Squamous Cell Carcinoma Involving Periocular Area
Madhumita Rout1, Zahiruddin Khan2, Lipika Panda3
1 Postgraduate Resident, Department of Ophthalmology, Hitech Medical College, Bhubaneswar, Odisha, India.
2 Professor, Department of Ophthalmology, Hitech Medical College, Bhubaneswar, Odisha, India.
3 Assistant Professor, Department of Ophthalmology, Hitech Medical College, Bhubaneswar, Odisha, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Madhumita Rout, Heritage Properties 1 Jagannath Nagar, Road No-15, Ggp Colony, Bhubaneswar-751010, Odisha, India.
E-mail: drmadhuophtha@gmail.com
Squamous Cell Carcinoma (SCC) involving periocular area accounts for 5-10% of all malignant eyelid neoplasms. Although, periocular SCC is the second most common eyelid malignancy after basal cell carcinoma, but is more aggressive and invasive than basal cell carcinoma. It can metastasize and invade the orbital and intracranial structure, hence it has a considerable potential of mortality and morbidity. We report a case of 35-year-old male with SCC involving periocular area who presented with non-healing ulcer over the skin of upper eyelid, lower eyelid and outer canthus of left eye with Perineural Invasion (PNI) and Lymphovascular Invasion (LVI).
Lymphovascular invasion, Perineural invasion, Periocular squamous cell carcinoma
Case Report
A 35-year-old male patient reported to the Department of Ophthalmology with chief complaint of redness, lacrimation and ulcerated growth over the eyelid of left eye since last six months. He is a security guard by profession. He was a known case of xeroderma pigmentosum, diagnosed when he was 20-year-old. He first noticed small keratinized growth over forehead 15 years back, which was non-progressive in nature and was not associated with pain or fever. He was not on any medication for the same.
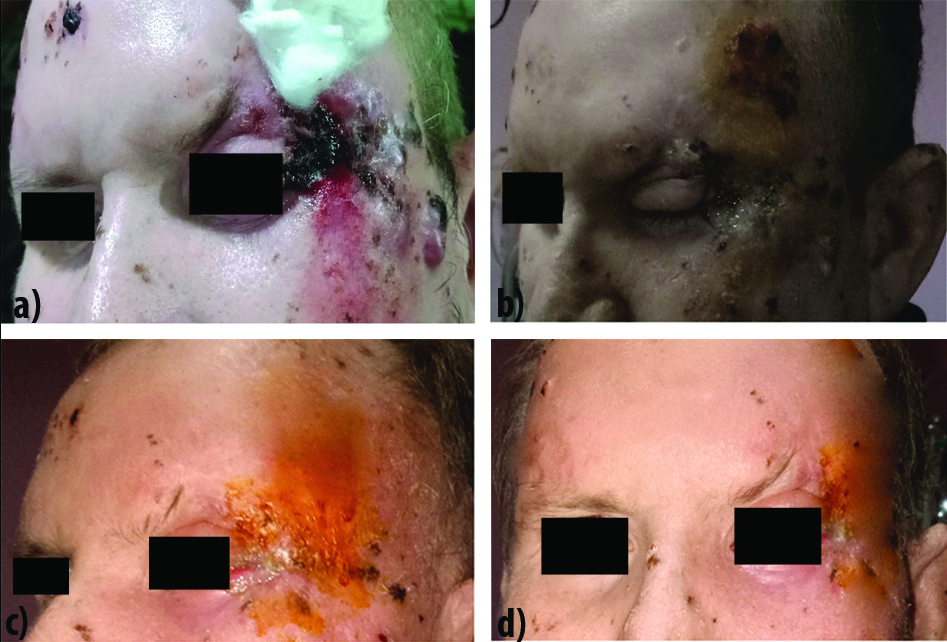
On examination there was a 15×7 mm nodular growth located at lateral canthus of left eye. It extended superio-inferiorly and mesiodistally [Table/Fig-1a]. Around 2-3 similar keratinized nodular growths were also located over the forehead. On inspection, it had necrotic background, ulcerative, non-exudative, irregular borders and on palpation it was firm in consistency, bleeds easily on touch. On ocular examination, eyes were orthotropic, ocular motility full and free in all directions. Intraocular pressure was normal in both the eyes. Slit lamp examination showed edematous, hyperpigmented lesion in the skin of upper eyelid, lower eyelid and outer canthus of left eye. Conjunctiva, Cornea, Iris were within normal limits in both eyes. Pupil was round, regular, reacting to light in both eyes. Visual acuity was normal in both eyes. Fundus examination showed normal retina in both eyes [Table/Fig-2]. On palpation of regional lymph node -ipsilateral neck lymph nodes were enlarged and non-tender.
(a) Squamous cell carcinoma before surgery; (b) SCC after total surgical excision; (c) SCC after Phase I Radiotherapy; (d) SCC after Phase II Radiotherapy.
| Ocular position/Orbit | Normal |
| Ocular alignment | Orthotropic |
| Right eye | Left eye |
| Ocular motility | Full in all directions | Full in all directions |
| Visual acuity | 6/6 N6 | 6/6 N6 |
| Applanation tonometry | 14 mmHg | Digitally normal |
| Slit lamp examination | Eyelids | Flat | Edematous lesion in the skin near upper eyelid and lateral canthus |
| Conjunctiva | Normal | Mild congestion on temporal side |
| Sclera | Normal | Normal |
| Cornea | Clear | Clear |
| Anterior chamber | Normal in contents and depth | Normal in contents and depth |
| Iris | Iris Transilluminance+ | Iris Transilluminance+ |
| Pupil | Round, Regular, Reacting | Round, Regular, Reacting |
| Fundus examination | Retina | Normal | Normal |
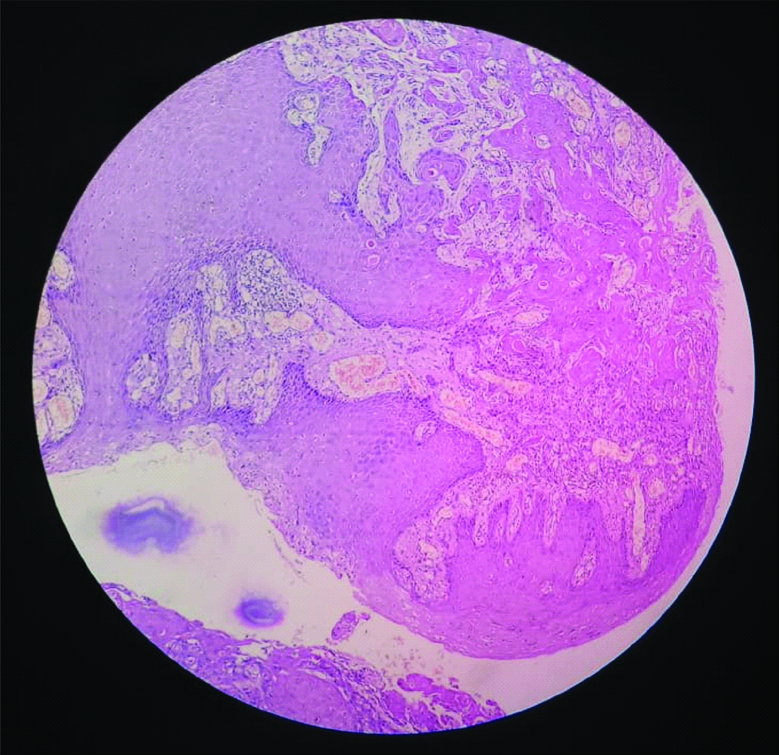
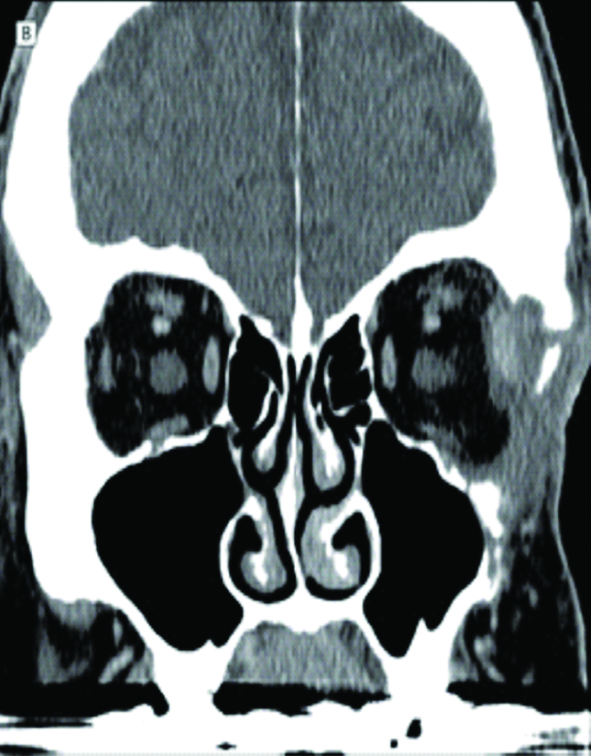
FNAC of forehead lesion showed cellular, clusters of polygonal cells with high N:C ratio. Histopathological examination of excisional biopsy showed well differentiated SCC infiltrating the underlying skeletal muscle bundle with presence of LVI and PNI [Table/Fig-3]. CT scan of orbit shows heterogenous enhancing mass lesions with internal area of necrosis in supero-lateral aspect of left orbit with extension to surrounding areas. Erosion of lateral wall of orbit was noted [Table/Fig-4]. Other routine examinations were within normal limits. According to American Joint Committee on Cancer Staging System, he was staged as SCC Stage III (T3aN1M0).
Histopathological examination of excisional biopsy showing well differentiated squamous cell carcinoma (4x). Tumour is infiltrating the underlying skeletal muscle bundle with presence of Lymphovascular Invasion (LVI) and Perineural Invasion (PNI).
CT scan shows heterogenous enhancing mass lesions with internal area of necrosis in superolateral aspect of left orbit with extension to surrounding areas. Erosion of lateral wall of orbit noted.
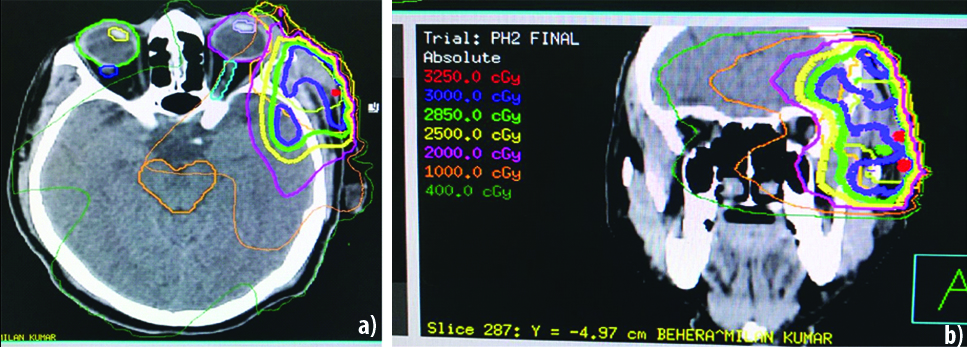
He underwent total surgical excision of lesion with direct closure. Frozen section examination of surgical margins was used to ensure adequate excision. As histopathological examination showed underlying skeletal muscle bundle infiltration with presence of LVI and PNI, he was given external beam radiotherapy to lateral orbital wall given in two phases. In phase I, total dose of 30 gray in 15 fractions in 26 days (30 gy/15#/26 days) and in phase II, a total dose of 24 gy/12#/16 days was given [Table/Fig-1b-d,5]. He was followed-up regularly, no recurrence has occurred at six months postoperatively.
CT mapping for phase I and phase II radiotherapy.
Discussion
SCC involving periocular area accounts for 5-10% [1,2] of all malignant eyelid neoplasms. Periocular SCC is the second most common eyelid malignancy and the incidence has been reported to be between 0.09 and 2.42 cases per 100 000 population [3]. Periocular SCC is a potentially fatal disease because of its ability to invade the orbital and intracranial regions and metastasize to the lymph nodes and distant organs, hence it has a considerable potential of mortality and morbidity [4]. An overall rate of regional lymph node metastases reported to range from 10% to as high as 20%-25% [5]. However, early detection and with proper treatment, the prognosis is outstanding and death and disability can be reduced. The clinical presentation varies and histological assessment is necessary for correct diagnosis. Two studies by Veness MJ et al., and Jambusaria-Pahlajani A et al., in high-risk patient groups identified that PNI and/or LVI (composite feature) as an independent risk factor for nodal metastasis and disease-specific death [6,7]. In our case, PNI, an adverse prognostic sign, was there and by its PNI capacity; there is high chance that it may invade orbital structures. So post-operative prophylactic radiotherapy was considered. Treatment protocol in our patient i.e., complete surgical excision with histologically confirmed clear margin is same as in a retrospective study done by Donaldson MJ et al., [2]. In our case orbital invasion has started as evidenced by infiltration of tumour cells to the underlying skeletal muscle bundle, necrosis in supero-lateral aspect of left orbit with extension to surrounding areas and erosion of lateral wall of orbit. It is a rare, but serious complication especially in aggressive or neglected lesions. The incidence of orbital invasion has been reported to occur in 2.5% of all eyelid basal and SCC [8]. Presence of PNI, previous recurrences, longer duration of lesion and larger lesion size are adverse prognostic factors associated with secondary orbital invasion [9].
Conclusion
SCC involving periocular area is relatively uncommon, but potentially a fatal disease. Prognosis is excellent and death and disability can be reduced, if detected early and treated adequately. Histological examination is required for accurate diagnosis. Presence of PNI and LVI should be considered high risk features. Regular follow-up examination are advised in all patients with eyelid SCC to prevent recurrence or deadly complication.
[1]. Malhatra R, Huilgol SC, Huynh NT, Selva D, The Australian Mohs databasePeriocular squamous cell carcinoma. Ophthalmology 2004 111:617-23.10.1016/j.ophtha.2003.07.02015051191 [Google Scholar] [CrossRef] [PubMed]
[2]. Donaldson MJ, Sullivan TJ, Whitehead KJ, Williamson RM, Squamous cell carcinoma of the eyelidsBritish Journal of Ophthalmology 2002 86(10):1161-65.10.1136/bjo.86.10.116112234899 [Google Scholar] [CrossRef] [PubMed]
[3]. Cook BE, Bartley GB, Epidemiologic characteristics and clinical course of patients with malignant eyelid tumours in an incidence cohort in Olmsted County, MinnesotaOphthalmology 1999 106:746-50.10.1016/S0161-6420(99)90161-6 [Google Scholar] [CrossRef]
[4]. Reifler DM, Hornblass A, Squamous cell carcinoma of the eyelidSurv Ophthalmol 1986 30:349-65./10.1016/0039-6257(86)90089-5 [Google Scholar] [CrossRef]
[5]. Thosani MK, Schneck G, Jones EC, Periocular squamous cell carcinomaDermatologic Surgery 2008 34(5):585-99.10.1097/00042728-200805000-0000118248482 [Google Scholar] [CrossRef] [PubMed]
[6]. Veness MJ, Palme CE, Morgan GJ, High-risk cutaneous squamous cell carcinoma of the head and neck: results from 266 treated patients with metastatic lymph node diseaseCancer 2006 106(11):2389-96.10.1002/cncr.2189816649220 [Google Scholar] [CrossRef] [PubMed]
[7]. Jambusaria-Pahlajani A, Kanetsky PA, Karia PS, Hwang WT, Gelfand JM, Whalen FM, Evaluation of AJCC tumour staging for cutaneous squamous cell carcinoma and a proposed alternative tumour staging systemJAMA Dermatol 2013 :1-9.10.1001/jamadermatol.2013.245623325457 [Google Scholar] [CrossRef] [PubMed]
[8]. Howard GR, Nerad JA, Carter KD, Whitaker DC, Clinical characteristics associated with orbital invasion of cutaneous basal cell and squamous cell tumours of the eyelidAm J Ophthalmol 1992 113:123-33.10.1016/S0002-9394(14)71523-5 [Google Scholar] [CrossRef]
[9]. Soysal HG, Markoç F, Invasive squamous cell carcinoma of the eyelids and periorbital regionBr J Ophthalmol 2007 91(3):325-29.10.1136/bjo.2006.10267317020898 [Google Scholar] [CrossRef] [PubMed]