versus helical blade in trochanteric fractures, Stern R et al., reported screw cut-out rate of 2.9% and blade cut-out rate of 1.5%, which was again comparable [15].
Rates of failure with DHS have been reported in the literature. Hsueh KK et al., reported a screw cut rate of 6.8%, Adams CI et al., found a cut-out rate of 2% which was similar to cut-out rate of 1.9% as reported by Chirodian N et al., [8] in a study on sliding hip screw fixation of trochanteric hip fractures [20,21,8]. Cut-out rates as high as 10.6% have been reported in the literature [Table/Fig-3] [22].
Comparative analysis of failure rates.
| Study | Failure rate (%) DHS blade | Failure rate (%) DHS |
|---|
| Siwach RC et al., [2] | 7.8% | |
| Chirodian N et al., [8] | | 1.9% |
| O’Malley NT et al., [9] | 2.3% | 2% |
| Stern R et al., [15] | 1.5% | 2.9% |
| Fitzpatrick DC et al., [16] | 7.4% | None |
| Hsueh KK et al., [20] | | 6.8% |
| Adams CI et al., [21] | | 2% |
| Present study | 6.6% | |
Reason for implant failure could be the conversion of the dynamic implant into a fixed angle implant. In both the cases of implant failure, there was maximal collapse at six weeks, which did not allow further collapse leading to screw penetration into the joint along with varus collapse and medialization of the distal fragment.
Limitation
The present study had its limitations; the number of the patients were less, so results cannot be generalised and having no control group was another limitation.
Conclusion
The DHS blade is a reliable and safe method of treatment in intertrochanteric fractures in the elderly patients as far as rates of union and functional outcome are concerned. Although the DHS blade is considered to be superior to DHS in cut-out strength, but it has similar rates of cut-out or implant failure as compared to DHS.