Case Report
A 32-year-old male patient arrived at the Oral Medicine Clinic with the chief complaint of an uncomfortable nodule in the region of upper vestibular sulcus with evolution of 2 years. In addition, the patient reported that he had painful symptomatology for 3 months. The patient reported no significant medical history regarding systemic diseases, allergic reactions or previous surgery/surgical complications. Also, the patient presented excellent dental condition, without any compromised teeth in the affected area.
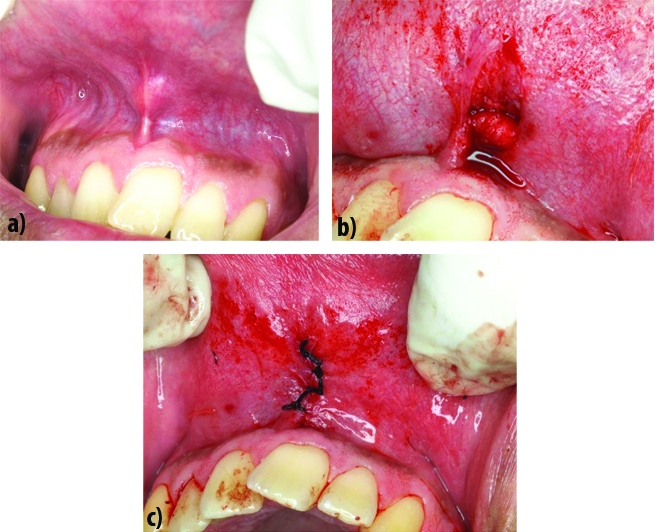
Intra oral examination, showed a fluctuating nodule in the midline of the vestibular sulcus, extending towards the upper lip with normal colour, tender on palpation, measuring about 0.8 cm wide, without any extra oral alteration [Table/Fig-1a]. Based on the clinical presentation, the common differential diagnosis were chronic periodontal/periapical abscess, lipoma and fibroma irt upper vestibular sulcus. However, abscess was ruled out as patient gave negative history of trauma, no tooth discolour and no caries was appreciated. “Slip sign” was negative, so lipoma was also ruled out. For fibroma and its similar appearing types there was negative history of chronic irritation/trauma, so this was also not considered. Hence, the main diagnostic hypothesis for the case was pleomorphic adenoma, or other soft tissue tumour such as Schwannoma, Palisade Encapsulated Neuroma and Traumatic Neuroma.
a) Nodule in the midline of the vestibular sulcus extending towards the upper lip; b) Surgical removal of the lesion; c) Immediatepost-surgical view, after repositioning and final sutures in place.
We narrowed the possible hypotheses to these four lesions because the traumatic neuroma presents as masses or nodules of few diameter that can be related to pain and numbness symptoms, most often associated with trauma, also the mucosa presents with normal colour and the upper lip is one of the most affected sites. The palisade encapsulated neuroma usually manifests as a small, solitary and firm nodules, which never exceeds 1.0 cm, may manifest on the upper lip; while the Schwannoma usually are solitary, encapsulated, slow growing and painless, affecting the tongue, lips and vestibule is the most affected site. The Pleomorphic Adenoma usually presents as a swelling of firm consistency, slow growing painless growth, covered by mucosa of normal colour [1,2].
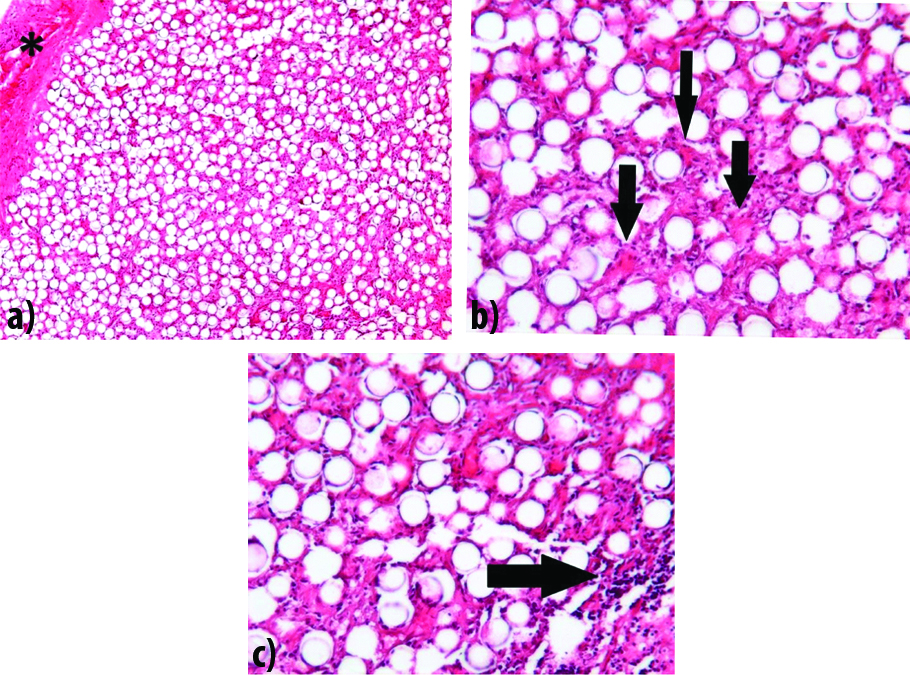
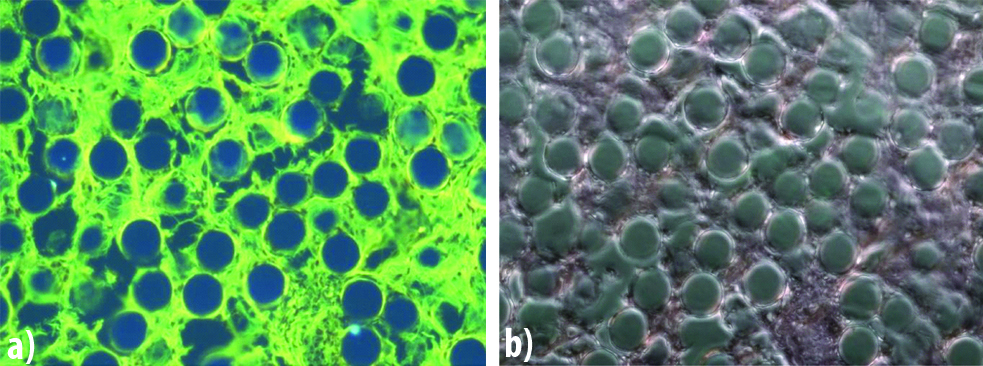
Based on the clinical evaluation an excisional biopsy was performed, and the fragment of soft tissue was obtained presenting an irregular surface and firm consistency measuring 1.5×0.7×0.7 cm. [Table/Fig-1b,c]. The microscopic evaluation revealed fragments of loose connective tissue with a capsular organisation surrounding multiple spherules of transparent synthetic material of uniform diameter, circumscribed by giant foreign body type cells [Table/Fig-2a,b]. In addition, area of fibrosis and focal intense inflammatory lymphocytic infiltrate was present [Table/Fig-2c]. Through the technique of fluorescent and polarised microscopy, the transparent synthetic material did not present birefringence in polarised light and fluorescent properties [Table/Fig-3a,b]. The distinctive microscopic features lead to the final diagnosis of foreign body granuloma caused by Polymethylmethacrylate.
a) Haematoxylin and Eosin (HE) stain showing a loose connective tissue forming a circumscribed capsule surrounding the foreign body granuloma (asterisk) Magnification X100; b) Haematoxylin and Eosin (HE) stain. Multiple spherules of transparent synthetic material of uniform diameter circumscribed by giant foreign body type cells (arrows). Magnification X400; c) Haematoxylin and Eosin (HE) stain. Areas of intense inflammatory lymphocytic infiltrate (arrows). Magnification X400.
a) Fluorescence microscopy, Red fluorescence filter showing no fluorescent property for the Polymethylmethacrylate; b) Polarised light microscopy showing no birefringence for Polymethylmethacrylate.
With the histopathological report, the patient was confronted why he did not mention other surgical procedures in that region. Only then, the patient stated that he underwent a rhinoplasty procedure which was done five years back, but he could not relate it to the oral lesion. The patient was kept under close follow-up for one year three months and the patient showed no signs of complication or relapse on follow-up.
Discussion
Facial aging is a progressive process of diminished subcutaneous fat and dermic collagen resulting in facial depressions. As aging is accompanied by loss of volume of the subcutaneous fat and dermic collagen, the autologous solution with fat graft and the autologous fibroblasts has the best biocompatibility, but has limited duration. The late reabsorption of the fat graft and the high cost of the procedures would lead substitution to graft for another material;among them is the PMMA [3]. Formerly, the treatment for facial aging was more conservative directed to procedures of lifting and repositioning of tissues. Currently, with the advent of alloplastic materials, the renewal of facial contours became the first line of treatment before surgical corrections.
Foreign body granuloma is thought to be an infrequent lesion, which is related to amount of alloplastic material injected on an inner surface or more superficial dermis. The form of material filling indicates whether there will be more intense inflammation or not, the correct choice of material being a crucial step. The clinical investigation of the patient and the importance of the differential diagnosis seems to be decisive in the definitive prognosis of material facial filling, because according to literature, the development granuloma occurs among 0.01% to 2.5% of applications [4].
Polymethylmethacrylate (PMMA) is the most commonly used permanent filling material, which is composed by microspheres (30-40 microns) and generally associated to bovine dermal collagen. Glabellar frown, nasolabial and radial lip folds, perioral lines, depressed corners of the mouth, lip augmentation, and acne scars are the main indications for its use. Injecting fillers into the subcutaneous fat layer are considered safe, but if placed into the deep dermal layer it may cause side effects such as nodules, inflammation, allergic reactions and foreign body granuloma formation [5].
The material indicated for facial filling needs to have properties such, biocompatibility, clinical and chemical tolerance, no carcinogenic activity, and should not cause any adverse inflammatory response [6]. According to Shahrabi FS et al., the dermal fillers collagen and hyaluronic acid may be classified into degradable/ resorbable fillers and the silicone into permanent/non-resorbable filler. Also, the dermal fillers are categorised into filling/volumizing, biostimulatory, or combined fillers based on their space-filling or stimulatory effects on the dermal microenvironment [7]. Autografts are safer due to its biocompatibility and absence of allergic reactions, for example, adipose tissue graft, but the disadvantage is the unpredictable reabsorption of material, the high cost of the procedure and the donor site of the collected material [8]. The autologous fibroblasts, technique that uses living cells of the patient itself has the advantage of prolonged result, because these cells reactivate the own production of collagen and elastin; however, the high cost and the complex procedures related to this technique restricts its use [9].
The facial filling materials must be injected subdermally. The injected volume depends on the depth and size of the skin defect or wrinkle. Complications may appear when it is applied in the superficial dermis and the material spreads to other undesirable regions. In addition, a high volume of the applied filler, excessive pressure during application and excessive muscular movement, or natural tension lines could contribute to distant migrations, being the feminine gender the most affected group [5,10].
Clinical investigation is extremely important, because in intraoral and perioral areas the lesions mimic mucus extravasation cysts, neoplasms and soft tissue tumours, especially the minor salivary gland [10] such as Pleomorphic Adenoma, (thought as a differential diagnosis in the present case report). Such clinical characteristics are usually: undefined, floating nodule, with normal colour, well circumscribed, and sometimes related to pain [11]. Therefore, a good clinical investigation during the diagnostic process is very important considering the large amount of differential diagnosis possible to happen in the oral cavity.
Da Costa Miguel MC et al., reported a similar case. A 56-year-old woman, presented for evaluation of a swelling in the lower lip [11]. A firm pink nodule covered with non-ulcerated mucosa, located in the right anterior inferior alveolar mucosa was revealed on intraoral examination. The initial clinical diagnosis was salivary gland mucocele and an excisional biopsy was performed. When asked about any aesthetic procedure performed close to the anatomical site, the patient reported the injection of a cosmetic filler containing PMMA for lip enlargement performed almost 1 year earlier. Then, the definitive diagnosis was foreign body granuloma due to cosmetic filler injection.
When the filler has a more irregular surface and is of varied size, it can generate a high inflammatory response. Serious side effects with PMMA may be caused, but in varied intensities depending on the amount and depth at which it is applied, including foreign body granuloma, allergic reactions and displacement deformity, More severe complications caused by accidental vascular injection could cause embolism, facial necrosis and blindness [12].
The histiocytic presence in the inflammatory infiltrate caused by PMMA has been identified immunohistochemically with CD68 marker [13]. The polarised light and fluorescent microscopy used in the present case, contributed to further knowledge about the material. Since other compounds may have fluorescent properties or birefringence such asPoly-L-lactic acid and silicone, the PMMA containing bovine collagen or carboxygluconate does not shown birefringence properties [14]. As shown on [Table/Fig-3] histologically, PMMA is presented as multiple spherules of uniform size, the Silicone (Polydimethylsiloxane) has a “bubbly” aspect in microscopy, while Poly-L-lactic acid and hyaluronic acid, presents respectively as a “rice-shaped” and irregular morphology [Table/Fig-4] [5].
Table showing the microscopic morphology of synthetic filling materials.
| Synthetic material | Morphology |
|---|
| Polymethylmetacrylate |  |
| Polydimethylsiloxane |  |
| Polylatic acid |  |
| Hyaluronic acid |  |
Some aesthetic filling materials may produce inflammatory reactions resulting in tissue destruction, even mimicking malignant tumours. Gonçales ES et al., reported a case of silicone implant mimicking a low-grade liposarcoma in oral cavity [15]. Occasionally, the silicone loaded histocytes can have atypical nuclei and mimic this malignant tumour. The silicone particles are degraded into smaller particles inside the macrophages appearing as multivacuolatedlipoblast-like cells with variable sizes, what, in routine H&E staining, could be interpreted as a liposarcoma [15]. PMMA is a permanent/non-resorbable filler, its large round particles can only be phagocyted by a giant strange body multinucleated cell.
The primary treatment of foreign body granuloma caused by synthetic fillers include: intralesional injections with corticosteroids how the Fluoracil-5 and Bleomycin, systemic therapy with Minocycline, Allopurinol, Colchicine, Cyclosporine and prednisolone and surgical therapy with excision, incision and drainage and fat graft or flaps. In this case report, the surgical removal performed during excisional biopsy was able to remove the lesion completely, leading to a complete remission of the clinical signs and symptoms of the patient.
Conclusion
The histopathological diagnosis of findings confirmed the final diagnosis as foreign body granuloma. PMMA injection should be well distributed, in order to prevent similar lesions, as reported in the present case. The microscopic features showed that excessive quantities of the material might act as a local irritant, despite of its biocompatibility.
[1]. Kuo YL, Tu TY, Chang CF, Li WY, Chang SY, Shiao AS, Extra-major salivary gland pleomorphic adenoma of the head and neck: a 10-year experience and review of the literatureEur Arch Otorhinolaryngol 2011 268(7):1035-40.10.1007/s00405-010-1437-221120660 [Google Scholar] [CrossRef] [PubMed]
[2]. Kuriakose MA, Chakrabarti S, Cheong SC, Luiz PK, Tiago NP, Camile SF, Head and Neck Tumours. In: Farah C., Balasubramaniam R., McCullough M. (eds)Contemporary Oral Medicine 2018 Springer, Cham10.1007/978-3-319-28100-1_20-1 [Google Scholar] [CrossRef]
[3]. Vargas AF, Amorim NG, Pintaguy I, Late complications of permanent fillersRev Bras CirPlást 2009 24(1):71-81. [Google Scholar]
[4]. Gladstone HB, Wu P, Carruthers J, Backgroud Information on the use of esthetic fillers. In: Carruthers J, Carruthers A, edsSoft Tissue Augmentation 2005 PhiladelphiaElsevier:1-10. [Google Scholar]
[5]. Loda G, Papaiordanou F, José TMF, Bravo BSF, de Abreu L, Cuzzi T, Surgical approach to multiple foreign body granulomas (PMMA)Surgical & Cosmetic Dermatology 2016 8(4):366-69.10.5935/scd1984-8773.201684793 [Google Scholar] [CrossRef]
[6]. Requena L, Requena C, Christensen L, Zimmermann US, Kutzner H, Cerroni L, Adverse reactions to injectable soft tissue fillersJ Am Acad Dermatol 2011 64:1-34.10.1016/j.jaad.2010.02.064 [Google Scholar] [CrossRef]
[7]. Shahrabi FS, Lerman MA, Noonan V, Kabani S, Woo SB, Granulomatous foreign body reaction to dermal cosmetic fillers with intraoral migrationOral Surg Oral Med Oral Pathol Oral Radiol 2014 117(1):105-10.10.1016/j.oooo.2013.10.00824332334 [Google Scholar] [CrossRef] [PubMed]
[8]. Tamiolakis P, Piperi E, Christopoulos P, Sklavounou-Andrikopoulou A, Oral foreign body granuloma to soft tissue fillers. Report of two cases and review of the literatureJ Clin Exp Dent 2018 10(2):e17710.4317/jced.5419129670737 [Google Scholar] [CrossRef] [PubMed]
[9]. Watson D, Keller GS, Lacombe V, Fodor PB, Rawnsley J, Lask GP, Autologous fibroblasts for treatment of facial rhytids and dermal depressions: a pilot studyArch Facial Plast Surg 1999 1(3):165-70.10.1001/archfaci.1.3.16510937098 [Google Scholar] [CrossRef] [PubMed]
[10]. Carlos-Fabuel L, Marzal-Gamarra C, Martí-Álamo S, Mancheño-Franch A, Foreign body granulomatous reactions to cosmetic fillersJ Clin Exp Dent 2012 4(4):e244-47.10.4317/jced.5086824558563 [Google Scholar] [CrossRef] [PubMed]
[11]. Da Costa Miguel MC, Nonaka CF, Dos Santos JN, Germano AR, De Souza LB, Oral foreign body granuloma: unusual presentation of a rare adverse reaction to permanent injectable cosmetic fillerInt J Oral Maxillofac Surg 2009 38(4):385-87.10.1016/j.ijom.2009.01.01319243914 [Google Scholar] [CrossRef] [PubMed]
[12]. Ozturk CN, Li Y, Tung R, Parker L, Piliang MP, Zins JE, Complications following injection of soft-tissue fillersAesthet Surg J 2013 33(6):862-77.10.1177/1090820X1349363823825309 [Google Scholar] [CrossRef] [PubMed]
[13]. Jham BC, Nikitakis NG, Scheper MA, Papadimitriou JC, Levy BA, Rivera H, Granulomatous foreign-body reaction involving oral and perioral tissues after injection of biomaterials: a series of 7 cases and review of the literatureJ oral Maxillofac Surg 2009 67(2):280-85.10.1016/j.joms.2008.01.05219138600 [Google Scholar] [CrossRef] [PubMed]
[14]. Mercer SE, Kleinerman R, Goldenberg G, Emanuel PO, Histopathologic identification of dermal filler agentsJ Drugs Dermatol 2010 9(9):1072-78. [Google Scholar]
[15]. Gonçales ES, Almeida AS, Soares S, Oliveira DT, Silicone implant for chin augmentation mimicking a low-grade liposarcomaOral Surgery, Oral Medicine, Oral Pathology, Oral Radiology 2009 107(4):21-23.10.1016/j.tripleo.2008.12.04419327631 [Google Scholar] [CrossRef] [PubMed]
[16]. Lee JM, Kim YJ, Foreign body granulomas after the use of dermal fillers: pathophysiology, clinical appearance, histologic features, and treatmentArch Plast Surg 2015 42(2):232-39.10.5999/aps.2015.42.2.23225798398 [Google Scholar] [CrossRef] [PubMed]