Endotracheal intubation is the gold standard of airway management and usage of the cuffed ETT is a common clinical practice. The ETT provides effective ventilation for patients under general anaesthesia and reduces the risk of aspiration by providing a tight seal with the tracheal mucosa.
Almost 40% of the patients after extubation, complains of sore throat and hoarseness of voice in the postoperative period, more so in patients with co-morbidities and smoking [3,7]. The incidence of cough has been noted ranging from 38-96% [8]. Cough during emergency can alter haemodynamics, can lead to haemodynamic instability which can be detrimental in patients with compromised cardiovascular reserve [9].
To prevent all these complications, the cuff of an ETT which is a hydrophobic semi-permeable membrane can be used as a reservoir for drug delivery to the tracheal mucosa [8,10,11]. Various alternatives like saline, plain lignocaine and dexamethasone, have been evaluated for cuff inflation to reduce the laryngotracheal morbidity and decrease the haemodynamic response to extubation [6,12]. To produce this desired effect, the volume of plain lignocaine required will be high, which can increase the cuff pressure [12-14], but alkalinising lignocaine (pH maintained more than 7) will cause faster diffusion, and required volume will be less [14,15]. Use of an alternative method of cuff inflation could be a simple and effective way in decreasing the complications of endotracheal intubation both in the perioperative period as well as in ICU setting. This study was done to compare the effects of ETT cuff inflation with air, saline or alkalinised lignocaine on postoperative airway morbidity.
Materials and Methods
The prospective randomised control study was conducted at Department of Anaesthesiology and Critical care, Justice K.S. Hegde Charitable hospital, Mangalore, Karnataka, India, from March 2018 to September 2018. Institutional Ethics Committee clearance was obtained (INST.EC/EC/079/2017-18).
Adult patients aged between 18-70 years belonging to ASA PS I & II posted for elective surgical procedures, under general anaesthesia with endotracheal intubation lasting more than two hours. Randomisation was done by closed envelope method. According to the Estebe JB et al., the difference of proportion of hoarseness of voice between two groups in that study was 70% [8].
Sample size was calculated using the formula for the difference of proportions as follows:
α: alpha error: 5%
Zα: Z score for the alpha error chosen=1.96 at 5% level of significance
Zβ: Z score: 1.281 at 90% power
p1 (proportion of hoarseness of voice in group 1): 80%
p2 (proportion of hoarseness of voice in group 2): 10%
p=p1+p2
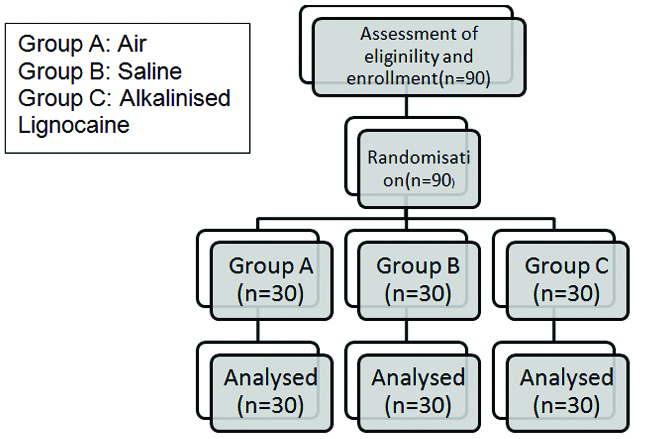
After substituting the concerned values to the above formula we arrived at a sample size (n) ≥15 per group. However, 30 patients were enrolled in each group to increase the power of the study and exclude patients due to protocol violation [Table/Fig-1].
Inclusion Criteria
All adult patients aged between 18-70 years.
Patients belonging ASA PS I & II posted for elective surgical procedures of duration more than two hours under general anaesthesia with endotracheal intubation.
Exclusion Criteria
Refused informed consent by the patient.
Patients undergoing emergency surgeries.
Procedures requiring perioperative nasogastric tube placement.
Patients with a high risk of aspiration.
Anticipated difficult airway.
Pregnant women.
Active upper respiratory tract infections.
Preoperative sore throat.
Previous history of GERD.
Head and neck surgeries and surgeries requiring prone position.
Procedure
All patients underwent a thorough pre-anaesthetic evaluation with a detailed history, complete physical examination and routine investigations and those satisfying the inclusion criteria were enrolled for the study after obtaining an informed and written consent.
Ninety patients were randomly allocated into one of the three groups in which the endotracheal tube cuff was inflated with:
Group A: Air
Group B: Saline
Group C: Alkalinised lignocaine
Alkalinisation of lignocaine was achieved by adding 2.5 mL of 7.5% sodium bicarbonate to 2.5 mL of 2% lignocaine with 5 mL of saline (10 mL). The saline or the alkalinised lignocaine were prepared by OT technician who documented the same in a separate register. The alkalinisation of lignocaine was checked with the use of universal indicator paper. All solution in Group C was ensured to have a pH of above 7. All patients were kept nil per oral and premedicated as per standard guidelines.
On the day of surgery after shifting the patient to OT and intravenous access was secured. Standard monitors such as electrocardiogram (ECG), pulseoximeter, and Non-Invasive Blood Pressure (NIBP) were attached, and baseline vitals were noted. All patients were preoxygenated for 3 minutes and induced with IV Fentanyl 2 mcg/kg and IV Propofol (2 mg/kg) or to the loss of verbal command. After confirmation of adequate bag and mask ventilation Inj. Vecuronium 0.1 mg/kg was given for muscle relaxation. The patients were ventilated using Bain’s circuit and face mask with a mixture of 100% Oxygen and inhaled anaesthetics (isoflurane/sevoflurane). An anaesthesiologist with at least two years of experience did direct laryngoscopy and intubation with Macintosh blade (#3 or #4) following adequate relaxation as judged by a peripheral nerve stimulator.
Endotracheal intubation was done using the appropriate size polyvinylchloride endotracheal tube as per gender and lubricated with saline, and the cuff was inflated with allocated agents as per randomisation. The cuff is inflated till the air leak has just stopped which is assessed by auscultation or presence of any leak in the ventilator expired volume. The cuff pressure was measured only in Group A with air soon after endotracheal cuff inflation and at an interval of 1 hour, 2 hour and before deflation of the cuff.
Patients with unanticipated difficult intubation requiring >2 attempts were excluded from the study. Anaesthesia was maintained with 66% nitrous oxide in oxygen and inhaled anaesthetics with positive pressure ventilation, along with top up of muscle relaxant to maintain ETCO2 between 30-35 mmHg. At the end of the procedure, inhaled anaesthetics were discontinued and patients were extubated after giving appropriate dosage of neuromuscular reversal agent as per institutional protocol. Patients were shifted to Post Anaesthesia Care Unit (PACU) after the completion of the procedure.
An independent observer, who was blinded to the group allocation made the following observations:
Haemodynamic responses to extubation: Heart rate, systolic, diastolic and mean blood pressure was measured just after giving reversal, and immediately after extubation (T0) and subsequently at 5 minute (T5), 10 minute (T10), 15 minute (T15), 30 minute (T30) and at 60 minute (T60).
The smoothness of extubation: Absence of coughing or bucking, and variation of less than 30% from the baseline regarding heart rate, systolic, diastolic and mean blood pressure was considered as smooth extubation. We recorded number of times each patient bucked or coughed after reversal agent was given till extubation. Bucking during oral suctioning was excluded.
The presence of sore throat, hoarseness of voice and cough was documented and graded at intervals of two, four and six hours in PACU after shifting the patient.
A 4 point graded scale was used for sore throat, hoarseness of voice and cough [16]:
1) Sore throat
Grade 0: No sore throat
Grade 1: Mild discomfort or itchy sensation
Grade 2: Pain on swallowing
Grade 3: Pain at rest
2) Hoarseness of voice
Grade 0: No Hoarseness
Grade 1: Hoarseness at the time of interview but noted only by the patient
Grade 2: Hoarseness that is readily apparent but mild
Grade 3: Hoarseness that is readily apparent and severe
3) Cough
Grade 0: No cough
Grade 1: Minimal cough
Grade 2: Moderate cough
Grade 3: Severe cough
Statistical Analysis
SPSS version 20 for Windows was used for analysing data. Continuous data were analysed using one-way ANOVA for normally distributed data and Kruskal- Wallis test for skewed data. Intergroup comparisons were made by using Post-Hoc Bonferroni test for normally distributed data and Mann-Whitney U test for skewed data. Normally distributed data were represented as mean±standard deviation and skewed data was represented as median with an interquartile range between 25th to 75th percentile. Categorical data like proportions were analysed using the Chi-square test. A p-value <0.05 was considered statistically significant.
Results
The demographic variables, duration of surgery and the volume of agent instilled in the ETT cuff were comparable among the groups as stated in [Table/Fig-2].
Comparison of demographic details, duration of surgery and amount of allocated agent instilled in cuff.
| Group A | Group B | Group C | p-value |
|---|
| Age in years (mean±SD) | 41.10±13.61 | 38.67±13.43 | 38.20±13.47 | 0.659* |
| Sex (F/M) | 16/14 | 15/15 | 16/14 | 0.956# |
| Weight in Kg (mean±SD) | 60.47±8.94 | 63.43±8.60 | 62.53±7.90 | 0.386* |
| Duration of surgery in minutes (mean±SD) | 222.07±51.073 | 235.33±50.68 | 219±34.26 | 0.375 |
| Amount of allocated agent in ml (mean±SD) | 5.70±0.72 | 5.85±0.64 | 5.58±0.54 | 0.278 |
*One way Anova; #Chi-square
The cuff pressure was significantly high when baseline values were compared with 1 hour, 2 hour and deflation with a p-value of <0.001. Comparison of cuff pressure from 1st hour till deflation was comparable [Table/Fig-3].
Comparison of cuff pressures at regular intervals.
| Cuff pressure | Mean difference | Standard error | p-value* |
|---|
| Starting v/s 1h | -11.73 | 2.318 | <0.001 |
| Starting v/s 2h | -8.30 | 1.40 | <0.001 |
| Starting v/s Deflation | -5.90 | 1.03 | <0.001 |
| 1h v/s 2h | 3.43 | 1.92 | 0.510 |
| 1h v/s Deflation | 5.83 | 2.149 | 0.066 |
| 2h v/s Deflation | 2.40 | 1.08 | 0.210 |
*Post-Hoc Bonferroni
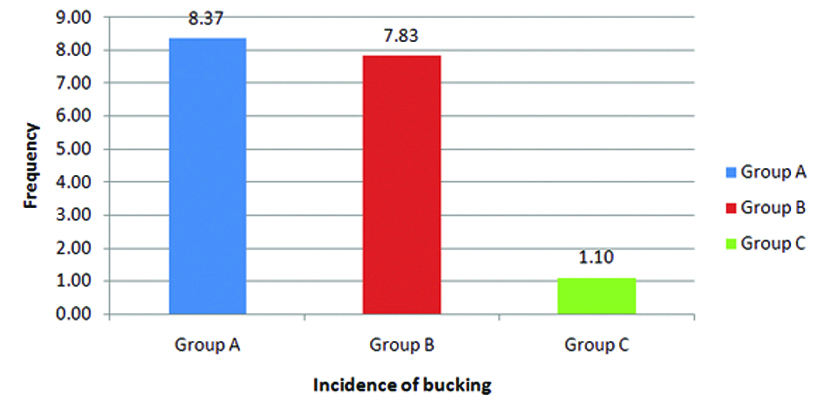
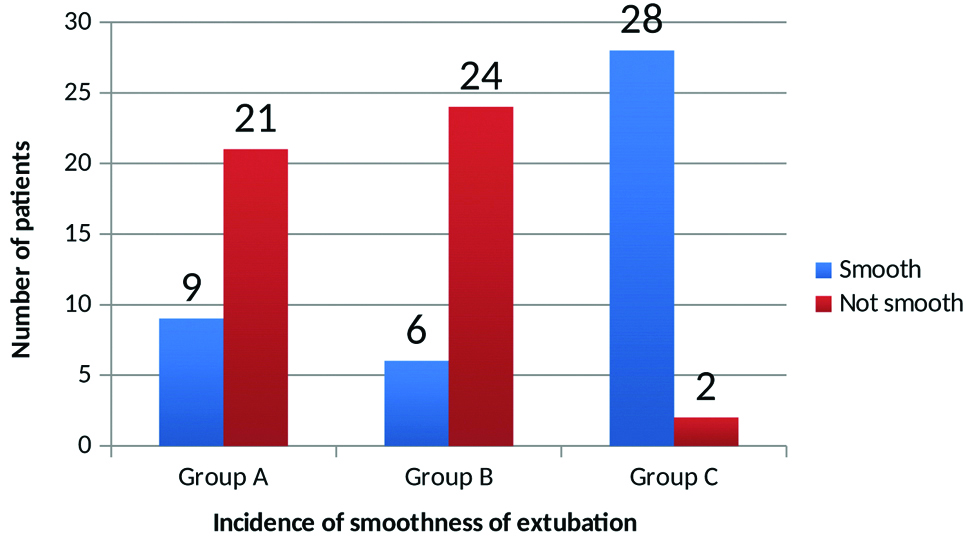
Bucking was assessed after giving of reversal agent: Group C showed a lower incidence of bucking compared to Group A and B which was clinically significant (p<0.001) [Table/Fig-4].
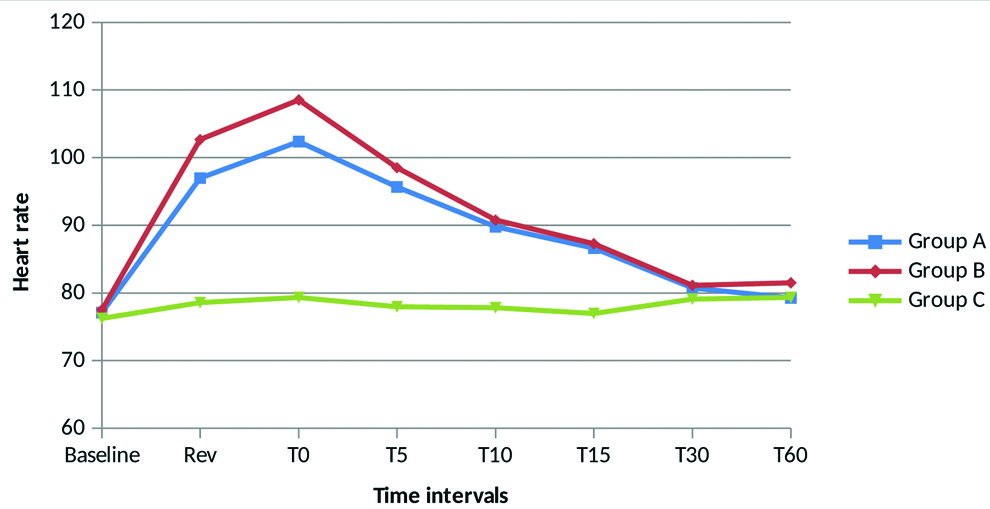
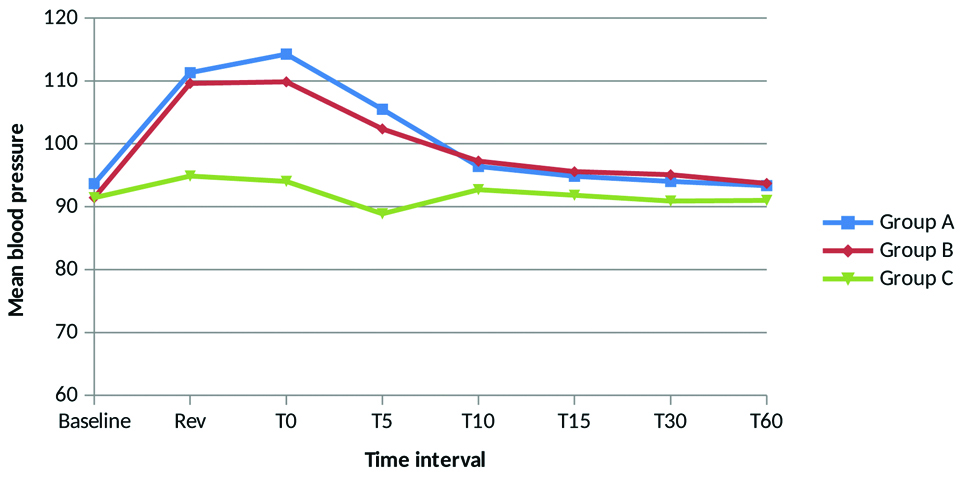
Haemodynamic parameters (heart rate and mean arterial pressure) were measured at baseline before induction, at reversal and after extubation at 0, 5, 10, 15, 30 and 60 minutes after giving reversal. Group C had lower incidence of increase in heart rate compared to Group A and Group B which was statistically significant. From 30 minutes all 3 groups are comparable showing no difference [Table/Fig-5].
Group C had lower incidence of increase in mean arterial pressure compared to Group A and Group B which was statistically significant. From 10 minutes all 3 groups are comparable showing no difference . Group A and Group B was comparable at all intervals [Table/Fig-6].
Trend of mean arterial pressure.
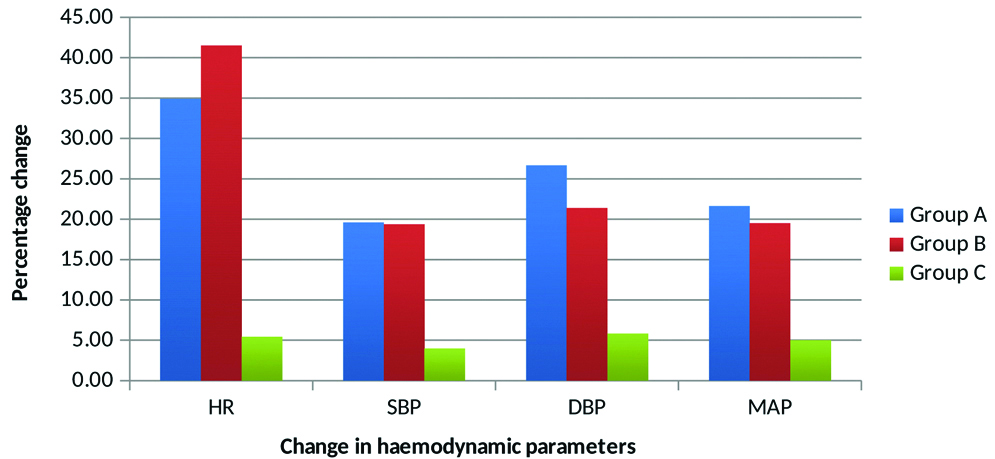
There was a highly significant difference in percentage change in heart rate and blood pressure during extubation among the three groups with a p-value of <0.001 [Table/Fig-7].
Haemodynamic changes during extubation.
Smoothness of extubation: Group C had maximum smooth extubation compared to other two groups (p<0.001) [Table/Fig-8].
Incidence of smooth extubation.
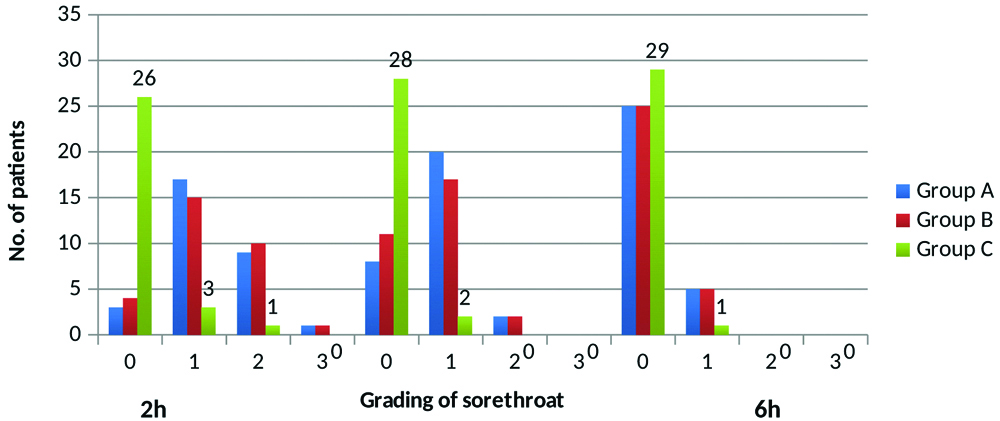
Sore throat: Sore throat grade was lowest in group C at the end of 2 hours and 4 hours. 26 out of 30 had a grade of 0 at the end of 2 hours and 28 out of 30 had a grade of 0 at the end of 4 hours with a p-value of <0.001. At 6 hours all three groups were comparable with a p value of 0.194 [Table/Fig-9].
Incidence of sore throat.
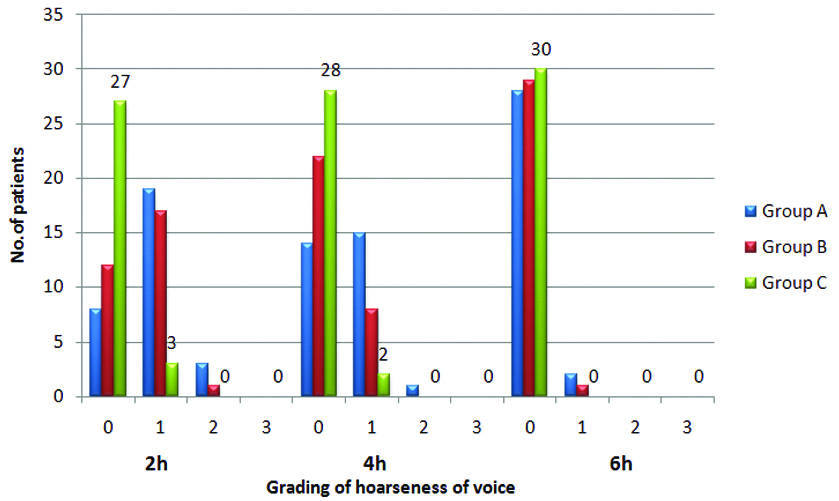
Hoarseness of voice: Hoarseness of voice at 2 hours and 4 hours was lowest in group C. 27 out of 30 patients in group C had a hoarseness grade of 0 at 2 hours and 28 out of 30 had a grade of 0 at 4 hours with a p-value of <0.001. At 6 hours hoarseness of voice was comparable [Table/Fig-10].
Incidence of hoarseness of voice.
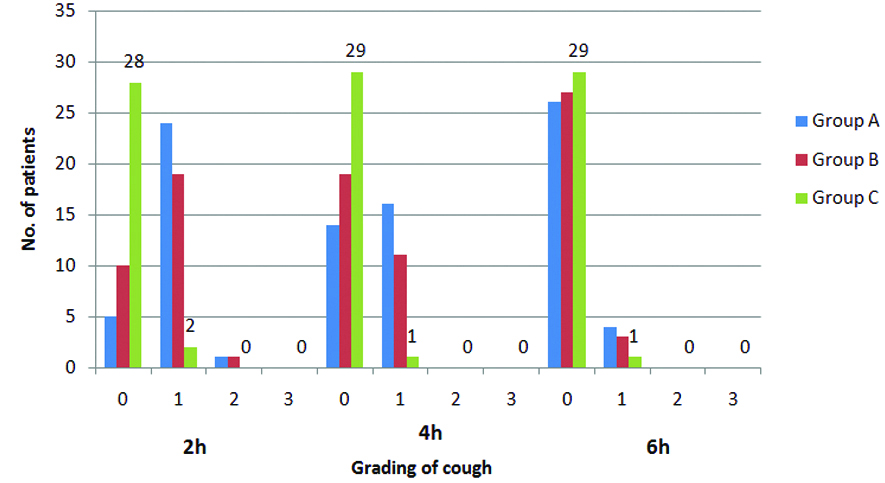
Cough: Cough was lowest in group C at the end of 2 hours and 4 hours. 28 out of 30 had a grade 0 after 2 hours and 29 out of 30 had a grade of 0 at the end of 4 hours with a p-value of <0.001. At 6 hours all three groups were comparable with a p-value of 0.387 [Table/Fig-11].
Discussion
Most of the surgical cases under general anaesthesia are managed with endotracheal intubation with Intermittent Positive Pressure Ventilation (IPPV). Post-intubation, the endotracheal cuff is generally inflated with air which prevents aspiration of gastric contents. Postoperative sore throat, hoarseness of voice and cough are the side effects of intubation. These problems contribute to patient discomfort and laryngotracheal morbidity and delays discharge. The haemodynamic response seen during extubation can lead to significant morbidity and can be catastrophic in cardiopulmonary compromised patients. Smooth extubation with a comfortable post-operative recovery is the desired goal.
In our study, we compared the effect of three agents for inflation of the cuff on the immediate postoperative laryngotracheal symptoms as well as haemodynamic parameters at extubation. All three groups were comparable with regards to age, sex, height and weight as well as the duration of surgery. Minimum period of two hours was taken for the surgery which allowed sufficient time for the drug to diffuse out of the cuff. The incidence of Postoperative Sore Throat (POST) was compared among the three groups. It was noted to have 7 to 8 times lesser incidence of POST in alkalinised 0.45% lignocaine group (13.3%) when compared to saline (86.7%) and air (90%) groups. Alkalinised lignocaine group has a minimal incidence of sorethroat with a p-value of <0.001 at the end of two and four hours when compared to saline and air. These findings are similar to the study of Soares SM et al., were the incidence of sore throat was 11 times higher in air (22%) group and 5 times higher in saline (10%) group when compared to alkalinised lignocaine (2%) group, and the decrease was maximum with 1% lignocaine [17]. Similarly, Jaichandran W et al., found that the POST incidence after 1 hour of extubation decreased by 5 times when 2% alkalinised lignocaine was used instead of air for cuff inflation [18].
In our study, the incidence of Postoperative Hoarseness of Voice (POHV) was 6 to 7 times lesser in alkalinised 0.45% lignocaine group (10%) when compared to air (73.3%) and saline (60%) and it was mostly seen after two and four hours. Similarly, Estebe JB et al., also noted 19 times lesser incidence of POHV in alkalinised lignocaine (4%) when compared to air (76%) and 8 times when compared to plain lignocaine (32%) [19]. Jolly S et al., also showed that hoarseness of voice at post-extubation (24hrs) was minimal in alkalinised lignocaine group (6%) when compared to saline (19%) and plain lignocaine (11%) with a p-value of 0.04 [9]. We found that the incidence of Postoperative Cough (POC) was less in alkalinised 0.45% lignocaine group (6.7%) compared to air (83.3%) and saline (66.7%) group. Alkalinised lignocaine group had 11-12 times lesser incidence of cough postoperatively with a p-value of <0.001 at the end of two and four hours when compared to saline and air. Fagan C et al., also compared the incidence of cough post-extubation, when ETT cuff was inflated with lignocaine, air and saline [12]. They found that the minimum incidence of cough was seen in the lignocaine group which was 16% when compared to air and saline which was 38% and 44% respectively.
In our study, we measured the cuff pressure in air group and noticed that there was an increase of cuff pressure from baseline when compared at intervals of one hour, two hours and before deflation with a p-value of <0.001. We used N2O for maintenance of anaesthesia. Baseline haemodynamic parameters were noted before induction and were comparable among all three groups with a p-value of 0.448. Haemodynamic response during and post-extubation was compared in all the three groups. Alkalinised lignocaine group showed a better result compared to the other groups, which was transient and lasted for 15 minutes for heart rate and 5 minutes for blood pressure. The incidence of bucking was lowest in group C. The smoothness of extubation was better in alkalinised lignocaine, showed 93.3% incidence of smooth extubation when compared to air and saline which had only 30% and 20% respectively (p<0.001).
It is well known that the irritant receptors present in tracheal mucosa are very sensitive to physical or chemical stimulation. ETT cuff is made of polyvinylchloride, which forms a semi-permeable membrane through which lipophilic substance can diffuse across. Therefore, the lignocaine thus reaching the tracheal mucosa has perhaps anaesthetised the mucous membrane obtunding the extubation response and decreasing the immediate postoperative morbidity.
Limitation
The drawbacks of the study were gauged as the incompatibility of the cuff manometer, which lead to measuring of the cuff pressure of ETT only for Group A (air), and not done for Group B (saline) and Group C (alkalinised lignocaine), the vocal cord mobility of the patient was not checked during extubation and blood serum levels of lignocaine was not checked intraoperatively.
Strength of the study: Sample size was adequate for the study, it was properly randomised and proper blinding was followed. The results are unambiguously in favour of alkalinised lignocaine with statistical proof of the same. The outcomes are similar to previous reports reinforcing the hypothesis.
Conclusion
Use of intracuff alkalinised lignocaine is very effective in reducing the laryngotracheal morbidity like sore throat, hoarseness of voice and cough in the immediate postoperative period when compared to saline and air. It also helps in smoother extubation by decreasing haemodynamic response and bucking over the tube. It is a safe and effective method of improving extubation and recovery from endotracheal intubation for patients undergoing surgeries under general anaesthesia.
*One way Anova; #Chi-square
*Post-Hoc Bonferroni