Probiotics are live micro-organisms which upon ingestion result in health benefits in the host. The term probiotic was coined in 1965 by Lilly and Stillwell [1]. Probiotics are ingested through food supplements like pharmaceuticals, dairy products, fruit juices etc.
Randomised clinical trials have already shown that these bacteria can be used as preventive and therapeutic agents for gastro intestinal ailments and vaginal infections in the host [2, 3].
These bacteria competitively grow and inhibit the harmful bacterias in the oral cavity causing caries, periodontal problems, and yeast infections. Studies have also proved that the probiotics effectively modulate the immune response and secrete antimicrobial substances to curb the pathogenic bacteria growing intraorally [4]. The benefits of the probiotic bacteria are strain specific, therefore a combination of strains are preferred. Most commonly used strains are Lactobacillus and Bifidobacterium [5].
Advantages of probiotics include improvement in the gastrointestinal system improving the overall health of the host. Probiotics, therapeutically combat diarrhea in children, relieve lactose intolerance and inflammatory bowel disease. They have been suggested as a preventive measure for colorectal cancer, regulatory means for blood pressure and suppressing cholesterol levels. Despite being strongly recommended with proven benefits, they are contraindicated in patients who are allergic to specific strains or lactose intolerance, and cardiac valve disease. There are not many disadvantages of probiotics other than sporadic gastrointestinal symptoms, systemic infections, excessive immune stimulation in susceptible individuals and gene transfer [6].
Candidiasis of oral cavity in denture wearers is common especially in palatal region, if the dentures are worn for longer period of time [7]. Once the patients are infected by candida, antifungal therapy is started which has deleterious side effects on gastro intestinal system. [8]
Therefore, much research has been dedicated towards preventing the colonisation of candida on the surfaces of denture and mucosal surfaces [9]. Antifungal denture forming materials are underway to prevent candidiasis [10]. Between the searches, Probiotics have emerged as a boon to dentistry. Probiotics have shown benefit when used systemically as well as used intra- orally in geriatric patients [11]. Research has increased in this direction of utilising the inherent antifungal and antibacterial properties of probiotics, when used locally in the oral cavity [12].
Denture adhesives play a supplemental role in increasing the retention and stability of dentures in edentulous patients. Not only in compromised situations but in well- formed ridges where patients expectations from the prosthesis are too high [13] . These products are bought over-the-counter and sometimes clinically indicated, therefore they are used widely by the patients.
Many times completely edentulous patients, even after receiving a well-made prosthesis are not satisfied with its retention and stability [14]. The conditions like highly resorbed ridges, very high mucosal attachments, flabby ridges, inability to utilise the neuromuscular control to hold the denture due to muscular disorders, or unable to visit the dentist for fabrication of a new denture due to senility are situations where the retention and stability are compromised [15]. In such situations, fabricating implant supported dentures may provide the necessary retention and stability expected from the prosthesis [16]. But at times due to systemic conditions and economic constraints of the patient, it is not feasible to fabricate such a prosthesis. In such situations, denture adhesives can play an important role in the retention of the prosthesis [17].
Along with the use of adhesives, denture hygiene maintenance is of prime importance. The lack of hygiene maintenance, propagates the opportunistic behaviour of candida causing Denture stomatitis. Therefore this study was planned to evaluate the effect of probiotics when used along with Denture adhesives on colony forming units of candida in denture wearing patients. For this purpose the probiotics were added to denture adhesives and this product was tested for its stability. The aim of the study was to evaluate and compare the colony forming units of candida, after using plain and probiotic added denture adhesive, in denture wearing patients. Null hypothesis of the study was that, there was no difference in colony forming unit of candida after using plain and probiotic added denture adhesive.
Materials and Methods
The study was a double-blind randomised clinical crossover trial conducted at Department of Prosthodontics, K M Shah Dental College and Hospital, on completely edentulous patients visiting the OPD. According to the patient enrollment, the study was conducted over six months i.e. March 2017 to August 2017.
The sample size of the study (n) was calculated based on the number of completely edentulous patients reporting per month to the department OPD (N) after using the formula:
n=N/1+Ne2where N is Population size and e is the level of precision. If N is 60 for a month and e is 0.05. Hence, n was calculated to be 52. To take into the account the dropout rate of 20% as it is clinical trial, therefore n becomes 65. The power of the study was 80% with level of significance 0.05 and 95% confidence interval.
The inclusion criteria for the study was completely edentulous patients who were asymptomatic candida carriers with no candida infection, who were not on any antibiotics, probiotics or antifungal treatment. Patients with lactose intolerance, patients suffering from chronically debilitating disorder including gastrointestinal disorders, heart ailments, intolerance to milk and any patient who were not willing to be part of the study were excluded.
The ethical clearance for the study was obtained from institutional ethics committee and the study was registered with CTRI with Reg no. CTRI/2017/04/008314. Informed consent was obtained and patient information sheet was given to the participants of the study.
Adhesive Formulation
The adhesive was manufactured specially for the study which did not contain any preservatives or antimicrobials {Lot No.RD/FX 04}. Three strains of probiotic bacteria L.rhamnosus HS111, L. acidophilus HS101, and Bifidobacteriumbifidum were purchased from the manufacturers of probiotics (Mitushi Pharmaceuticals, Batch No.PBR1504130). The strength of the probiotic mix was kept at 108CFU. 3 gms of probiotic powder was added to 15 gm of denture adhesive. (Fixon, brand ICPA Health Product Ltd., GIDC, Ankleshwar, Gujarat). The viability of the probiotics was tested by the manufacturer of the denture adhesive (ICPA) according to ICH guidelines [18] [Table/Fig-1].
Stability test data for the combination of adhesive and probiotic.
| ICPA Health Products Limited 286/287, GIDC, Ankleshwar-393002 |
|---|
| Department: Research and Development | Format No.: RD/SP/052/A2 |
|---|
| Stability study data |
| Product: Probiotic Mucoadhesive powderB.No.: RD_FX_02Pack size: 15 g PET bottlesMfg. Date: 9.10.2015Packaging Date: 9.10.2015 | Batch Size:100 g Label claims: 15% of blends of Lactobacilus acidophilus, Lactobacilus rhammosus, Bifidobacetrium bifidum. Storage condition: As per SOP No.RD/SP/52R1.Test Method: As per RD/SS/BP/13/10 |
| Testprotocol | Limits | Initial | CONDITIONS | 1 M | 2 M | 3 M |
| Description | An off white free flowing fine powder having characteristic flavor | An off white free flowing fine powder having characteristic flavor | 25±2°C/65±5 %RH | OK | OK | OK |
| 30±2°C/65±5 %RH | OK | OK | OK |
| 40±2°C/75±5 %RH | OK | OK | OK |
| Total Probiotic count | 4 to 6 CFU | 5 CFU | 25±2°C/65±5 %RH | 4 | 3 | 2 |
| 30±2°C/65±5 %RH | 4 | 2 | 2 |
| 40±2°C/75±5 %RH | 4 | 2 | 2 |
| Adhesion power | 3.5 to 6.0 kg | 4.6 kg | 25±2°C/65±5 %RH | 4.5 | 4.5 | 4.3 |
| 30±2°C/65±5 %RH | 4.6 | 4.3 | 4.2 |
| 40±2°C/75±5 %RH | 4.4 | 4.3 | 4.1 |
The study being double-blind RCT, the principal investigator and the patient were kept blinded to the study. Principal investigator was blinded as the entire allocation and assignment of intervention of the participants was carried by the staff nurse. Each patient received an identification number and was randomly allocated to 1 of the 2 intervention groups. Computer generated random numbers was used for random allocation. Allocation concealment of the assigned intervention was done with use of similar appearing bottles of adhesives. Staff nurse enrolled the participants and assigned them to their respective interventions. Codes were sealed in opaque envelop and decoded at the time of statistical evaluation.
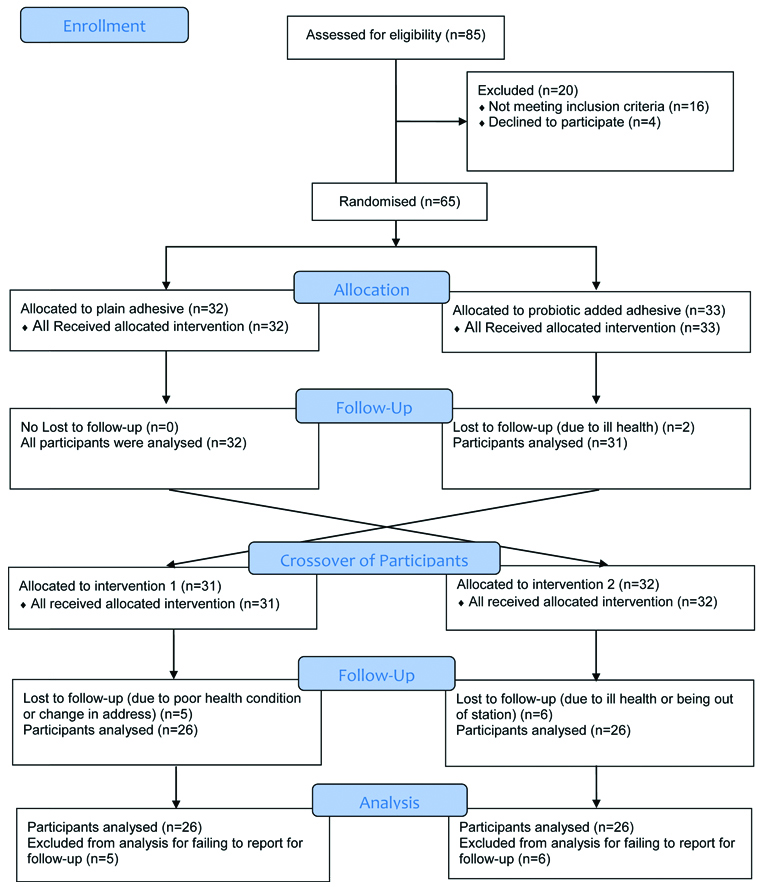
Trained operators performed the procedure of fabricating the complete denture prosthesis. [Table/Fig-2] shows the flow diagram of the study.
Flow diagram of the study
Before recruitment of the participants they were evaluated for CFU/mL of candida after taking the palatal swab, if found asymptomatic (2-888 CFU/mL) they were enrolled in the study. [19]. This count of CFU/mL obtained for the first time, was recorded as the Baseline Data.
The entire Baseline observations for CFU of candida were made before the denture insertion. A palatal swab was obtained from each participant by rubbing a swab for 10 seconds on the palatal mucosal surface. The swab was serially diluted in phosphate- buffered saline and inoculated on the surface of Sabouraud Dextrose Agar (SDA) plates with 100 mg chloramphenicol/. After incubation for 24 to 48 hours, colonies were counted, and the number of CFU/mL was determined with Digital colony counter [20].
After recruitment of the patients at the baseline, according to inclusion and exclusion criteria, they were randomly allocated to the two groups.
Group A received a regular denture adhesive in powder form and the other Group B received a probiotic added denture adhesive in the powder form as well, at the time of insertion of the denture. Each participant was taught to sprinkle the provided denture adhesive five times on the intaglio surface of the maxillary and mandibular denture on each application from the bottle. Adhesive was supposed to be applied three times a day for five weeks. A count of five sprinkles was decided upon to regularise the amount of powder sprinkled by the participant each time. Participants were recalled after five weeks and second time palatal swab was taken again for counting the CFU of Candida.
After a wash out period of one week, a crossover of patients was done. Participants in group A were crossed over to Group B and vice versa. After a 5-week experimental period, participants were recalled and analysed for CFU/mL for the third time.
Statistical Analysis
Statistical test applied were descriptive statistics, Repeated Measures ANOVA, Bonferroni adjustment for Pairwise comparison among the groups using SPSS Version 21. The parameter to be evaluated was CFU/mL at baseline and in each group.
Results
The present study enrolled 65 edentulous patients aged 60 years and above of which 25% were females. The baseline demographic and clinical characteristic are shown in [Table/Fig-3]. 32 patients were randomly allocated to Group A after denture insertion who were supposed to use plain adhesive and 33 patients were given probiotic added adhesive for 5 weeks. Two patients were lost to follow-up after first recall due to ill health. Patients were evaluated for CFU/mL after taking palatal swab of the patient.
Baseline demographic and clinical characteristics.
| Age | 60-70 | 70-80 | 80 and above |
| 68% | 26% | 6% |
| Sex | Males | Females | |
| 75% | 25% | |
| Previous denture use | Less than 5 years | 5-10 years | New denture |
| 20% | 23% | 57% |
| Denture hygiene | Poor | Fair | Satisfactory |
| 7% | 46% | 47% |
| CFU/mL | 0-20 | 20-40 | |
| 83% | 17% | |
After a wash out period of one week, a cross-over of the patients was done to either group again for five weeks. At recall the CFU/mL of the patients were evaluated. Another 11 patients were lost to follow-up due to health condition or being out of station. At the baseline, data varied from 10 to 110 with a mean of 59.56±34.36. In group A with plain adhesive, the CFU/mL varied from 20 to 150 with a mean of 70.94±33.56. In Group B, with probiotic added denture adhesive, CFU/mL ranged from 8 to 96, a mean of 51.07±26.85. [Table/Fig-4]. The mean CFU/mL showed marked reduction in probiotic added denture adhesive. Data tabulated pre cross over for Group A and Group B is shown in [Table/Fig-5]. After crossover of the patients and considering the loss to follow-up, the data is shown in [Table/Fig-6]. [Table/Fig-7] shows Mauchly’s Test of Sphericity indicating the assumption of sphericity is fulfilled, χ2 (2)=1.023, p<0.05, and therefore, a Greenhouse-Geisser correction was used. There was a significant effect of different interventions in the form of plain adhesive and probiotic added adhesive in the Colony forming units, F=58.090, p<0.001.
Descriptive Statistics of the CFU/mL among the three groups.
| Descriptive statistics |
|---|
| Groups | N | Minimum | Maximum | Mean | Std. deviation |
|---|
| CFU/mL at Baseline | 65 | 10.00 | 110.00 | 59.5636 | 34.36016 |
| CFU/mL with plain adhesive (Group A) | 58 | 20.00 | 150.00 | 70.9455 | 33.56443 |
| CFU/mL with probiotic added adhesive (Group B) | 57 | 8.00 | 96.00 | 51.0727 | 26.85962 |
Precross over CFU/mL in Group A and Group B.
| Descriptive statistics |
|---|
| N | Minimum | Maximum | Mean | Std. deviation |
|---|
| CFU/mL with plane adhesive | 32 | 22.00 | 120.00 | 67.0938 | 31.50152 |
| CFU/mL with probiotic added adhesive | 31 | 8.00 | 96.00 | 49.1563 | 28.06572 |
Post cross ove rCFU/mL in Group A and Group B.
| Descriptive statistics |
|---|
| N | Minimum | Maximum | Mean | Std. deviation |
|---|
| CFU/mL with plane adhesive | 26 | 22.00 | 120.00 | 65.3846 | 31.39054 |
| CFU/mL with probiotic added adhesive | 26 | 10.00 | 96.00 | 49.9231 | 27.65201 |
Repeated measures of ANOVA with Mauchly’s analysis.
| Repeated measures ANOVA |
|---|
| Within subjects effect | Mauchly’s W | Approx. Chi-square (df, pvalue) | Greenhouse-Geisser |
|---|
| Type III sum of squares | Df | F | p-value |
|---|
| Colony_Forming_Units | .981 | 1.023 (2, 0.600) | 10937.055 | 1.962 | 58.090 | ≤0.001 |
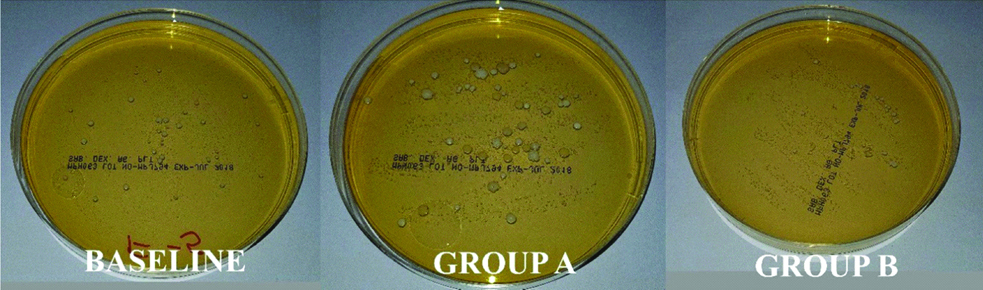
Dextrose agar plates at baseline, Group A and Group B of the same patient are shown in [Table/Fig-8]. The Bonferroni Adjustment for the CFU/mL among the three groups show that there was no statistically significant reduction in CFU/mL between baseline and when plain adhesive is used. The mean difference, however, in these two stages was high showing that there is an increase in CFU/mL when plain adhesive is used compared to CFU/mL at baseline by 11.382. The difference between CFU/mL was found to be statistically significant in cases where probiotic is added in the adhesive as the p value is less than 0.001. As seen in [Table/Fig-9], the mean difference between these two groups was 19.873, which shows that the reduction in CFU/mL after adding probiotic in adhesive was also statistical significant from CFU/mL when plain adhesive was used. Similar statistically significant result was also observed between the CFU at baseline and when probiotic is added in adhesive. The mean difference between the CFU/mL at baseline and when probiotic is added to the adhesive was 8.491, which was also statistically significant having p<0.05.
Colony forming unit of candida at baseline, with plane adhesive and probiotic added adhesive.
Shows the results for Bonferroni adjustment showing the Pair wise Comparisons in three groups (*denotes that these values are considered significant at 0.05 level).
| Pair wise comparison of the three groups |
|---|
| (I) Colony_Forming_Units | (J) Colony_Forming_Units | Mean difference (I-J) | Std. error | p-value | 95% Confidence interval for difference |
|---|
| Lower bound | Upper bound |
|---|
| CFU/mL at Baseline | CFU/mL with plane adhesive (Group A) | -11.382* | 1.920 | 0.345 | -16.125 | -6.638 |
| CFU/mL with probiotic added adhesive (Group B) | 8.491* | 1.906 | ≤0.001 | 3.781 | 13.200 |
| CFU/mL with plane adhesive (Group A) | CFU/mL at Baseline | 11.382* | 1.920 | .345 | 6.638 | 16.125 |
| CFU/mL with probiotic added adhesive (Group B) | 19.873* | 1.718 | ≤0.001 | 15.628 | 24.117 |
| CFU/mL with probiotic added adhesive (Group B) | CFU/mL at Baseline | -8.491* | 1.906 | ≤0.001 | -13.200 | -3.781 |
| CFU/mL with plane adhesive (Group A) | -19.873* | 1.718 | ≤0.001 | -24.117 | -15.628 |
Discussion
Candida being a commensal in the oral cavity turns into an opportunist due to various supporting factors. Age and diminishing immunity, improper oral hygiene, systemic disorders being few among the factors. Patients with complete denture prosthesis always show tendency to develop denture stomatitis when they are not able to maintain the prosthesis [21]. The situation may worsen with adhesives use, when added as a layer on the dentures to improve its function [22]. Once the patients suffers from candidiasis, irrational use of antifungals lead to various side effects like Gastrointestinal problems [8]. Therefore, this study was planned to evaluate the effect of Probiotics when used locally with the denture adhesives on colony forming units of candida in the oral cavity of a denture wearer.
Probiotics are living microorganisms when ingested in appropriate strengths bring positive health changes in the host. Probiotics have proved to be beneficial against the pathogenic bacteria and genus Candida in oral cavity [23]. There are several mechanisms by which these noble bacteria hinder the growth of the pathogens. A few mechanism are by competing, antagonising, and altering immune response of the host. Evidence suggesting protective role of probiotics on elderly individuals allow their use in topical applications and various formulations to treat oral diseases [11]. Hence the following study was carried out to evaluate the combination of probiotics added to Denture Adhesives.
Denture Adhesives have been used over the years now to enhance the stability and retention of dentures [24]. They are short and long acting synthetic polymers. Molecules of adhesives swell up to fill the spaces between denture and mucosa. They also increase the cohesive force by increasing the interfacial tension when the denture is tried to be pulled away from mucosa. Evidence has shown that the adhesives are beneficial under many circumstances [25]. Not only are they effective in poor ridge cases but also in good ridges. On one hand they improve the retention and stability of denture in a poor ridge cases and on the other hand it improves satisfaction in well-built ridges. Adhesives can also be utilised as a means to improve retention in poor muscular control due to nerve damage in stroke or chronic debilitating disorders. Denture adhesives provides the necessary lubrication in aged thin mucosa, preventing abrasion and entry of food particles beneath it. Not only objective measures like quality of life studies but also objective measures like kinesiographic studies and electromyographic studies have also proved that denture adhesives enhance the retention and stability of the dentures [26]. Evidence based guidelines state the judicious use of adhesives is beneficial to the denture wearers [27].
Studies have shown that the colony forming units of candida does not increase after using adhesives [28]. Though few studies reported that adhesives can increase the number of candida infection in the mouth. The results of this study are similar to the studies done earlier where there is no statistically significant increase in colony forming units of candida (.345) from baseline to using adhesives. A small amount of increase in candida depends upon how well the patients practice hygiene. The colony forming units may increase even if small adhesive remains stuck to the intaglio surface of denture [29]. The colony forming unit of candida decreased after probiotics are added to denture adhesives as seen in the present study [Table/Fig-4].
The probiotics act on pathogens by several mechanisms for the advantage of the host [30].
They enhance the host defence by increasing their immunity against the pathogens. Studies show that probiotics help friendly bacteria to rise in number [31]. They release certain chemicals like organic acids, hydrogen peroxide, and bacteriocins [32]. The precise mechanism by which this occurs is still being studied. Probiotic bacteria hinder the survival of the pathogens and affect their virulence on the host [33]. They compete for nutrients and adhesion sites with the pathogens on the host, thereby directly affecting their pathogenicity [34]. Pathogens harm the host by forming a biofilm on its surface, which is also deterred by probiotic bacteria [35]. Murzyn A et al., have inferred that Capric acid is the main product that hinders hyphae formation in the yeast [36]. Kohler GA et al., concluded that lactic acid at low pH affect biofilm formation [37]. According to Kheradmand E et al., the release of exometabolites hinders candida growth [38]. Ujaoney carried an in vitro study and stated that the lack of nutrients for candida due to overgrowth of probiotic bacteria prove harmful for candida growth [39].
Similarly there are some of clinical studies which have yielded similar results as obtained in this study. Mendonca FH did a study on women, the results showed 92.9 to 85% reduction in candida after using probiotics [40]. Studies conducted by Hatakka K and Ishikawa KH have shown in their studies that how oral intake and local application of probiotics reduce amount of CFU/mL in the oral cavity [11,20].
Matsubara VH et al., conducted a study to understand the mechanism of action of the probiotics in altering the host immunity [35]. They studied that how the expression of pattern-recognition receptors genes is altered (CLE7A, TLR2, and TLR4) with probiotic treatment. Macrophages which were treated with probiotics showed lesser production of Dectin-1. The lactate released by lactic acid bacteria (LAB) interferes with purpose of macrophages and dendritic cells and alters the inflammatory response of epithelial cells.
According to the results of the study, it can be inferred, the probiotics can alter the host immunity and decreases the number of candida in the oral cavity even in asymptomatic candida carriers. Therefore probiotics can have prophylactic effect in patients who are prone to suffer from oral candidiasis and can also be used as an adjuvant in therapy of people suffering from oral thrush. The new combination of probiotics added to denture adhesives if used can serve as a boon for the completely edentulous patients, utilising the advantages of both the products together.
In the present study, regular calls were made to the patients enrolled for the study to make sure that the patients were following the instructions given regarding use of Denture adhesives and would return for follow-up.
Limitation
The limitations of the study was that the stability of the novel combination was tested for just three months only and further studies are required to check the stability of this combination with different range of probiotics and strengths. Also studies need to be carried out in symptomatic patients to assess and compare the efficacy of plain and probiotic added denture adhesive.
This further has the advantage, that the product will not be overly used for a long period of time, as evidence based guidelines studies suggest the use of Denture adhesives for two to three months. Probiotics have the inherent nature of becoming nonviable at higher temperatures and storage conditions.
Conclusion
Within the limitations of the study, it can be concluded that a combination of Denture adhesive and probiotics can be formulated which is stable for three months. Also, the product when used by completely edentulous patients can help in reducing candida. It can be used as an adjuvant to therapeutic measures and as an preventive means to reduce the risk of contacting candidiasis.