Leiomyomas are benign smooth muscle tumours. The most common site of origin of the leiomyomas (uterine fibroids) is the myometrium of the uterus. They are the single most common cause for hysterectomy in the reproductive and peri-menopausal age group [1,2]. They are mostly asymptomatic but may present with menstrual disturbances [3]. These symptoms are mainly due to the hyper-oestrogenic status associated with these tumours. Adenomyosis is a myometrial lesion characterised by the presence of ectopic endometrium in the myometrium. Furthermore, both adenomyosis and leiomyomas commonly coexist in nearly 33% of the cases [4]. This shows the hormone dependency of the leiomyomas. The pathogenesis of the fibroids is still unclear; however recent evidences show that they are due to the steroid hormones, oestrogen and progesterone [5]. The endometrium of the uterus is also under the cyclical influence of these steroid hormones. There are studies suggesting the association of endometrial changes with leiomoyomas such as glandular hyperplasia in the endometrium, this may be the expression of oestrogenic hyperactivity and atrophic endometrium which could be the result of mechanical forces upon the endometrium [6]. Distortion, elongation, and dilatation of the glands are said to be the result of pressure effect of the leiomyoma. Since the leiomyomas are hormone dependant tumours and the uterine endometrium is also under the influence of these hormones, there could be an association between the hormone influence on the leiomyoma and the endometrium changes associated with it. In this study LMP is used as a guide to phase the endometrium and there by identify the abnormal changes in the endometrium which are not correlating with the phase and date of the endometrium.
Materials and Methods
A retrospective study was done on 331 hysterectomy specimens, done for leiomyomas during the period June 2013-May 2015. Haematoxylin and eosin stained sections obtained from the 331 hysterectomy specimens were used for the study. All hysterectomy specimems done for leiomyomas were included and myomectomy specimens, endometrial biopsies, endocervical biopsies, endometrial currettings were excluded from the study. Histopathological evaluation of the gross specimens were done and H&E stained slides were studied and the endometrium was classified as proliferative, secretory, hyperplastic and atrophic, stromal changes and type of leiomyoma was also classified.
Results
In this study, out of 1463 hysterectomy specimens received in two years (June 2013-May 2015) 331 (22.62%) had leiomyomas. Most common age group affected was 41-50 years (56.5%) [Table/Fig-1]. Multiparous women (94.86%-314 cases) harboured more leiomyomas compared to primipara (3.63%-12 cases) and nullipara (1.51%-5 cases). It was observed that menorrhagia was the most common symptom seen in 46.53% (154 cases) followed by abdominal pain in 26.89% (89 cases) of cases. The other symptoms that were observed were post menopausal bleeding (9.67%-32 cases), dysmenorrhoea (3.93%-13 cases), mass descending per vaginum (2.72%-9 cases), polymenorrhoea (2.42%-8 cases), dysuria (1.81%-6 cases) and urinary retention (0.91%-3 cases). A 5.14% (17 cases) of the women were asymptomatic. It was observed that adenomyosis was associated with leiomyoma in 110 cases (33.23%). It was most commonly seen in multiparous women and in the age group of 30-50 years.
It was observed that majority of the cases of leiomyomas were single in number (59.82%-198 cases) and multicentric was 40.18% (133 cases). It was observed that the most common type of leiomyoma encountered was intramural type in 49.85% (165 cases) followed by subserosal and submucosal fibroid seen in 22.66% (75 cases) and 15.11% (50 cases) respectively, leiomyomas in multiple locations was observed in 12.39% (41 cases). One case of broad ligament fibroid was observed. Secondary changes were observed in 39.27% (130 cases) of the leiomyomas of which the most commonest secondary change was found to be hyaline change observed in 23.87% (79 cases) of the leiomyomas. The other secondary changes that were observed were cystic change (11 cases), haemorrhage (12 cases), calcification (2 cases), lymphocytic infiltration (4 cases), infarction (1 case), osseous metaplasia (1 case) and lipoleiomyoma (5 cases). Red degeneration which occurs in pregnancy was observed in one case.
In this study of 331 cases, the most common type of endometrium associated with a leiomyoma was proliferative endometrium observed in 44.41% (147 cases). Hyperplasia without atypia was seen in 16.92% (56 cases) [Table/Fig-2].
Age distribution of leiomyoma.
| Age group | Frequency | Percentage |
|---|
| 21-30 | 2 | 0.60% |
| 31-40 | 92 | 27.79% |
| 41-50 | 187 | 56.50% |
| 51-60 | 42 | 12.69% |
| 61-70 | 7 | 2.11% |
| 71-80 | 1 | 0.30% |
| Total | 331 | 100% |
Endometrial changes in leiomyoma.
| Type of endometrium | Frequency | Percentage |
|---|
| Early proliferative endometrium | 10 | 3.02% |
| Late proliferative endometrium | 137 | 41.39% |
| Early secretory endometrium | 36 | 10.88% |
| Late secretory endometrium | 21 | 6.34% |
| Secretory endometrium with arias stella reaction | 3 | 0.91% |
| Pill endometrium | 6 | 1.81% |
| Atrophic endometrium | 30 | 9.06% |
| Disordered proliferative endometrium | 30 | 9.06% |
| Simple hyperplasia without atypia | 34 | 10.27% |
| Complex hyperplasia without atypia | 22 | 6.65% |
| Endometrioid adenocarcinoma | 2 | 0.60% |
| Total | 331 | 100% |
It was found that hyperplasia without atypia was most common in subserosal fibroids (20%) and atrophic endometrium was most common in multiple leiomyoma [Table/Fig-3].
Correlation of type of leiomyoma with type of endometrium.
| Type of endometrium | Leiomyoma | Total |
|---|
| Intra-Mural | Multi-Ple | Submucosal | Sub serosal |
|---|
| Proliferative endometrium | 78 | 19 | 18 | 32 | 147 |
| 47.28% | 46.34% | 36% | 42.67% |
| Secretory endometrium | 24 | 12 | 11 | 10 | 57 |
| 14.55% | 29.27% | 22% | 13.34% |
| Disordered proliferative endometrium | 16 | 1 | 5 | 8 | 30 |
| 9.7% | 2.44% | 10% | 10.67% |
| Atrophic endometrium | 15 | 2 | 5 | 8 | 30 |
| 9.1% | 4.88% | 10% | 10.67% |
| Hyperplasia of endometrium | 26 | 7 | 8 | 15 | 56 |
| 15.76% | 17.07% | 16% | 20% |
| Others | 6 | - | 3 | 2 | 11 |
| 3.64% | - | 6% | 2.67% |
| Total | 165 | 41 | 50 | 75 | 331 |
| 49.85% | 12.39% | 15.1% | 22.7% |
The stromal changes were in concurrence to the corresponding type of endometrium observed i.e., for proliferative endometrium and hyperplasia the stroma appeared cellular and compact, for secretory endometrium the stroma was edematous, decidualised stroma was seen in Pill endometrium and Arias-Stella reaction.
In this study, Last Menstrual Period in days were divided into 3 groups as 7 to 15 (84 cases), 16 to 30 (118) and more than 30 (129). Late proliferative endometrium was the predominant type in all 3 categories of LMP. [Table/Fig-4] suggests proliferative changes persisting in majority of cases of leiomyoma beyond 15 days of LMP giving light to a hormonal influence of the leiomyoma.
Last Menstrual Period (LMP) and endometrium.
| Type of endometrium | LMP in days | Total |
|---|
| 7-15 | 16-30 | >30 |
|---|
| Early proliferative endometrium | 3 | 2 | 5 | 10 |
| 3.6% | 1.7% | 3.9% | 3.0% |
| Late proliferative endometrium | 52 | 34 | 51 | 137 |
| 61.9% | 28.8% | 39.5% | 41.4% |
| Early secretory endometrium | 3 | 24 | 9 | 36 |
| 3.6% | 20.3% | 7.0% | 10.9% |
| Late secretory endometrium | 2 | 15 | 4 | 21 |
| 2.4% | 12.7% | 3.1% | 6.3% |
| Secretory endometrium with arias stella reaction | -- | 3 | -- | 3 |
| 2.5% | .9% |
| Pill endometrium | 1 | 1 | 4 | 6 |
| 1.2% | .8% | 3.1% | 1.8% |
| Atrophic endometrium | 3 | 5 | 22 | 30 |
| 3.6% | 4.2% | 17.1% | 9.1% |
| Disordered proliferative endometrium | 6 | 11 | 13 | 30 |
| 7.2% | 9.3% | 10.1% | 9.1% |
| Simple hyperplasia without atypia | 12 | 10 | 12 | 34 |
| 14.3% | 8.5% | 9.3% | 10.3% |
| Complex hyperplasia without atypia | 2 | 13 | 7 | 22 |
| 2.4% | 11.0% | 5.4% | 6.6% |
| Endometrioid adenocarcinoma | - | - | 21.6% | 2 |
| .6% |
Discussion
The leiomyomas are the most common benign tumours of the uterus in the reproductive and post menopausal age group. This is of importance owing to the fact that they are the most common cause for hysterectomies in the women in the reproductive age group. In the current study, out of 1463 hysterectomy specimens in two years 331 (22.62%) hysterectomies had leiomyomas. Cramer SF et al., observed 77% of hysterectomies are due to leiomyomas and Velu ARK et al., observed it to be 28% and Jha R et al., found it to be 28% [1,7,8].
Leiomyomas most commonly occur in the mid reproductive age group women. Baird DD et al., in their study of randomly selected women between 31-49 years found that the incidence of uterine fibroids was 60% by age 35 years which increased to 80% by age 50 years in African-American women and for Caucasian women by 35 years of age the incidence of uterine fibroids was 40% and by age 50 years it was found to be 70% [9]. In this study, it was observed that majority of the cases (56.50%) were seen in the age group of 41-50 years and 84.29% cases were seen in age group between 31-50 years. This is in concurrence with the studies of Gowri M et al., Velu ARK et al., and Begum S et al, [2,3,7]. In this study it was also observed that 20.54% cases were post-menopausal, this is in contrast with the findings of Velu ARK et al., who had only 4% of the women who were in the post-menopausal age group [7].
Multiparous women (94.86%) were found to have more leiomyomas compared to primipara and nullipara. This is explained by the fact that multiparous women, acquire increased levels of oestrogen, progesterone and their receptors, ER and PR [10,11].
Most of the women with leiomyomas are asymptomatic, however they most commonly present with menorrhagia. In the current study menorrhagia was seen in 46.53% followed by abdominal pain in 26.89% of cases. These findings are in concurrence with other studies [2,3]. The cause for the predominance of menstrual symptoms could be attributed to the fact of increased vascularity, endometrial surface, altered contractility of endometrium and the hormonal influence of the tumor.
Majority of the cases of leiomyomas were single in number (59.82%). These findings are in agreement with studies of Gowri M et al., and Velu ARK et al., [3,7]. This finding is in contrast with Begum S et al., and Cramer SF et al. who found multiple leiomyomas to be more frequent than single leiomyomas [1,2].
The most common type of leiomyoma encountered was intramural type in 49.85%. These findings are in concurrence with Gowri M et al., and Velu ARK et al., who found that the most common type of leiomyoma to be of the intramural type [3,7].
Secondary changes were observed in 39.27% of the leiomyomas of which the commonest secondary change was found to be hyaline change observed in 23.87% of the leiomyomas. This is in agreement with the observations of Gowri M et al., Begum S et al., and Persaud V et al., [2,3,12].
In the current study,110 (33.23 %) leiomyomas were associated with adenomyosis. This is in contrast with Ben AN et al., who reported 62 % of cases of leiomyoma with adenomyosis and Raju GC et al., who reported 16 % of leiomyomas with associated adenomyosis [12-14]. In the current study it was observed that adenomyosis was most commonly seen in multiparous women and in the age group of 30-50 years as observed by other Raju GC et al., and Velu ARK et al., [7,13].
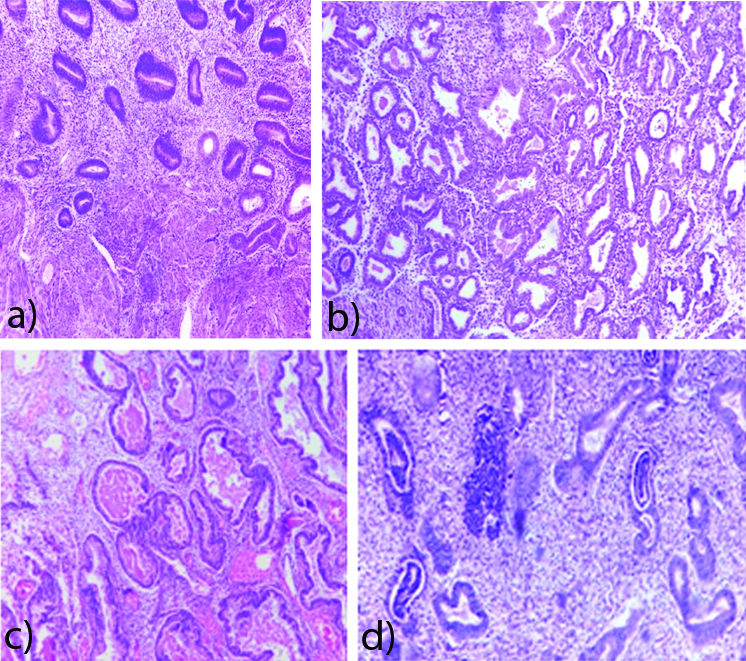
The most common type of endometrium associated with a leiomyoma was proliferative endometrium observed in 44.41% of which the late proliferative endometrium was the predominant type in 41.38% and early proliferative in 3.02%. This is in concurrence with Velu ARK et al., and Gowri M et al., [Table/Fig-5] [3,7].
Proliferative endometrium (100x-H&E); b) Early secretory endometrium (100x-H&E); c) Late secretory endometrium (100x-H&E); d) Disordered proliferative endometrium (100x-H&E).
Hyperplasia of endometrium was seen in 16.92% of the cases of which 10.27% of the cases showed simple hyperplasia without atypia and 6.64% of the cases showed complex hyperplasia without atypia. The findings of the current study is in contrast with the studies of Velu ARK et al., Gowri M et al., and Chethana M et al., who found hyperplastic changes in 25%, 22% and 24% respectively [3,7,11] [Table/Fig-6].
Simple hyperlasia without atypia (100X-H&E); b) Complex hyperlasia without atypia (100x-H&E); c) Endometrioid adenocarcinoma (100x-H&E).
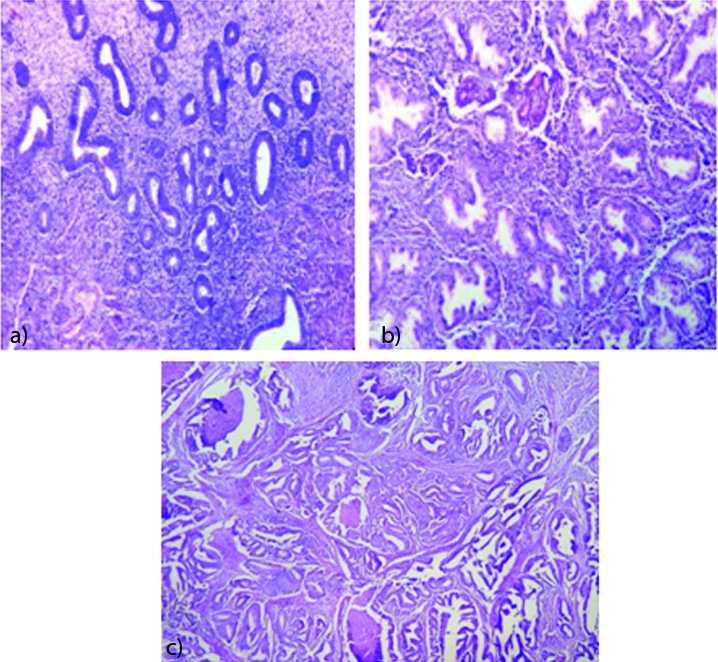
Atrophic endometrium was seen in 9.06% of the cases and disorderly proliferating endometrium in 9.06% of cases of leiomyoma. This is in concurrence with the studies of Velu ARK et al. whereas Gowri M et al., and Chethana M et al., had observed more percentage of cases with atrophic changes probably due to more cases of submucosal fibroids in both the studies which cause pressure effects on the endometrium leading to atrophy [3,7,11]. Atrophic endometrial changes are not only due to pressure effects but also due to post menopausal hormone insufficiency [6].
In this study of the 331 cases, 88 cases (26.58%), showed abnormal endometrial changes. The most frequent abnormality was simple hyperplasia without atypia. Teleman S et al., who proposed that leiomyoma and endometrial hyperplasia, develop in a hormonal context. The risk is higher in the perimenopausal period. The most frequent abnormality in endometrium is simple hyperplasia suggesting a rare progression to highest grades and a possible protective role of leiomyoma as target tissue which capture oestrogens [15].
It was also observed that 159 cases (48.03%) of the total 331 cases showed persistence of the proliferative phase beyond 15 days of the LMP. This shows that leiomyomas are also associated with a persistent proliferative endometrium, which is due to a hyper-oestrogenic effect. This hyper-oestrogenic effect could be a common factor contributing to the leiomyoma and the endometrial changes as noted by Velu ARK et al., [7].
The probable cause for the endometrial changes could be oestrogen, progesterone and pressure effects, in cases of submucosal fibroids. Deligdish L et al., concluded that there is high oestrogen level in women with fibroids and it is hypothesised that oestrogen is synthesised by the endometrium which is responsible for the growth of the fibroid [6]. Oestrogen and progesterone together play a role in fibroid growth [7]. The oestrogen up regulates both oestrogen receptors and progesterone receptors in the fibroids during proliferative phase which is followed by the progesterone induced mitogenesis during the luteal phase [16].
Study by Gull B et al., has shown that the tissue concentration of oestrogen receptor and progesterone receptor were more in the leiomyoma when compared with the normal myometrium [16].
The endometrium is under the cyclical influence of the steroid hormones. There is an entity called the sub-endometrial myometrium which also undergoes cyclical steroid receptor changes in concurrence with the endometrium during the menstrual cycle [17]. There is growing evidence that the leiomyomas are benign tumours arising from this sub-endometrial myometrium Hence the leiomyomas, arising from the sub-endometrial myometrium, also show cyclical changes in the oestrogen and progesterone receptors, during the menstrual cycle, which adds to the evidence that the leiomyomas are not only steroid dependant for their growth but occur in concurrence with the changes in the endometrium [5,18]. So, it could be said that, oestrogen and progesterone are common factors affecting the leiomyoma and the endometrium.
Limitation and Recommendations
The limitations of this study is the lack of IHC for ER, PR to demonstrate the hormonal dependency of the leiomyoma. This could be carried out in the future to ascertain the fact of leiomyoma consuming the steroid hormones and thereby protecting the endometrial influence of these hormones. A study of the subendometrial myometrium could also throw more light on the pathogenesis of a leiomyoma.
Conclusion
Leiomyoma (22.62%) was the commonest condition noted in hysterectomy specimens and 33.23% of leiomyomas had associated adenomyosis which suggests the hormonal dependency of these tumours. Abnormal endometrial changes do tend to occur in concurrence with a leiomyoma, as they constituted nearly one-fourth of the cases. Most of these endometrial changes occur due to a hyper-oestrogenic status which is substantiated by the persistent proliferative phase seen beyond 15 days of LMP in 48.03% of cases, which also explains the various menstural disturbances that the patients present with in a leiomyoma. A 10.3% of the cases showed simple hyperplasia without atypia and only 6.66 % showed complex hyperplasia without atypia of endometrium. There were two cases of leiomyoma with endometrial carcinoma. This study thus shows that the leiomyomas have a protective role on the endometrium. Thus, a proliferative endometrium beyond 16 days of LMP in a endometrial curettage sample could also be considered to be due to a leiomyoma and thereby can be treated with harmone therapy or simple myomectomy, thereby a hysterectomy can be avoided in these patients if detected early.