Introduction
Cryptococcal infection is the most common opportunistic fungal infection was seen in HIV patients. Despite specific treatment, mortality due to cryptococcaemia still remains high primarily because of late diagnosis. Therefore, studies have recommended that routine screening is cost-effective in patients with CD4 count ≤100 cells/mm3 in areas with cryptococcal antigenemia >0.6%. Prevalence of cryptococcaemia in India is reported to be variable and therefore, whether routine screening for cryptococcal infection is cost-effective or not, cannot be ascertained.
Aim
To find out the prevalence of cryptococcaemia in HIV infected patients with CD4 counts of ≤100 cells/mm3.
Materials and Methods
This was a cross-sectional study, conducted at KEM hospital, Mumbai, India which is a tertiary care hospital, all HIV infected patients with CD4 count ≤100 cells/mm3 coming to the hospital between January 2015 and December 2015 were enrolled. Blood samples drawn were processed for wet mount, negative staining with India ink, gram staining, fungal culture and Cryptococcal Antigen (CrAg) Lateral Flow Assay (LFA) using IMMY LFA Kit. Statistical calculation was done using SPSS software Version 20.0 (SPSS Inc. Chicago, IL, USA) and chi-square and Fisher-exact test was used to compare categorical variables.
Results
Out of 150 patients enrolled, 23 (15.3%) had CD4 count below 50, while 127 (84.7%) had between 51-100. 108 patients (72%) were Anti-Retroviral Therapy (ART) experienced and 42 (28%) were ART naïve. An amount of 53.3% of patients had no opportunistic infections, 27.3% had pulmonary tuberculosis, 11.3% had candidiasis and 8% had extra-pulmonary tuberculosis. Four samples tested positive for LFA giving a prevalence of 2.67%, while none of the cultures were positive for Cryptococcus species. No significant association was seen between age and gender to positive serum cryptococcal antigenemia. However, low CD4 count was found to be strongly co-related to positive serum cryptococcal antigenemia.
Conclusion
This study reveals that cryptococcal antigenemia is a health problem and Cryptococcal antigen screen and treat policy recommended by World Health Organisation should be made routine for HIV patients registering at ART centre in the present setting especially those who are ART naive and have CD4 counts ≤100 cells/mm3.
Introduction
Cryptococcal infection is the most common opportunistic fungal infection in Human Immunodeficiency Virus (HIV) patients. The estimated total number of People Living with HIV (PLHIV) in India was around 21.17 lacs (17.11 lacs-26.49 lacs) in 2015 [1]. Cryptococcal meningitis ranks third in the common opportunistic infections seen in HIV patients [2]; also being a leading cause of mortality among them in developing countries [3]. Despite the arrival and increased availability of specific treatment for cryptococcosis in resource-limited settings, the mortality rate still remains high, particularly in patients with advanced cryptococcal diseases [4,5]. There is a high incidence of cryptococcaemia and mortality before ART initiation. Therefore, to decrease the mortality associated with cryptococcosis in HIV, it is required to detect cryptococcal infection early.
Cryptococcal Antigen (CrAg) is an early stage biomarker for detection of disseminated cryptococcosis in HIV patients and can be seen as early as 234 days prior to meningitis symptoms [3]. CrAg in serum indicates a high chance of disease progression to CM within a year [6]. Serum CrAg performed by the rapid test kit yields high sensitivity and specificity and is a simple method available for the diagnosis of symptomatic cryptococcosis in advanced HIV disease [7-9]. Although, the issue remains as to whether it is cost-effective in resource limited settings to perform this rapid test routinely in all HIV patients with CD4 count <100 cells/mm3. Various studies have concluded that routine screening and pre-emptive therapy is cost-effective among patients with CD4 count <100 cells/mm3 in areas having a cryptococcal antigenemia prevalence of at least 3% or more [5,6,10,11]. World Health Organisation (WHO) in 2011 has also recommended routine Cryptococcus neoformans antigen (CrAg) screening in ART naïve patients with CD4 counts <100 cells/mm3 in population with a high prevalence of cryptococcal antigenaemia (>3%) [12]. WHO guidelines also recognised that earlier initiation of ART stays to be the most important preventive strategy to decrease the incidence of cryptococcal infection and associated high mortality [13]. However, recent studies suggest that the screening may be cost-effective above a prevalence of 0.6% [6,10,12,14]. There is a paucity of literature defining the prevalence of cryptococcal antigenemia in India. Hence, it is important to know the prevalence of cryptococcaemia in the present setting and the need for the routine screening of all patients for CrAg.
Therefore, the study was conducted to find out the prevalence of cryptococcaemia in HIV infected patients with CD4 counts <100 cells/mm3. Also, the utility of rapid test and standard culture method for diagnosis of cryptococcaemia in blood samples was also compared.
Materials and Methods
A cross-sectional study with a sample size of 150 was carried out after taking Institutional Review board permission (EC/196/2014) in the Department of Microbiology of KEM hospital, Mumbai, India which is a tertiary level teaching hospital. HIV infected patients who came for routine CD4 testing between January 2015 and December 2015 were considered for participation in the study. Patients were enrolled in the study after written informed consent and if his/her CD4 count was ≤100 cells/mm3. Patients receiving primary prophylaxis for cryptococcosis or having past history or current cryptococcal infection were excluded from the study as the aim of this study was to find out prevalence of cryptococcaemia removing all confounding factors. A detailed clinical history consisting of complaints, personal history, HIV serotype (HIV I/II), whether on antiretroviral therapy, CD4 count and Opportunistic Infections if any were noted down for all patients.
Blood samples were processed for fungal culture after preliminary microscopic examination, comprising wet mount, negative staining with India ink and Gram’s staining. Cultures were visually examined for growth daily [Table/Fig-1].
*Biphasic agar in bottle with Sabouraud Dextrose agar and Brain heart infusion broth was used for culturing the blood samples of patients in the study.

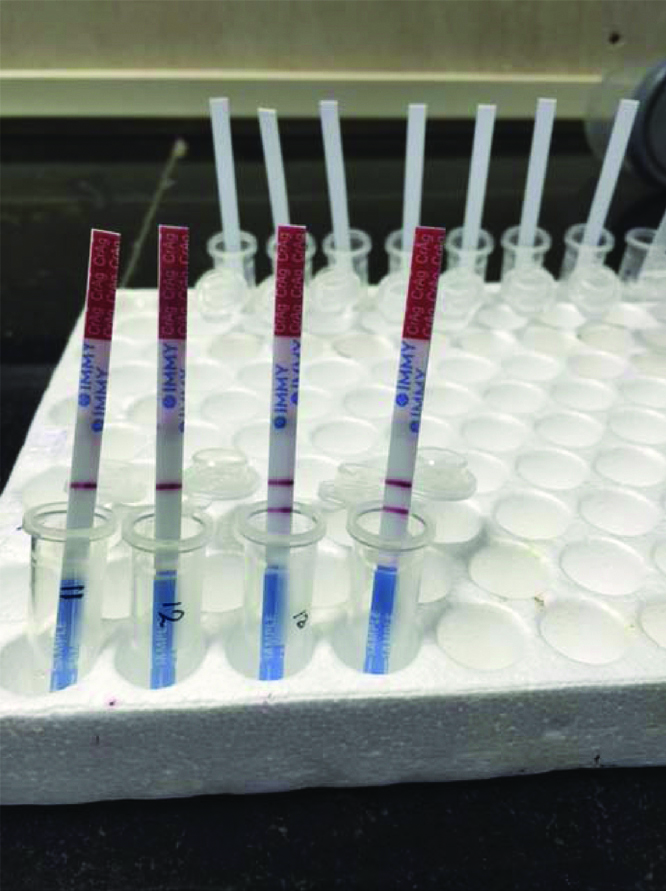
Any growth noticed was stained to observe any yeast cell morphology and sub-cultured onto appropriate media for identification. On gram stain, the round budding yeast cells appeared gram-positive. The colony morphology was noted. Cryptococcus spp was identified based on yeast like mucoid colony on SDA and urease test [15]. None of the culture was positive. The CrAg Lateral Flow Assay IMMY LFA kit (Immuno-Mycologics, Inc., Norman, OK) is a dipstick method which employs sandwich Immunochromatography [Table/Fig-2].
Positive LFA test with positive and negative control.
Statistical Analysis
Statistical calculation was done using SPSS software Version 20.0 (SPSS Inc. Chicago, IL, USA) by consultant statistician. Chi-square and Fisher-exact test was used to compare categorical variables. p-value of ≤0.05 was considered significant. With an expected prevalence of 10% at 95% confidence interval and 5% precision the sample size was calculated with the following formula (n=Z2 P (1-P)/d2), where n=sample size, Z=Z statistic for a level of confidence, P=Expected prevalence of proportion (if the expected prevalence is 20* then P=0.2), d=Precision (If the precision is 5*, then d=0.05).
Results
Of the 150 HIV-infected patients included in the study [Table/Fig-3], mean age was 35.3 years. Majority of patients-108 (72%) were in the age group of 21-40 years. Other than 14 patients who were asymptomatic, 136 patients (90.7%) had some symptoms [Table/Fig-4]. Fever was the most common symptom (70.7%). Out of 150 patients, 23 (15.3%) had CD4 count below 50, while 127 (84.7%) patients had CD4 count range from 51-100. Median CD4 count was 68 [Table/Fig-3].
Baseline characteristics of 150 patients.
| Characteristics | Total (n=150) | Serum cryptococcal antigen positivity as detected by rapid test | p-value |
|---|
| Positive (n=4) | Negative (n=146) |
|---|
| Age* |
| 21-30 | 49 (32.7%) | 1 (25%) | 48 (32.9%) | 0.999 |
| 31-40 | 59 (39.3%) | 3 (75%) | 56 (38.4%) | 0.336 |
| 41-50 | 29 (19.3%) | 0 | 29 (19.9%) | 0.838 |
| 51-60 | 7 (4.7%) | 0 | 7 (4.7%) | 0.999 |
| 61 and above | 6 (4%) | 0 | 6 (4%) | 0.999 |
| Gender* |
| Male | 95 (63.3%) | 3 (75%) | 92 (63.1%) | 0.623 |
| Female | 55 (36.7%) | 1 (25%) | 54 (36.9%) |
| CD4 count* |
| 1-50 | 23 (15.3%) | 3 (75%) | 20 (13.7%) | 0.01 |
| 51-100 | 127 (84.7%) | 1 (25%) | 126 (86.3%) |
| HIV serotype* |
| HIV-I | 143 (95.3%) | 4 (100%) | 139 (97.2%) | >0.999 |
| HIV-II | 7 (4.7%) | 0 | 7 (4.8%) |
| ART status* |
| ART experienced | 108 (72%) | 0 | 108 (100%) | 0.01 |
| ART naive | 42 (28%) | 4 (9.52%) | 38 (90.48%) |
*Chi-square test used
Clinical features of 150 patients.
| Clinical features | Total (n=150) | Serum cryptococcal antigen positive (n=4) | Serum cryptococcal antigen negative (n=146) | p-value |
|---|
| Fever | 106 (70.7%) | 3 (75%) | 103 (70.1%) | 0.99 |
| Cough | 92 (61.3%) | 1 (25%) | 91 (62.3%) | 0.32 |
| Weight loss | 88 (58.7%) | 2 (50%) | 86 (58.1%) | 0.99 |
| Nausea and vomiting | 67 (44.7%) | 2 (50%) | 65 (43.9%) | 0.99 |
| Neck stiffness | 23 (15.3%) | 1 (25%) | 22 (15.1%) | 0.97 |
| Headache | 22(14.7%) | 3 (75%) | 19 (13%) | 0.01 |
| Altered mental status | 17 (11.3%) | 1 (25%) | 16 (10.9%) | 0.77 |
| Seizures | 6 (4%) | 1 (25%) | 5 (3.4%) | 0.30 |
| Visual alterations | 6 (4%) | 0 | 6 (4%) | 0.999 |
*Chi-square test used
A total of 4 out of 150 serum samples tested positive for LFA test giving a prevalence of 2.67% in HIV seropositive patients with CD4 count of ≤100 cells/μL. None of the 150 samples of fungal culture were positive for cryptococci and no fungal elements were appreciated on microscopy in any of the 150 samples. All patients positive for serum cryptococcal antigen test were in the age group of 21-40 years. No statistically significant association was found between age and serum cryptococcal antigenemia. Three males and one female were positive for serum cryptococcal antigen test. There was no statistically significant association between gender and serum cryptococcal antigen positivity (p-value=0.623). Three patients with CD4 counts ≤50 cells/μL and one patient with CD4 counts in range of 51-100 cells/μL were positive for serum cryptococcal antigen. Statistically, significant association was found between low CD4 counts and serum cryptococcal antigenemia (p-value=0.01). A total of 4 out of 42 cases (9.52%) in ART naïve group were positive for serum cryptococcal antigen test. Serum cryptococcal antigenemia was not seen in ART experienced group. A statistically significant association was seen with serum cryptococcal antigen positivity and ART. (p-value=0.01). All 4 patients positive for serum cryptococcal antigen test were positive for HIV-1 antibodies. No statistically significant association was seen with HIV serotype and cryptococcaemia. (p-value >0.999).
Discussion
Cryptococcal Meningitis (CM), a late and disseminated form of cryptococcal infection, leads to substantial morbidity and mortality among HIV-infected individuals [1,3,16,17]. Severely immunocompromised HIV-infected individuals with a CD4+T-lymphocyte (CD4) count of ≤100 cells/mL are at greatest risk for developing CM [10]. Treatment of CM especially in resource limited settings are often difficult as it requires hospitalisation, expensive intravenous antifungal therapy and monitoring [17]. Those who survive frequently suffer from long-term severe neurological complications because of uncontrolled rise in intracranial pressure during the disease progression [18]. Therefore, it is of utmost importance to detect cryptococcal infection early through routine screening for cryptococcal antigenemia.
Prevalence of serum CrAg in persons with advanced HIV infection ranges between 1% and 19% in sub-Saharan African and Southeast Asian countries [5,6,10,12,14,19-21]. Patel S et al., also reported a prevalence of 5% in a study conducted in London [22]. Many countries have shown interest in CrAg screening and early treatment; a few countries like South Africa, Rwanda, and Mozambique, are already implementing such programs [23]. In the current study, the prevalence of cryptococcal antigenemia was 2.67%. The disparity in the prevalence may be due to seasonal variations or the variable intensity of the presence of cryptococcal species in the local environment.
Currently, WHO recommends CrAg screening in ART naive individuals with CD4 count below 100 cells/μL [12]. In the present study, 108 cases (72%) enrolled were receiving ART and 42 cases (28%) were ART naïve. However, all four cases positive for serum cryptococcal antigenemia were ART naïve and the difference was statistically significant (p-value=0.01). The CrAg positivity in ART naïve patients was 9.52% which is much higher than the 3% recommended by WHO [13]. Hence, CrAg screening may be considered in the present setting especially for ART naive patients with low CD4 counts on a priority basis as it is known to bring down the mortality, morbidity and is cost-effective. Recent analyses have reported that screening may be cost-effective even at a prevalence as low as 0.6% [6,10,12,14]. And as the overall prevalence in the present study is 2.67%, routine screening for all patients irrespective of ART status might be considered at a later date.
Currently, culture is considered as the gold standard for diagnosis, its demerits include poor sensitivity, requirement of a large quantity of specimens and laboratory infrastructure [24]. Studies report a blood culture sensitivity of 47-70% in detecting cryptococcal meningitis [25,26]. Blood culture was used to detect the presence of Cryptococcus in our study population. Sivasangeetha K et al., has reported a case of blood culture positive and CSF culture negative cryptococcosis [27]. However, none of the blood cultures in the present study were positive for Cryptococcus, limiting its use for the screening of Cryptococcus.
The lateral flow assay used in the current study is user friendly. Refrigeration of the test materials or cold chain transport or any specimen pre-treatment is not required and accessibility of LFA is much more in resource limited settings.
In the present study, the median age of the patients enrolled was 33 (21-66 years) which is similar to the studies conducted by Micol R et al., (median age 35 years) and Oyella J et al., (median age 32 years), Oladele RO et al., (median 40 years) [5,20,21]. In the HIV infected individuals, rate of hospitalisation per million total population peaks in the 31-40 age range [28]. The present study also revealed that age group of 21-40 years was most commonly affected though not significantly which may reflect a difference of exposure and outdoor activity rather than a difference in host susceptibility as it was noted earlier [29].
No statistically significant association of gender to serum cryptococcal antigen positivity was found in the current study which is similar to that reported by Pongsai P et al., Patel S et al., and Manga NM et al., [10,19,22]. Ogba OM et al., and Osazuwa F et al., reported higher prevalence rates amongst females but the difference was not significant [30,31]. Micol R et al., reported that male gender was independently associated with positive serum cryptococcal antigen positivity [5].
HIV is characteristically associated with T lymphocyte depletion and subsequent opportunistic infections. Lower the CD4 counts higher the probability of developing infection. In the present study, there was a significant association of CD4 count ≤50 cells/μL with serum cryptococcal antigenemia (p-value ≤0.05). Similar findings have been reported by Micol R et al., and Osazuwa F et al., [5,31]. Out of 150 cases included in the study, HIV-1 serotype was detected in 143 cases (95.4%) whereas HIV-2 serotype was detected in only seven cases (4.6%). All the four cases who had positive serum cryptococcal antigen test were also positive for HIV-1 antibodies but no statistically significant association was found with cryptococcal antigenemia and HIV serotype. Similar findings have been reported by Manga NM et al., [19].
Participants in the current study were severely immunocompromised and more prone to AIDS related complex and opportunistic infections. In the present study, symptoms were seen in 136 of the 150 patients. However, Magambo KA et al., reported symptoms in 35 out of 140 patients which can be attributed to inclusion of HIV positive patients with CD4 count ≤200 cells/μL in their study [32].
Significant association between cryptococcal antigenemia and fever, meningeal signs, altered consciousness, neck stiffness, neck pain and low body mass index has been reported by various authors [5,11,14,20,21]. In the current study, a significant association was observed between headache and positive cryptococcal antigenemia (p=0.01). Micol R et al., also reported a significant association but have stated that headache should not be considered as a specific symptom of CM [33]. These findings suggest that symptoms alone are not good indicators for identifying patients to be tested for cryptococcal antigenemia and a systematic screening may yield better results. TB is the manifestation of AIDS in >50% of cases in developing nations [34]. In the current study 35.3% of patients had tuberculosis [Table/Fig-5]. Also, 2 out of 4 cases had concurrent cryptococcal antigenemia and tuberculosis in our study (50%). The present findings are concurrent with those of Pongsai P et al., and Andama AO et al., [10,35]. These findings suggest that in a developing country like ours, tuberculosis remains the most common co-infection in PLHIV.
Opportunistic infections seen in 150 patients.
| Opportunistic infections* | Total (n=150) | Serum cryptococcal antigen positive (n=4) | Serum cryptococcal antigen negative (n=146) | p-value |
|---|
| No | 80 (53.3%) | 1 (25%) | 79 (52.7%) | 0.42 |
| Pulmonary tuberculosis | 41 (27.3%) | 2 (50%) | 39 (26.7%) | 0.99 |
| Candidiasis | 17 (11.3%) | 1 (25%) | 16 (10.9%) | 0.77 |
| Extra-pulmonary tuberculosis | 12 (8%) | 0 | 12 (8.2%) | 0.99 |
*Chi-square test used
Prevalence of cryptococcaemia in India is reported to be variable and this study reports it to be 2.67% [36,37].
Limitation
Cryptococcal antigen titer were not performed and cryptococcal selective culture media was not used. A prospective study is required to know the impact of this policy on the morbidity, mortality and cost benefits.
Conclusion
The present study reveals that cryptococcal antigenemia is a health problem and Cryptococcal antigen screen and treatment policy recommended by World Health Organisation should be made routine for HIV patients registering at ART centre in the present setting especially those who are ART naive and have CD4 counts ≤100 cells/mm3 by rapid point of care assays.
*Chi-square test used
*Chi-square test used
*Chi-square test used
[1]. India HIV estimations 2015. Technical Report. NACO & National Institute of Medical Statistics, ICMR. Ministry of Health & Family Welfare, Government of India, New Delhi. Available from: http://www.naco.gov.in, accessed on December 17; 2016 [Google Scholar]
[2]. Louie JK, Chi NH, Thao le TT, Quang VM, Campbell J, Opportunistic infections in hospitalized HIV-infected adults in Ho Chi Minh City, Vietnam: a cross sectional studyInt J STD AIDS 2004 15:758-61.10.1258/095646204239515915537464 [Google Scholar] [CrossRef] [PubMed]
[3]. French N, Gray K, Watera C, Nakiyingi J, Lugada E, Moore M, Cryptococcal infection in a cohort of HIV-1-infected Ugandan adultsAids 2002 16(7):1031-38.10.1097/00002030-200205030-0000911953469 [Google Scholar] [CrossRef] [PubMed]
[4]. Jongwutiwes U, Kiertiburanakul S, Sungkanuparph S, Impact of antiretroviral therapy on the relapse of cryptococcosis and survival of HIV-infected patients with cryptococcal infectionCurrent HIV Research 2007 5(3):355-60.10.2174/15701620778063655117504178 [Google Scholar] [CrossRef] [PubMed]
[5]. Micol R, Lortholary O, Sar B, Laureillard D, Ngeth C, Dousset JP, Prevalence, determinants of positivity, and clinical utility of cryptococcal antigenemia in Cambodian HIV-infected patientsJ Acquir Immune Defic Syndr 2007 45(5):555-59.PubMed PMID: 1757712410.1097/QAI.0b013e31811ed32c17577124 [Google Scholar] [PubMed] [CrossRef] [PubMed]
[6]. Jarvis JN, Lawn SD, Vogt M, Bangani N, Wood R, Harrison TS, Screening for cryptococcal antigenemia in patients accessing an antiretroviral treatment program in South AfricaClinical Infectious Diseases 2009 48(7):856-62.10.1086/59726219222372 [Google Scholar] [CrossRef] [PubMed]
[7]. Temstet A, Roux P, Poirot JL, Ronin O, Dromer F, Evaluation of a monoclonal antibody-based latex agglutination test for the diagnosis of cryptococcosis: comparison with two tests using polyclonal antibodiesJ Clin Microbiol 1992 30(10):2544-50.PubMed PMID:1400951 [Google Scholar] [PubMed]
[8]. Lara-Peredo O, Cuevas LE, French N, Barley JW, Smith DH, Cryptococcal infection in an HIV-positive Ugandan populationJ Infect 2000 41(2):195PubMed PMID:1102377410.1053/jinf.2000.069711023774 [Google Scholar] [PubMed] [CrossRef] [PubMed]
[9]. Imwidthaya P, Poungvarin N, Cryptococcosis in AIDSPostgraduate medical journal 2000 76(892):85-88.10.1136/pmj.76.892.8510644384 [Google Scholar] [CrossRef] [PubMed]
[10]. Pongsai P, Atamasirikul K, Sungkanuparph S, The role of serum cryptococcal antigen screening for the early diagnosis of cryptococcosis in HIV-infected patients with different ranges of CD4 cell countsJ Infect 2010 60:474-77.10.1016/j.jinf.2010.03.01520347868 [Google Scholar] [CrossRef] [PubMed]
[11]. Meya D, Manabe YC, Castelnuovo B, Cook BA, Elbireer AM, Kambugu A, Cost-effectiveness of serum cryptococcal antigen screening to prevent deaths among HIV-infected persons with a CD4+ cells count <100 cells/μL who start HIV therapy in resource-limited settingsClin Infect Dis 2010 51:448-55.10.1086/65514320597693 [Google Scholar] [CrossRef] [PubMed]
[12]. Liechty CA, Solberg P, Were W, Ekwaru JP, Ransom RL, Weidle PJ, Asymptomatic serum cryptococcal antigenemia and early mortality during antiretroviral therapy in rural UgandaTrop Med Int Health 2007 12:929-35.10.1111/j.1365-3156.2007.01874.x17697087 [Google Scholar] [CrossRef] [PubMed]
[13]. World Health OrganizationRapid advice: Diagnosis, prevention and management of cryptococcal disease in HIV-infected adults, adolescents and children 2011 GenevaWorld Health Organization [Google Scholar]
[14]. Ganiem AR, Indrati AR, Wisaksana R, Meijerink H, van den Ven A, Alisjahbana B, Asymptomatic cryptococcal antigenemia is associated with mortality among HIV-positive patients in IndonesiaJ Int AIDS Soc 2014 17:1882110.7448/IAS.17.1.1882124476751 [Google Scholar] [CrossRef] [PubMed]
[15]. Murray PR, Baron JH, Pfaller MA, Jorgensen JH, Yolken RH, 2003, Manual of Clinical Microbiology, 8th Ed., American Society for MicrobiologyWashington, D.C.10.1086/383067 [Google Scholar] [CrossRef]
[16]. Park BJ, Wannemuehler KA, Marston BJ, Govender N, Pappas PG, Chiller TM, Estimation of the current global burden of cryptococcal meningitis among persons living with HIV/AIDSAIDS 2009 23:525-30.10.1097/QAD.0b013e328322ffac19182676 [Google Scholar] [CrossRef] [PubMed]
[17]. Corbett EL, Churchyard GJ, Charalambos S, Samb B, Moloi V, Clayton TC, Morbidity and mortality in South African gold miners: impact of untreated disease due to human immunodeficiency virusClinical Infectious Diseases 2002 34(9):1251-58.10.1086/33954011941552 [Google Scholar] [CrossRef] [PubMed]
[18]. Shoham S, Cover C, Donegan N, Fulnecky E, Kumar P, Cryptococcus neoformans meningitis at 2 hospitals in Washington, DC: adherence of health care providers to published practice guidelines for the management of cryptococcal diseaseClinical Infectious Diseases 2005 40(3):477-79.10.1086/42721315668874 [Google Scholar] [CrossRef] [PubMed]
[19]. Manga NM, Cisse-Diallo VM, Dia-Badiane NM, Diop-Nyafouna SA, Yengo DE, Ndour CT, Prevalence and factors associated with positive cryptococcal antigenemia among HIV infected adult hospitalized in senegalJournal of HIV & Retro Virus 2016 /10.21767/2471-9676.100020 [Google Scholar] [CrossRef]
[20]. Oyella J, Meya D, Bajunirwe F, Kamya MR, Prevalence and factors associated with cryptococcal antigenemia among severely immunosuppressed HIV-infected adults in Uganda: a cross-sectional studyJournal of the International AIDS Society 2012 15(1):110.1186/1758-2652-15-1522417404 [Google Scholar] [CrossRef] [PubMed]
[21]. Oladele RO, Akanmu AS, Nwosu AO, Ogunsola FT, Richardson MD, Denning DW, Cryptococcal antigenemia in Nigerian patients with advanced human immunodeficiency virus: influence of antiretroviral therapy adherenceIn Open Forum Infectious Diseases 2016 3(2)Oxford University Press:of w05510.1093/ofid/ofw05527186581 [Google Scholar] [CrossRef] [PubMed]
[22]. Patel S, Shin GY, Wijewardana I, Vitharana SR, Cormack I, Pakianathan M, The prevalence of cryptococcal antigenemia in newly diagnosed HIV patients in a Southwest London cohortJournal of Infection 2013 66(1):75-79.10.1016/j.jinf.2012.09.01423046967 [Google Scholar] [CrossRef] [PubMed]
[23]. Kaplan JE, Vallabhaneni S, Smith RM, Chideya-Chihota S, Chehab J, Park B, Cryptococcal antigen screening and early antifungal treatment to prevent cryptococcal meningitis: a review of the literatureJAIDS Journal of Acquired Immune Deficiency Syndromes 2015 68:S331-39.10.1097/QAI.000000000000048425768872 [Google Scholar] [CrossRef] [PubMed]
[24]. Lindsley MD, Mekha N, Baggett HC, Surinthong Y, Autthateinchai R, Sawatwong P, Evaluation of a newly developed lateral flow immunoassay for the diagnosis of cryptococcosisClinical Infectious Diseases 2011 53(4):321-25.10.1093/cid/cir37921810743 [Google Scholar] [CrossRef] [PubMed]
[25]. Chuck SL, Sande MA, Infections with Cryptococcus neoformans in the acquired immunodeficiency syndromeNew England Journal of Medicine 1989 321(12):794-99.10.1056/NEJM1989092132112052671735 [Google Scholar] [CrossRef] [PubMed]
[26]. Dromer F, Mathoulin-Pélissier S, Launay O, Lortholary O, French Cryptococcosis Study GroupDeterminants of disease presentation and outcome during cryptococcosis: the CryptoA/D studyPLoS Med 2007 4(2):e2110.1371/journal.pmed.004002117284154 [Google Scholar] [CrossRef] [PubMed]
[27]. Sivasangeetha K, Harish BN, Sujatha S, Parija SC, Dutta TK, Cryptococcal meningoencephalitis diagnosed by blood cultureIndian Journal of Medical Microbiology 2007 25(3):28210.4103/0255-0857.34777 [Google Scholar] [CrossRef]
[28]. Naka W, Masuda M, Konohana A, Shinoda T, Nishikawa T, Primary cutaneous cryptococcosis and Cryptococcus neoformans serotype DClinical and Experimental Dermatology 1995 20(3):221-25.10.1111/j.1365-2230.1995.tb01306.x [Google Scholar] [CrossRef]
[29]. Banerjee U, Progress in diagnosis of opportunistic infections in HIV/AIDSIndian J Med Res 2005 121:395-406. [Google Scholar]
[30]. Ogba OM, Abia-Bassey L, Cryptococcal antigenemia among HIV seropositive patients accessing care in antiretroviral therapy (art) clinics in CalabarSouth Southern Nigeria 2015 10.7243/2052-6180-3-7 [Google Scholar] [CrossRef]
[31]. Osazuwa F, Dirisu JO, Okuonghae PE, Ugbebor O, Screening for cryptococcal antigenemia in anti-retroviral naive AIDS patients in benin city, NigeriaOman Med J 2012 27(3):228-31.10.5001/omj.2012.5122811773 [Google Scholar] [CrossRef] [PubMed]
[32]. Magambo KA, Kalluvya SE, Kapoor SW, Seni J, Chofle AA, Fitzgerald DW, Utility of urine and serum lateral flow assays to determine the prevalence and predictors of cryptococcal antigenemia in HIV-positive outpatients beginning antiretroviral therapy in Mwanza, TanzaniaJournal of the International AIDS Society 2014 17(1)10.7448/IAS.17.1.1904025109284 [Google Scholar] [CrossRef] [PubMed]
[33]. Micol R, Tajahmady A, Lortholary O, Balkan S, Quillet C, Dousset JP, Cost-effectiveness of primary prophylaxis of AIDS associated cryptococcosis in CambodiaPloS One 2010 5(11):e1385610.1371/journal.pone.001385621085478 [Google Scholar] [CrossRef] [PubMed]
[34]. Vaidyanathan PS, Singh S, TB-HIV co-infection in IndiaNTI Bulletin 2003 39(3&4):11-18. [Google Scholar]
[35]. Andama AO, den Boon S, Meya D, Cattamanchi A, Worodria W, Davis JL, Prevalence and outcomes of cryptococcal antigenemia in HIV-seropositive patients hospitalized for suspected tuberculosis in UgandaJournal of Acquired Immune Deficiency Syndromes (1999) 2013 63(2):18910.1097/QAI.0b013e3182926f9523542636 [Google Scholar] [CrossRef] [PubMed]
[36]. Baradkar V, Mathur M, De A, Kumar S, Rathi M, Prevalence and clinical presentation of Cryptococcal meningitis among HIV seropositive patientsIndian J Sex Transm Dis AIDS 2009 30(1):19-22.10.4103/0253-7184.5547421938109 [Google Scholar] [CrossRef] [PubMed]
[37]. Kadam D, Chandanwale A, Bharadwaj R, Nevrekar N, Joshi S, Patil S, High prevalence of cryptococcal antigenaemia amongst asymptomatic advanced HIV patients in Pune, IndiaIndian J Med Microbiol 2017 35:105-08.10.4103/ijmm.IJMM_15_59628303828 [Google Scholar] [CrossRef] [PubMed]