Laparoscopic cholecystectomy is one of the most commonly performed elective surgeries worldwide. The exponential increase is probably due to a combination of increased availability of ultra-sonographic diagnosis and patient awareness. With the gain of expertise and evolution of technology this procedure became one of the most commonly performed surgeries for many surgeons.
A key step in the performance of this surgery is the dissection of Calot’s triangle to isolate cystic artery and cystic duct in order to divide these key structures safely. The division of cystic artery with power sources like bipolar coagulation and Harmonic Scalpel (HS) has been described [1]. But almost all surgeons prefer to mechanically occlude cystic duct with metallic clip, suture ligation or staplers prior to division: there is a visceral suspicion and dislike among surgeons for bile leak.
This almost obsessive need for mechanical occlusion has its own downsides: time, cost and potential delayed complications. Even if the issues of increased duration of surgery and cost are overlooked, the rare potential delayed complication of clip migration into common bile duct leading to biliary obstruction has to be borne in mind [2-5].
With the increased incidence of the procedure, even rare complications like clip migration are becoming more frequent. Consequently, this very commonly performed surgery has started to lure in litigations against surgeons [6].
Thus, it is only reasonable to explore alternatives of clip for cystic duct closure. One of the simplest alternatives was use of HS. But prior to trials on patients, it was thought prudent to study the excised gallbladders ex-vivo. Very few studies have been done to assess burst pressures of gallbladder ex-vivo with the aim of comparing HS and standard clipping. A very similar study by Kavlakoglu B et al., was done in Ankara, Turkey which is at sea level [7]. The result of that study indicated that burst pressure is similar in both the clip and the HS group. No such study was done at higher alitudes with a much lower ambient atmospheric pressure. Change in ambient pressure is liable to affect the burst pressures.
This study was undertaken to address the issue of feasibility of closure and division of cystic duct using HS only by comparing the ex-vivo burst pressures of gallbladders (removed during laparoscopic cholecystectomy) whose cystic ducts were occluded by either metallic clip or HS.
Materials and Methods
The study was conducted in Sikkim Manipal Institute of Medical Sciences, Gangtok, Sikkim, India, as a prospective analytical study from 2017 to 2018. The study was planned as a prospective ex-vivo randomised comparative interventional study involving ascertaining the ‘burst pressure’ of intact gallbladder removed during planned laparoscopic cholecystectomy. The study group was randomised into two groups using computer generated random number tables, the first in which the cystic duct was occluded with standard metallic surgical clip and the other in which it was divided with HS.
This study also got the approval first in institutional Research Protocol Evaluation Committee (RPEC) followed by Institutional Ethics Committee (IEC). RPEC Reference Number: SMIMS/RPEC/2016-062 RPEC Registration Number: RPEC/324/16-062. IEC Reference Number: SMIMS/IEC/C/2016-066. IEC Registration Number: IEC/458/16-066.
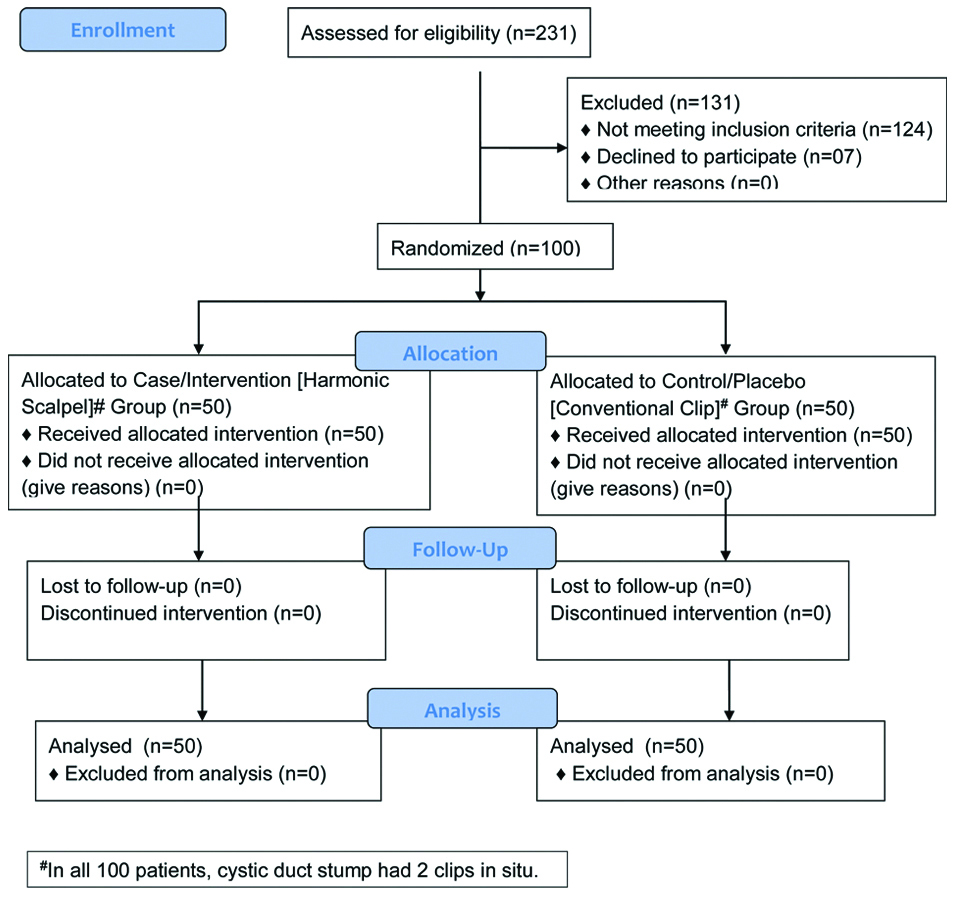
A sample size of 100 (50 in each group) was calculated [8], based on a similar study by Kavlakoglu B et al., who mentioned burst pressures of 332.46±24.0 mmHg and 343.06±29.3 mmHg for the two groups [for an α error of 0.05 and a β error of 0.20]. [Table/Fig-1] [7].
CONSORT 2010 flow diagram.
Patients scheduled for elective cholecystectomy during the study period and giving consent to participate were included in the study. The exclusion criteria were:
Patients with Common Bile Duct (CBD) stones (choledocholithiasis).
Suspicion of gallbladder malignancy based on ultrasonography and/or subsequent Computed Tomography (CT) findings.
Patients with complicated cholelithiasis, mucocele, empyema, gangrene or perforation of gallbladder.
Dense adhesions of gallbladder leading to extensive adhesiolysis and excessive handling of gallbladder.
Equipment or other technical failure leading to ergonomic difficulties.
Any injury or puncture of the gallbladder intraoperatively or during extraction.
Cystic duct length less than 5 mm determined intraoperatively.
Cystic duct diameter more than 7 mm determined intraoperatively.
During the course of preoperative evaluation for elective laparoscopic cholecystectomy, specific note was made of the wall thickness of gallbladder evaluated by sonography, in addition to other pertinent information regarding the biliary system.
Standard three or four port laparoscopic cholecystectomy was performed under general anaesthesia, taking specific cognizance to avoid undue aggressive handling or injury of the gallbladder. Once the gallbladder was extirpated from its liver bed it was placed in a retrieval bag, which was extracted intact through the umbilical port.
Ex-vivo, the cystic duct was re-clipped and divided with scissor just distal to the new clip in the clip group. In the harmonic group the cystic duct was divided ex-vivo using Ethicon® HS (at min mode at intensity 2). Then the gallbladder was immersed in normal saline at body temperature and connected to the intra-arterial pressure transducer module (of the anaesthesia workstation) with 20-gauge cannula inserted from the intact body of the gallbladder. The gallbladder was slowly instilled with normal saline (1 mL/sec) and real time intraluminal pressure was recorded using the invasive blood pressure module, until the gallbladder burst. The peak pressure at which the burst occurred was noted from the IBP module trace. Site of burst was also noted.
Statistical Analysis
Data was tabulated and analysed using Microsoft© Excel© 2016 and IBM© SPSS©-23. Comparison of burst pressure between the two groups (clip vs. HS) was done using appropriate statistical tools. The p-value of <0.05 was deemed to be significant.
Results
The overall mean age was 38.45±12.77, while it was similar in the clip and HS group at 37.96±12.92 and 39.04±12.72, the difference being statistically nonsignificant (p-value=0.675) [Table/Fig-2]. Similarly, the difference in mean gallbladder wall thickness was not statistically significant (p-value=0.959), being 3.058±0.735 mm and 3.064±0.634 mm in clip and HS group respectively (overall 3.060±0.577 mm). The overall mean BMI was 24.12±2.46. The BMI in clip and HS groups were, 24.69±2.05 and 23.55±2.7. This minor difference was statistically significant (p-value=0.019). The distribution frequencies are shown in [Table/Fig-3]. The distribution of these frequencies for age, sex, BMI and sonographic gallbladder wall thickness between the two groups was statistically nonsignificant on performing chi-squared test (p-value >0.05).
Age and sex distribution.
| Age group (years) | Clip | HS |
|---|
| Female | Male | Female | Male |
|---|
| 11-20 | 1 | 1 | 2 | 0 |
| 21-30 | 3 | 1 | 8 | 1 |
| 31-40 | 14 | 2 | 20 | 1 |
| 41-50 | 7 | 2 | 8 | 0 |
| 51-60 | 3 | 2 | 4 | 2 |
| 61-70 | 3 | 1 | 2 | 1 |
| 71-80 | 0 | 0 | 1 | 0 |
| Overall count | 41 | 9 | 45 | 5 |
| Mean age | 37.07 | 42.00 | 38.13 | 47.20 |
| SD | 12.67 | 14.07 | 12.21 | 15.79 |
BMI and sonographic GB wall thickness.
| Overall | Clip | HS |
|---|
| BMI (kg/m2) | Underweight (<19) | Counts | 2 | 0 | 2 |
| Normal (19-25) | 60 | 29 | 31 |
| Overweight (25-30) | 36 | 20 | 16 |
| Obese (>30) | 2 | 1 | 1 |
| Mean BMI | 24.12 | 24.69 | 23.55 |
| SD | 2.46 | 2.05 | 2.71 |
| Gallbladder wall thickness (mm) | ≤3 mm | Counts | 85 | 45 | 40 |
| 3-6 mm | 14 | 4 | 10 |
| >6 mm | 1 | 1 | 0 |
| Mean thickness | 3.060 | 3.058 | 3.064 |
| SD | 0.577 | 0.735 | 0.634 |
The mean intraoperatively visually determined external cystic duct diameter was 5.57±0.69 mm in the clip group and 5.672±0.59 mm in the HS group (overall 5.62±0.64 mm), the minor difference being statistically nonsignificant (p-value=0.431).
The overall mean burst pressure of extracted gall-bladders was 164.12 mmHg, being 162.26±19.25 mmHg and 165.98±21.34 mmHg in the clip and harmonic scalpel group respectively, the difference being statistically nonsignificant (p-value=0.362). The lowest pressure at which the burst occurred was 102 mmHg, occurring at the body of a gallbladder with cystic duct diameter of 6 mm. None of the gallbladders burst at the needle puncture site used for saline inflation.
On further analysis we found that there was no statistically significant difference between the mean burst pressures of the two groups within any of the subgroups, as detailed in [Table/Fig-4]. Eighty-one of the gall-bladders burst at the fundus on saline inflation, having an almost similar mean burst pressure of 164.18±19.71 mmHg versus 168.37±19.52 mmHg (p-value=0.339).
Comparison of mean gallbladder burst pressures in different subgroups between clip and HS groups.
| Subgroups | Subgroups |
|---|
| Clip | HS | p-value |
|---|
| Sex | Female | 162.51±18.74 (n=41) | 164.80±21.81 (n=45) | 0.602 |
| Male | 161.11±22.65 (n=9) | 176.60±13.87 (n=5) | 0.139 |
| Age (years) | 11-20 | 168.50±4.95 (n=2) | 180.50±19.09 (n=2) | 0.534 |
| 21-30 | 157.07±14.16 (n=14) | 162.00±19.64 (n=9) | 0.526 |
| 31-40 | 164.56±23.49 (n=16) | 168.86±24.59 (n=21) | 0.593 |
| 41-50 | 157.67±23.04 (n=9) | 158.88±22.64 (n=8) | 0.915 |
| 51-60 | 175.40±15.37 (n=5) | 164.50±18.24 (n=6) | 0.310 |
| 61-70 | 162.00±12.46 (n=4) | 165.67±10.02 (n=3) | 0.685 |
| 71+ | (n=0) | 179.00 (n=1) | - |
| BMI (kg/m2) | Normal | 160.14±17.34 (n=29) | 165.29±22.75 (n=31) | 0.326 |
| Obese | 159.00 (n=1) | 154.00 (n=1) | - |
| Overweight | 165.50±22.23 (n=20) | 171.81±16.26 (n=16) | 0.333 |
| Underweight | (n=0) | 136.00±18.38 (n=2) | 0.000 |
| Gallbladder wall thickness (mm) | ≤3 mm | 163.20±19.87 (n=45) | 167.23±20.54 (n=40) | 0.362 |
| ≤6 mm | 153.00 (n=1) | (n=0) | - |
| 3-6 mm | 154.00±11.49 (n=4) | 161.00±24.86 (n=10) | 0.487 |
| Cystic Duct Diameter (mm) | 2.1-4.0 mm | 176.40±16.82 (n=5) | 186.00±16.97 (n=2) | 0.572 |
| 4.1-6.0 mm | 160.86±19.20 (n=44) | 164.98±21.44 (n=47) | 0.337 |
| >6 mm | 153.00 (n=1) | 173.00 (n=1) | - |
| Bursting Point | Body | 161.33±9.81 (n=6) | 155.14±30.39 (n=7) | 0.626 |
| Fundus | 164.18±19.71 (n=40) | 168.37±19.52 (n=41) | 0.339 |
| Occlusion area | 144.50±19.30 (n=4) | 155.00±15.56 (n=2) | 0.532 |
| Histopathology | Acute cholecystitis | 173.25±26.00 (n=4) | 144.00 (n=1) | 0.389 |
| Chronic cholecystitis | 161.29±18.83 (n=45) | 166.38±21.55 (n=48) | 0.228 |
| Normal / polyp | 162.00 (n=1) | 169.00 (n=1) | - |
| Overall | 162.26±19.25 (n=50) | 165.98±21.34 (n=50) | 0.362 |
Only six of the extracted gall-bladders ruptured at the site of occlusion (by either clip or harmonic scalpel at the cystic duct) on saline inflation. Of these four were in the clip group and two in the HS group. The mean burst pressure in the clip group was 144.50±19.30 mmHg while in the HS group it was higher at 155.00±15.56 mmHg, though this difference was not statistically significant (p-value=0.532).
Discussion
Delayed complications associated with use of mechanical occlusion of cystic duct stump (clips or hem-o-loK® etc.,) for closure of cystic duct stump are being reported frequently. The commonest of these complications is clip migration into common bile duct and acting as a nidus for calculus formation [3,5,9,10]. Thus, it was imperative that to explore alternative means of cystic duct stump closure. HS has been explored previously for this purpose. The consideration of HS for this purpose stems from the fact that it has been safely used for long to seal blood vessels which have much higher and pulsatile luminal pressures [11].
In the current study, the pressures (162.26±19.25 mmHg clip and 165.98±21.34 mmHg for HS groups) at which the excised gallbladder burst on being instilled with normal saline was similar irrespective of whether clip or HS was used for occlusion of the gallbladder. This finding was similar to those reported by Kavlakoglu B et al., [7]. Although the burst pressures reported by them (332.46±24.00 mmHg for clip and 343.06±29.3 mmHg for HS groups) were higher, there was no significant difference between the two groups. The difference can be partially explained by the significantly lower ambient atmospheric pressure at the location of the current study (Gangtok, India) compared to Ankara, Turkey where Kavlakoglu’s study was conducted. Similarly, Westervelt J, Eltiras R et al., and Vijayvagiya A et al., have found HS to be safe for division of cystic duct provided it is not unduly wide (>6 mm), especially in terms of postoperative leakage from divided cystic duct stump [12-14].
Only six gallbladders burst at the occluded point, four in clip group and two in HS group. The higher burst pressure in HS group, compared to the clip group, was statistically nonsignificant (p-value=0.532).
It is worth noting that the mean pressures in the common bile duct is 12 cm H2O (8.8 mmHg) [15] while the maximum pressure exerted by sphincter of Oddi is about 100 mmHg [16]. The pressures at which the cystic dust bursts open is consistently higher than this (lowest burst pressure being 117 and 144 mmHg in clip and HS groups respectively).
Hüscher CGS et al., had described the method for division of cystic duct by HS [1]. He stated that the blades were first applied more proximally for a few seconds and then they were applied a few millimetres distal to the previous application site, holding the grasp until the division of the duct was completed. As the instrument has no feedback sensors this “few seconds” varies from surgeon to surgeon and this might require some standardisation by improved instrumentation or training.
Limitation
The current study compared only HS and metallic clip in ex-vivo gallbladder specimens extracted intact during laparoscopic cholecystectomy.
Conclusion
Harmonic scalpel provides equivalent safety (on comparison of burst pressure) for occlusion of cystic duct compared to metallic clip. Thus, it is concluded that HS can be used for cystic duct occlusion safely without any clip application.
Future recommendation: In vivo studies with comparison of leak rates and other complications between the two groups is required for a robust conclusion and any attempts at providing recommendation. Other modalities like Ligasure® and Thunderbeat® must also be studied for establishing the best modality for cystic duct stump closure.