Balance has been defined as the ability to control body’s Centre Of Gravity (COG) within given base of support [1,2], and has a continuum of postural stability from static to dynamic. It is primarily concerned with preserving, attaining, or restoring the centre of mass in relation to the limits of stability within a given base of support [3,4], and plays an important role in mobility, stability and the performance of many activities of daily living. The populations which are mostly affected are older people, post-injury or post-surgical, and those with neuromuscular dysfunction or pathology including DPN [5-7]. DPN comprises of sensory loss such as vibration perception, pressure and proprioception, affecting balance control, and as many as 30% of people with DPN experience muscle weakness, loss of ankle reflexes leading to decreased balance and coordination [8,9].
It is important to assess the integrity of the balance system to evaluate individual balance capabilities. Static, dynamic and functional balance tests have been developed to more adequately evaluate performance on the type of task. OLS, FRT and TUG are the clinical tests for static and dynamic balance. These clinical tests have demonstrated good reliability, validity and responsiveness in older population and people with balance impairment [10-13].
Recently, computerised measurements and feedback systems that assess static and dynamic balance performance, provide quantitative information and feedback pertaining to stability and weight transferred, have become more readily available. Various computerised devices like Biodex balance system, Wii balance board and force platform used to assess balance measures have been found to be reliable and valid [14-17]. However, these assessment systems are expensive compared to Pedalo®-Sensomove balance system (SensbalanceMiniBoard, Utrecht, the Netherlands), which is a portable device that allows for assessment of outcome measures using conventional wobble board along with visual feedback, both in a movement-measuring and an entertaining exercise/game environment [18-20]. Pedalo®-Sensomove balance device is reported to be reliable for the measurement of proprioception and reaction time with excellent test-retest reliabilty in community dwelling older adults [21]. There is, however, paucity of information related to the validity and responsiveness of the data generated from balance measures assessment using Pedalo®-Sensomove balance device. Therefore, this study was conducted to evaluate the validity and responsiveness of COP range and COP sway taken from Pedalo®-Sensomove balance device with clinical balance tests in DPN patients.
Materials and Methods
Twenty patients (males and females) with DPN were recruited through referrals from the university health center and nearby hospitals. Recruitment of subjects were done during the period from March 2016 to December 2016. They were assessed in the Human Performance Lab and trained in the gymnasium of Centre for Physiotherapy and Rehabilitation Sciences, Jamia Millia Islamia. The study was approved by the Institutional Ethical Committee, Jamia Millia Islamia, New Delhi, India, reference number: 17/9/40/JMI/IEC/2015 and a written informed consent were obtained from all participants. Ethical standards were maintained during the study according to declaration of Helsinki, 1964.
To examine the validity and responsiveness of COP range and COP sway taken from Pedalo®-Sensomove balance, a post-hoc power analysis was conducted for the sample size of 20, using the software G. Power 3.1. Based on the change in the COP range and COP sway following balance training, the effect size observed in the present study (d=0.73) revealed a power of 0.9, at an alpha level=0.05.
The inclusion criteria were; age between 45-75 years; BMI between 18.5-29.9 kg/m2; score more than 2/13 points in the Michigan Neuropathy Screening Instrument (MNSI) questionnaire, indicating the presence of at least two DPN symptoms; score greater than 1/10 point scale of MNSI physical examination, including impaired vibration perception; without any episode of plantar ulceration; no partial or total amputation and ability to walk independently in the laboratory. Exclusion criteria were: other neurological impairment; major vascular complication; severe retinopathy; severe nephropathy; severe musculoskeletal impairment to lower limb; severe cognitive impairment; cardiovascular complication; and receiving any supervised physical intervention. The participants were explained the purpose and methodology of the study.
Study Design and Procedures
This was a prospective cross-sectional study which consisted of two parts: validating the COP range and COP sway against FRT, OLS and TUG; and examining the responsiveness of the COP range and COP sway to changes in balance measures after balance exercise.
The initial assessment included demographic and anthropometric characteristics and screening for DPN, following which, the patients performed FRT, OLS, TUG, COP range and COP sway. Following familiarisation, each test was performed thrice with ten minutes of rest in between the tests. Best data from the triplicates of each test were used for analysis. The tests were re-administered in the same sequence following 8-weeks of balance exercises.
Assessment
Functional Reach Test (FRT): Subjects were asked to stand and reach as far forward as possible with arm straight in a plane parallel to the measuring device without taking step forward. Three trials were given and best was recorded. Practice trials were given to each participant. FRT is a precise (coefficient of variation=0.025), valid, and reliable measure (ICC=0.92) with established sensitivity to change (responsiveness index=0.97) [10,11].
One Leg Standing (OLS): Subjects were asked to stand on one leg with hands on waist and lift the other leg to the level of shin. The time was recorded till either the stance foot shifted in any way or the non stance foot touched the ground. Each patient performed the test first with their dominant leg and then the other leg in two conditions-eyes open (90 sec) and eyes closed (60 sec). Three trials were given and the best was used for analysis. Practice trials were given to each participant. The intra-rater and inter-rater reliability (ICC=0.93 to 0.99) have been reported to be excellent in community-dwelling older people [11].
Timed Up and Go test (TUG): The TUG is commonly used to examine functional mobility in community-dwelling, frail older adults. This test is based upon the time (in seconds) that a participant takes to stand up from an armchair, walk a distance of 3 m, turn, walk back, and sit down on the chair. The subjects were barefoot while performing this test and used their walking aids. Best of three trials were recorded for analysis. The time required to perform TUG is strongly related to the risk of falls. Healthy adults who are able to perform this test in a maximum of 10 seconds have lesser risk of falls, and those taking more than 14 seconds indicated high risk of falls [13]. This test has good intra-rater and inter-rater reliability (ICC=0.8 to 0.99) [13,22].
Pedalo®-Sensomove Balance Testing
Pedalo®-Sensomove balance device consists of miniboard which is a circular board with hemispheral shaped sensors placed below it and works as three-dimentional accelerometer and gyroscope with a sample frequency of 100 Hz. A 3.5 cm cushion was placed below the miniboard. The sensors are connected with the personal computer. Once the board was positioned, the device was calibrated such that the cursor or marker (representing the subjects’ COP) stays at the center. Participants were instructed to remove their shoes and step on to the board, with feet placed 4-5 cm apart. The visual display of the monitor was adjusted at the subjects’ eye level. Subjects were instructed not to move their feet and hands were placed at the level of pelvis.
The standard test protocol was administered, comprising of two tests: a) COP range in four different directions (front, back, left and right) and b) COP sway (AP and ML). COP range required subjects to shift their COG through focusing on the display monitor by movement of the cursor from the center. Subjects were asked to tilt maximally in four directions (front, back, left and right). Each subject was instructed to hold the end position for 3 seconds, return to the center, and then perform for the other direction. The maximal tilt angle was recorded as COP range in each direction.
COP sway test requires subjects to look straight ahead while standing as still as possible, focusing on the display monitor using visual feedback to maintain the position of the marker within centrally positioned target box. Subjects were asked to maintain upright position for 30 seconds. Verbal cues were given “look at the colored spot; maintain upright position with spot in the centre as much as possible”. COP sway AP and ML was calculated as an average of front-back deviation and average of left-right direction respectively. Assuming that the movement about the ankle (with a fixed foot position) resembles inverted pendulum, and delimit the area over which the COG can safely move without changing the base of support.
Statistical Analysis
Data analysis was done using SPSS version 21 and all graphs were made on GraphPad Prism (Version 5.01), with significant level set at p≤0.05. Shapiro-Wilk test was used to determine normality of distribution and data that was not normally distributed was analysed using non-parametric test.
The construct validity was established by evaluating the relationship of COP range and COP sway with FRT distance (using pearson correlation coeffecient) and OLS (using spearman correlation coefficient). The concurrent validity was examined by assessing the correlation of COP range and COP sway with TUG scores (using pearson correlation coefficent). The strength of correlation was interpreted as negligible (0-0.3), low (0.3-0.5), moderate (0.5-0.7), high (0.7-0.9), and excellent (0.9-1.0).
Responsiveness was examined by comparing the changes in COP range and COP sway after completion of eight weeks of balance exercises. In this study, Effect Sizes (ESs) and Standardised Response Means (SRMs) were used to assess responsiveness. ES was calculated by dividing observed mean change by SD of the baseline score. An ES of >0.8 was considered large, 0.5 to 0.8 moderate, and 0.2 to 0.5 small. SRM was calculated as observed mean change divided by SD of the difference scores. A value of SRM <0.5 was considered to be insensitive to change.
Results
Demographic characterstics of the subjects are presented in [Table/Fig-1]. Quantitative data is expressed in mean and SD and qualitative variables are expressed in frequency and percentage.
Demographic characterstics of the participants.
| Subject characterstics | Value |
|---|
| Sample | 20 |
| Age (years) | 60.45±8.79 |
| Sex (Male/Female) | 14/6 |
| Height (cm) | 164.12±8.77 |
| Weight (kg) | 66.57±13.56 |
| BMI (kg/m2) | 24.57±3.29 |
| Diabetic duartion (years) | 13.87±6.25 |
| Type 1/Type 2 | 2/18 |
| HbA1C (%) | 8.07±1.23 |
| RBG (mg/dL) | 178.5±61.93 |
| MNSI (Q) | 4.3±1.68 |
| MNSI (Ph) | 3.07±1.18 |
| On medication (Oral/Oral+Insulin/Insulin) | 13/5/2 |
| Smoking or tobacco (P/Ab) | 3/17 |
| Number of comorbidities (0/1/2) | 10/6/4 |
| Number of falls (0/1/2) | 12/3/5 |
BMI: Body mass index; HbA1C: Glycosylated heamoglobin; RBG: Random blood glucose; MNSI: Michigan neuropathy screening instrument; Q: Questtionaire; Ph: Physical assessment; P: Present; Ab: Absent
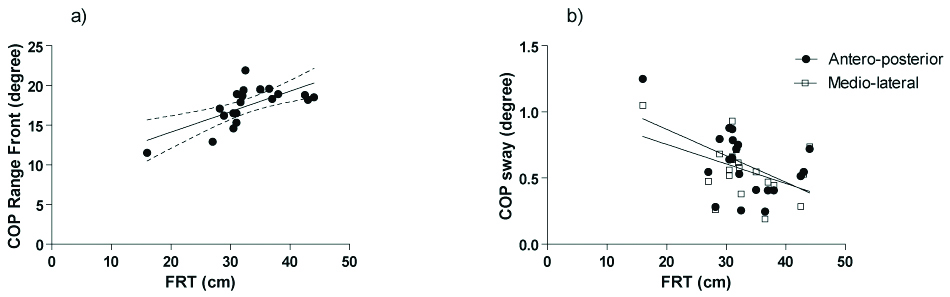
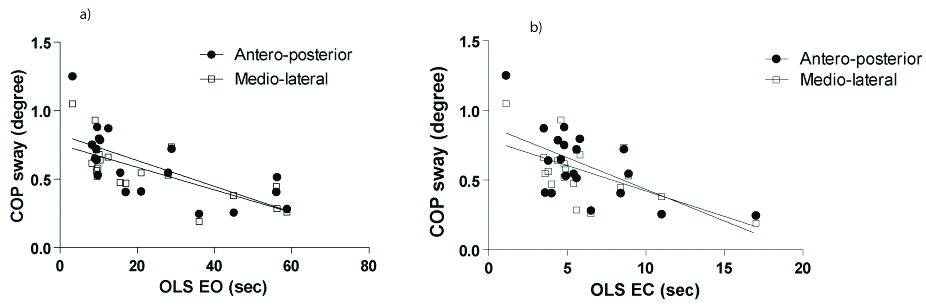
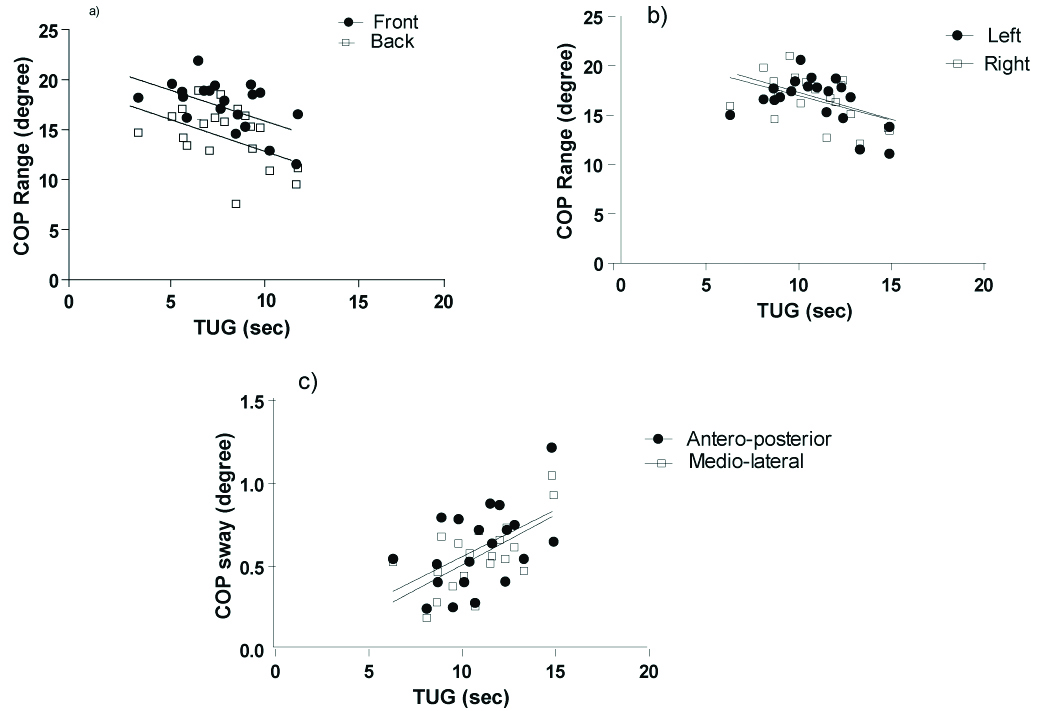
COP range front (r=0.665, p=0.001) demonstrated significant moderate positive correlation with FRT. COP sway (AP: r= -0.51, p=0.022; ML: r= -0.449, p=0.047) was found to be negatively related with FRT [Table/Fig-2]. OLS EO showed a significantly positive correlation to COP range (front: r=0.487, p=0.029; right: r=0.501, p=0.025) and yielded high negative correlation with COP sway (AP: r= -0.729, p≤0.001; ML: r= -0.747, p≤0.001). Similar association was found between OLS EC and COP sway (AP: r= -0.514, p=0.02; ML: r= -0.467, p=0.038) [Table/Fig-3]. On the contrary, TUG score correlated positively with COP range (front: r= -0.555, p=0.011; back: r= -0.474, p=0.035; left: r= -0.464, p=0.039; right: r= -0.505, p=0.023), and negatively with COP sway (AP: r=0.505, p=0.023; ML: r=0.643, p=0.003) [Table/Fig-4]. [Table/Fig-5] states the details of correlation.
Correlation between the FRT distance with a) COP range Front and b) COP sway AP and ML.
Correlation between the COP sway with a) OLS EO and b) OLS EC.
Correlation between the TUG (time) with a) COP range Front-back, b) COP range left-Right and c) COP sway.
Correlation matrix of the outcome variables.
| FRT | TUG | OLS EO | OLS EC |
|---|
| COP range Front | 0.665** | -0.555* | 0.487* | 0.414 |
| COP range Back | 0.303 | -0.474* | 0.414 | 0.197 |
| COP range Left | 0.223 | -0.464* | 0.342 | 0.001 |
| COP range Right | 0.387 | -0.505* | 0.501* | 0.427 |
| COP Sway AP | -0.51* | 0.505* | -0.729** | -0.514* |
| COP sway ML | -0.449* | 0.643** | -0.747** | -0.467* |
FRT: Forward reach test; TUG: Time up and go test; OLS: One leg stance; EO: Eyes open; EC: Eyes closed; COP: Centre of pressure; AP: Antero-posterior; ML: Medio-lateral; *Significant at p≤0.05; **significant at p≤0.01
The ES and SRM for changes were found to be moderate in the COP range front (ES=0.77, SRM=1.12), COP range left (ES=0.73, SRM=0.827), COP sway AP (ES=0.74, SRM=1.19) and COP sway ML (ES=0.71, SRM=0.92); and high in COP range back (ES=0.808, SRM=1.15), and COP range right (ES=0.93, SRM=1.38).
Discussion
The present study aimed to evaluate the construct, concurrent validity, responsiveness of the COP range and COP sway by Pedalo®-Sensomove balance device in patients with DPN and our findings support the suitability of these balance measures in patients with DPN.
The association of FRT with the COP range in front direction supports the consruct validity of the COP range indicating Limit Of Stability (LOS) in forward direction. FRT is a clinical measure which reflect limits of stability in anterior direction as reported by Duncan PW et al., [10]. Similarly, COP range front in Pedalo®-Sensomove balance device also measures the shifting of COG in the anterior direction without changing the base of support. Previously FRT demonstrate very high test-retest reliability; construct, concurrent, criterion and predictive validity; and sensitivity to change [10,23-25].
Our results also showed that the COP range in all direction has a negative correlation with TUG. COP range as LOS is a measure of dynamic stability while TUG is a measure of functional balance. The findings of this study suggest that these two components of balance measure are related to each other implying that a lesser TUG value (better functional balance) have higher LOS (shifting of COG in different direction without changing the base of support). However, the Pedalo®-Sensomove balance device maintains foot position in unstable platform that can cause changes in the size of base of support, although still fulfilling the operational defination of LOS, can be termed as dynamic LOS. In the present study, TUG was found to be positively correlated with COP sway AP and ML, thus demonstrating concurrent validity between these two measures of dynamic balance i.e., the better the balance, the faster the TUG speed (lower score) and the smaller the sway (less score).
The construct validity of COP sway in the present study is supported by its significant correlation with OLS EO and EC conditions. COP sway was recorded in presence of visual feedback which closely resembles OLS EO, thus showed a strong correlation. On the other hand OLS EC is a more challenging conditions, where patients were not able to hold the position for longer duration, which could be the reason for the low to moderate association. COP sway also showed correlation with TUG (positively correlated) and FRT (negatively correlated). Lin MR et al., showed that the TUG and FRT had excellent test-restest reliability and validity [11]. Studies state that the TUG is most appropriate for older people who are frailer, and OLS and FRT are more suitable for healthy older people [11,26], DPN subjects were able to successfully complete the COP sway test using Pedalo®-Sensomove balance device indicating that the device is valid for use in the DPN population.
The responsiveness of the COP range showed moderate to large ES (0.729 to 0.93) and SRM (0.827 to 1.38); similarly COP sway, evaluated through ES (0.71 and 0.74) and SRM (0.92 and 1.19), was found moderate. It detect the changes in these balance parameters for the patients affected with balance or postural control.
Limitation
First we studied a relatively small number of patients; second, a greater number of subjects exhibited mild to moderate level of neuropathy while those with severe neuropathy were relatively less in number. Therefore, these results may not be extrapolated to those with a severely affected DPN. In future studies, a larger group of people should include validating the measures of balance taken through Pedalo®-Sensomove balance system.
Conclusion
In summary, the present study substantiates that the COP range and COP sway measured by Pedalo®-Sensomove balance device are valid and responsive measures of balance in patients with mild to moderate DPN. It is a less expensive and portable device, that can be used as an alternative tool for the evaluation of the balance measures.
BMI: Body mass index; HbA1C: Glycosylated heamoglobin; RBG: Random blood glucose; MNSI: Michigan neuropathy screening instrument; Q: Questtionaire; Ph: Physical assessment; P: Present; Ab: Absent
FRT: Forward reach test; TUG: Time up and go test; OLS: One leg stance; EO: Eyes open; EC: Eyes closed; COP: Centre of pressure; AP: Antero-posterior; ML: Medio-lateral; *Significant at p≤0.05; **significant at p≤0.01