Worldwide, Cervical Cancer is considered as the second most common malignancy in women. In India, cervical cancer is the second most common cancer that leads to death in women after breast cancer [1]. Pap smear is a microscopic examination of cervical cells and is used to detect cancerous, pre-cancerous or benign conditions of the cervix [2]. The concept behind the Pap test is that cellular changes that may develop into cancer are detected at an early stage, thus preventing cancer [3]. Pap smear examination is the primary test for screening cervical cells [4].
There are many factors which may affect the reliability of Pap test like error in sample collection, presence of haemorrhagic material, lack of concentration, poor contrast etc. Objective techniques can be helpful in preventing false interpretation, in distinguishing borderline cases and thus better and timely treatment of patient [5]. Computer-assisted image analysis such as nuclear morphometry provides a powerful tool for high-precision measurement of several variables characterising the size and shape of cancer cell nuclei in conventional Pap smear [6]. Morphometry is a quantitative technique that describes the structure and features of cell undergoing metaplastic change taking different parameters in account [7]. The microscopic image is recorded by a digital camera and displays on a computer screen and then nuclear areas and various other parameters are computed using an image analysis software which is able to produce a quantitative data in form of cytograms and histograms [8]. The parameters that can be evaluated by morphometry are Nuclear Area, Cytoplasmic Area, Nucleus to cytoplasmic ratio, Perimeter, Diameter, Axis etc., [7].
This present study was conducted to find the significance of nuclear morphometry pattern in differentiating between ASC-US, ASC-H, LSIL, HSIL and SCC. ASC:SIL ratio was also calculated.
Materials and Methods
This was a three year retrospective and two year prospective study conducted from June 2013 to July 2018 on Pap smears received in cytology laboratory of pathology department at Subharti Medical College and associated Chhatrapati Shivaji Hospital, Meerut, Uttar Pradesh, India. Retrospective cases were retrieved from the saved departmental data and archived filed slides. No issue related to fading of slide was experienced as the slides of only three years were retrieved. The Institutional Ethics Committee clearance was obtained prior to commencement of study (Ethical number–SMC/EC/2016/99). Consent of the patient was taken before conducting the test. Pap Staining of cervical smear was done because of limitation of sample received (one slide per case) and for better visualisation and differentiation of cytoplasmic and nuclear features. Pap smears were reported according to The Bethesda System 2014 [9]. Pap smear reported as epithelial cell abnormality and Pap smear showing reactive cellular changes were included in the study whereas “inflammatory cervical smear without epithelial cell abnormality and reactive cellular changes”, women in their menstruation period were excluded from the study. A total of 163 cases (26 retrospective and 137 prospective studies) including 85 (26 retrospective and 59 prospective) epithelial cell abnormality (ASC-US, ASC-H, LSIL and HSIL) and malignant cases (SCC), 78 reactive cases (all prospective) were received in the department over a period of five years. Twenty normal control were also observed. Morphometric analysis of 163 cases and 20 control cases were done.
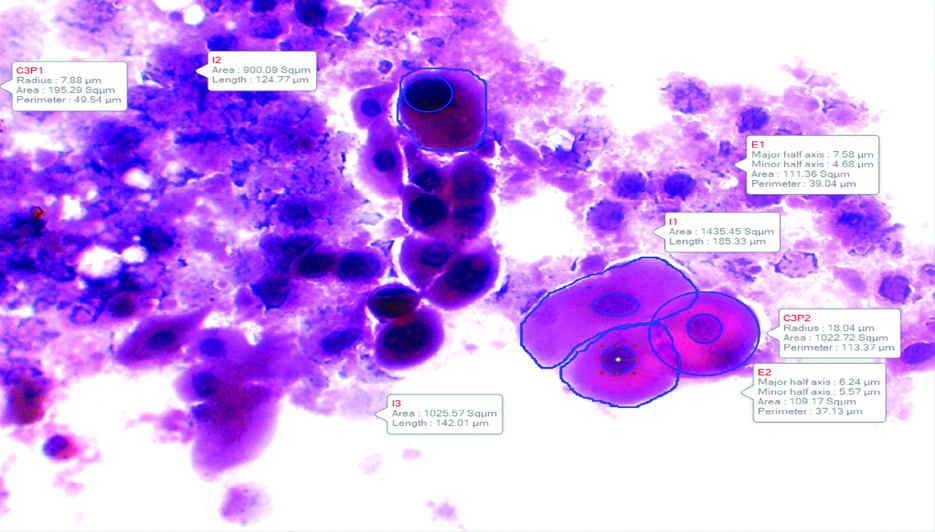
Nuclear Morphometry analysis was done on Pap smears with the help of Image Analyzer Software Motic Image Plus 3.0 at magnification of 400X and were stored in the computer. 20 squamous cells per slide were analysed. Cell area, cell perimeter, nuclear area, N:C ratio and nuclear diameter were noted.
Statistical Analysis
The mean and standard deviation were calculated and the results were compared between the different groups using SPSS Software Version 19.0. Student’s t-test was used as the test of significance. p-value of <0.05 was considered as statistically significant.
Results
A total of 163 cases out of which 85 cases (26 retrospective and 59 prospective) of epithelial cell abnormality (83 cases) and malignant cases (2 cases) and 78 reactive cases (all prospective) were analysed. The results obtained were compared with a control group of 20 cases. Age in the control group ranged from 21 to 70 years. Maximum number of patients belonged to 21-30 years of age (45%) followed by 41-50 years of age (25%). The age of patients diagnosed as reactive cellular changes ranged from 21 years to 70 years. The age of patients diagnosed with epithelial cell abnormality (ECA) ranged from 28 years to 85 years [Table/Fig-1].
Comparison of age wise distribution between reactive cellular change and epithelial cell abnormality.
| Age group (in years) | Reactive cellular change | Epithelial cell abnormality |
|---|
| 21-30 | 13 (16.6%) | 02 (2.3%) |
| 31-40 | 29 (37.2%) | 14 (16.5%) |
| 41-50 | 26 (33.3%) | 35 (41.2%) |
| 51-60 | 4 (5.2%) | 18 (21.1%) |
| 61-70 | 6 (7.7%) | 14 (16.5%) |
| 71-80 | 0 | 1 (1.2%) |
| 81-90 | 0 | 1 (1.2%) |
| Total | 78 | 85 |
The Pap smears were reported according to The Bethesda System 2014 and were categorised as Reactive cellular change (78 cases), ASC-US (55 cases), ASC-H (four cases), LSIL (four cases), HSIL (20 cases) and SCC (2 cases). Inflammation is seen in 93.3% (152/163) cases and 64.7% (55/85) epithelial cell abnormality cases were associated with reactive cellular changes. Tumour diathesis was present in 18.8% (16/85) cases reported as ECA. None of the reactive cases showed tumour diathesis. Number of ASC (ASC-US and ASC-H) reported were 59 and SIL (LSIL, HSIL and SCC) were 26 in number. ASC:SIL ratio was observed to be 2.2:1.
Nuclear parameters were analysed among normal control group, reactive cases and ECA cases [Table/Fig-2] and were further compared [Table/Fig-3]. Nuclear parameters analysed were cell area, cell perimeter, nuclear diameter, nuclear area and N:C ratio for normal control group [Table/Fig-4], reactive cellular changes [Table/Fig-5] ASC-US [Table/Fig-6], ASC-H, LSIL [Table/Fig-7], HSIL [Table/Fig-8] and SCC [Table/Fig-9]. Mean and standard deviation (SD) were calculated [Table/Fig-2]. It was observed that there was gradual increase in nuclear area and nuclear diameter from normal cell to dysplastic cell to SCC. There was gradual increase in N:C ratio from normal group to SCC except for LSIL which was lower than ASC-H. There was gradual decrease in cell area from normal cell to dysplastic cell to SCC except for LSIL which was more than ASC-H and there was gradual decrease in cell perimeter from normal group to SCC except for ASC-H which was greater than LSIL, HSIL and SCC.
Nuclear morphometry parameters in various categories.
| Category (Mean±SD) | Cell area (Mean±SD) (μm) | Cell perimeter (Mean±SD) (μm) | Nuclear area (Mean±SD) (μm) | Nuclear diameter (Mean±SD) (μm) | N:C ratio (Mean±SD) (μm) |
|---|
| Normal control group (N=20) | 4954.46±1461.32 | 352.27±48.45 | 97.31±23.35 | 12.92±1.87 | 0.02±0.01 |
| Reactive cellular changes (N=78) | 3388.52±922.84 | 258.69±43.99 | 165.51±35.91 | 15.93±2.26 | 0.05±0.03 |
| Epithelial cell abnormality (N=85) | ASC-US (N=60) | 2292.46±663.23 | 214.65±36.59 | 183.30±42.76 | 16.69±1.96 | 0.10±0.04 |
| ASC-H (N=5) | 1471.65±791.63 | 175.75±50.19 | 182.18±76.93 | 16.72±1.58 | 0.16±0.06 |
| LSIL (N=4) | 2308.20±124.09 | 219.15±6.32 | 188.68±23.59 | 18.13±1.41 | 0.09±0.01 |
| HSIL (N=14) | 1975.90±687.69 | 205.96±33.54 | 237.14±74.19 | 20.04±4.13 | 0.16±0.09 |
| SCC (N=2) | 1644.15±294.21 | 183.55±18.24 | 314.23±26.17 | 26.98±2.02 | 0.25±0.08 |
Comparison between different pair of categories for different nuclear morphometry.
| Pair of categories | Probable values of independent “T” test for different nuclear morphometry |
|---|
| Cell area | Cell perimeter | Nuclear area | Nuclear diameter | N:C ratio |
|---|
| Normal vs Reactive | p<0.01 (VS*) | p<0.01 (VS*) | p<0.01 (VS*) | p<0.01 (VS*) | p<0.01 (VS*) |
| Normal vs Epithelial cell abnormality | p<0.01 (VS*) | p<0.01 (VS*) | p<0.01 (VS*) | p<0.01 (VS*) | p<0.01 (VS*) |
| Reactive vs Epithelial cell abnormality | p<0.01 (VS*) | p<0.01 (VS*) | p<0.01 (VS*) | p<0.01 (VS*) | p<0.01 (VS*) |
| Reactive vs ASCUS | p<0.01 (VS*) | p<0.01 (VS*) | p<0.01 (VS*) | p<0.01 (VS*) | p<0.01 (VS*) |
*VS: Very significant
Nuclear morphometric analysis of normal cervical smear (Pap stain 400X).
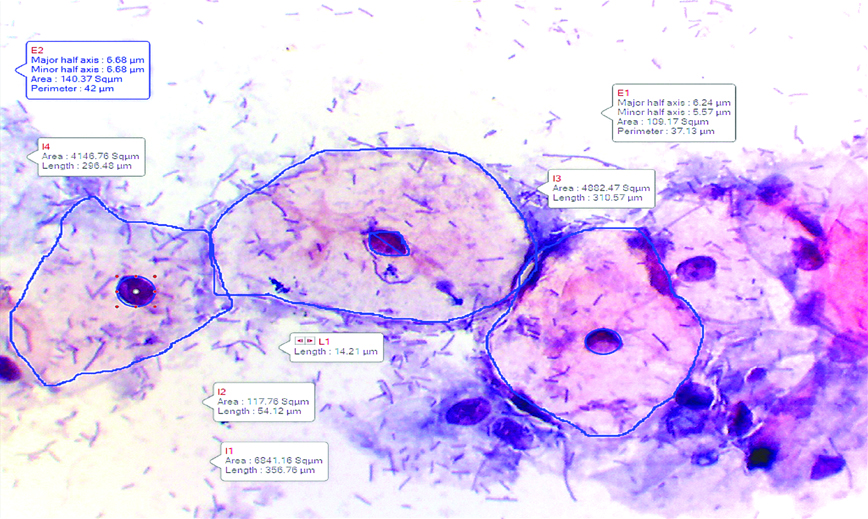
Nuclear morphometric analysis of reactive cellular changes (Pap stain 400X).
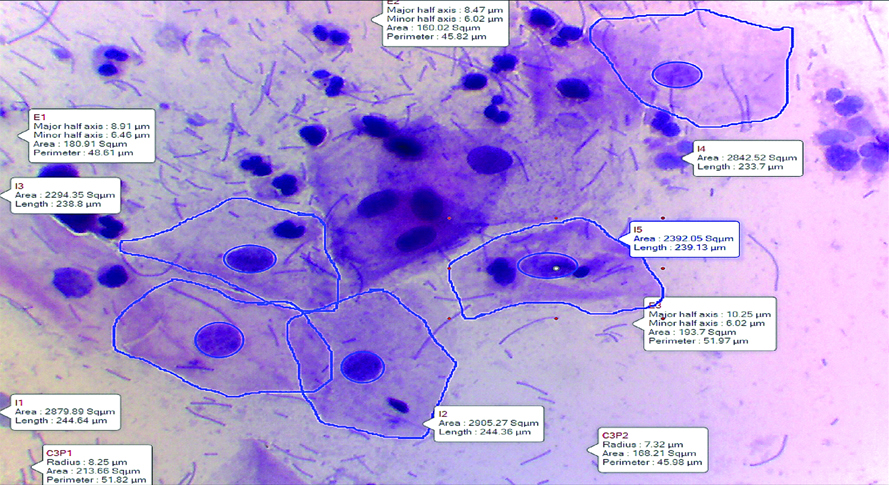
Nuclear morphometric analysis of ASC-US (Pap stain 400X).
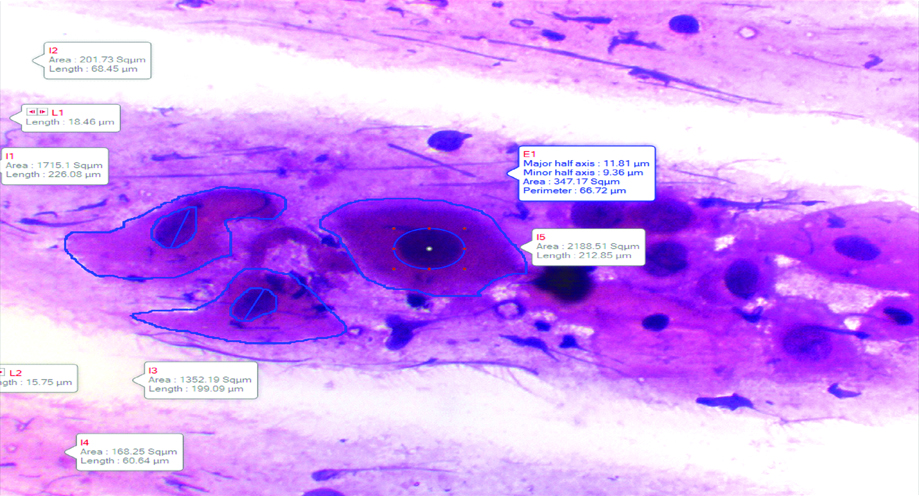
Nuclear morphometric analysis of LSIL (Pap stain 400X).
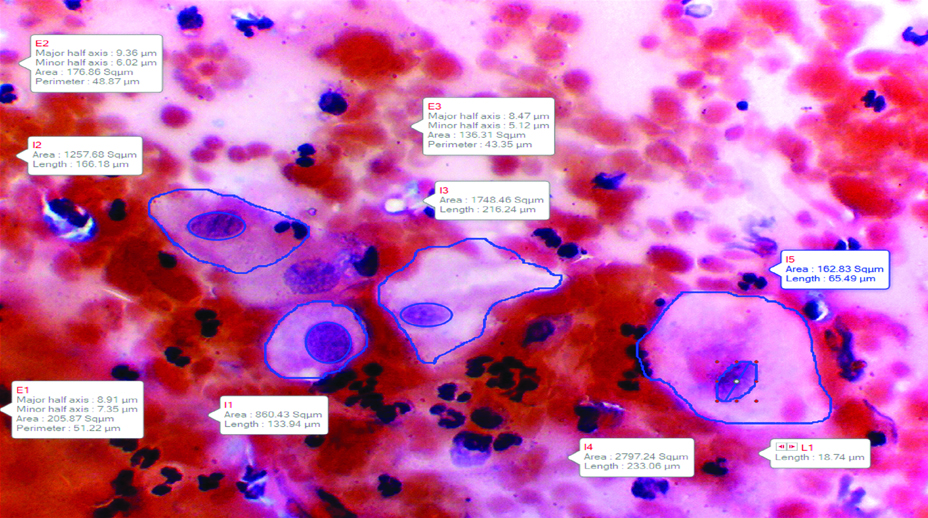
Nuclear morphometric analysis of HSIL (Pap stain 400X).
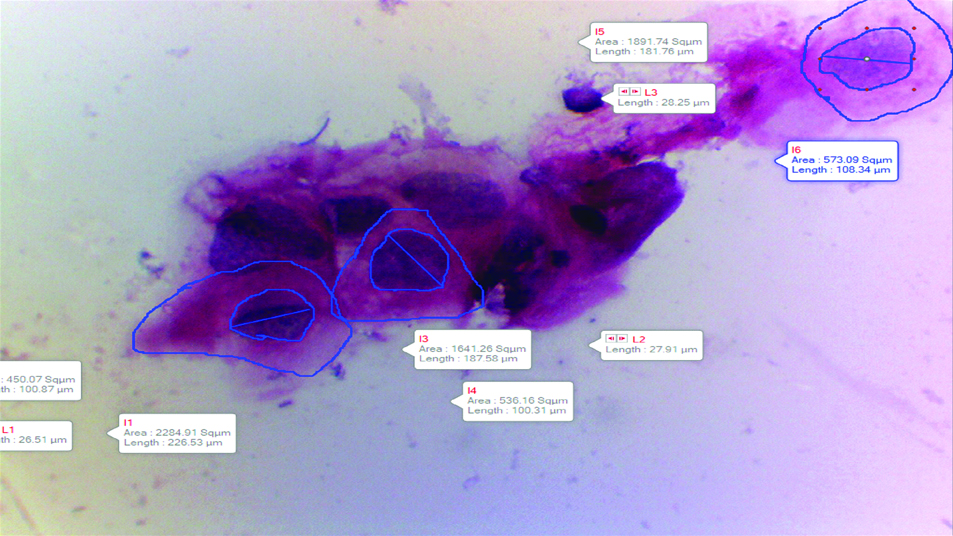
Nuclear morphometric analysis of SCC (Pap stain 400X).
In present study, on comparing normal control group with reactive cases, normal with ECA cases, reactive cases with ECA cases and Reactive with ASC-US, all the five parameters observed i.e. cell area, cell perimeter, nuclear area, nuclear diameter and N:C ratio were found to be statistically significant. Reactive cases were compared with ASC-US because of minimal microscopic differences between the two groups [Table/Fig-3].
Histopathological diagnosis was available in 22.4% (18/85) cases. Out of 18 cases, 94.4 % (17/18) cases showed cyto-histopathological correlation (malignant reported as malignant) and 5.6% (1/18) cases showed non-consensus. The case showing non-consensus was reported as Inflammatory cervical smear while on histopathological examination, it was reported as squamous cell carcinoma.
Discussion
Cervical cancer is a major cause of cancer mortality in women [10]. It is the fifth most common cancer in humans worldwide [11]. It has been estimated that an average woman under 40 years of age has 2% chance of developing cervical carcinoma [12]. This malignancy is ideal for screening as it meets both test and disease criteria for screening [13]. Pap smear has been extensively investigated and used as a screening test for cervical cancer [4]. Since the visual screening of Pap smear in various screening programs can be very demanding, tedious and can be tiring, so automated analysis of Pap test such as nuclear morphometry can be considered to improve diagnostic sensitivity [3].
In the present study, the age of patients diagnosed as cases of ECA ranged from 28 years to 85 years with the mean age of 50.5 years. Majority of the patients diagnosed with ECA were in fifth decade 41.2% followed by 21.1% in sixth decade. This is comparable to a study conducted by Lakshmi AB et al., in which the age of patients who presented with epithelial cell abnormality ranged from 30-70 years of age being highest in 5th decade [7]. In the present study, out of 85 ECA cases, 33.7% were reported as ASC-US, followed by 12.3% cases reported as HSIL, 2.5% as ASC-H and LSIL and 1.2% as SCC. Lakshmi AB et al., found the similar findings in their study [7]. However, in studies conducted by Bal MS et al., and Bukhari MH et al., maximum number of ECA cases were reported as LSIL, followed by HSIL, SCC and ASCUS [13,14]. The reasons behind this could be late screening of patients for cervical cancer, lack of awareness, could be error in reporting of Pap smear.
In present study, ASC:SIL was calculated which came out to be 2.2:1. It was within the range i.e. below 3:1 depicting the good quality control in cytopathology laboratory. Similar findings were observed in study conducted by Hemalata J et al., (1.1:1) and Renshaw AA et al., (0.87:1) [15,16].
There are various problems associated with Pap test like error in sample collection, only 20% of harvested cells are transferred on the slide and error which may be major contributors to false-negative readings of Pap smears [17,18]. To minimise the false negative results, utilisation of quantitative techniques, based on the evaluation of parameters has been suggested. Application of ancillary techniques such as Nuclear Morphometry is useful in providing an objective and reproducible diagnosis [19]. Morphometry is a quantitative description of geometric features of structures such as cells, nuclei or nucleoli.
In the present study, it was observed that there was a gradual increase in nuclear area from normal cell to dysplastic cell to SCC. Divya Rani MN et al., found that nuclear diameter showed a significant difference between LSIL and HSIL, LSIL and SCC, LSIL and HSIL and nuclear area showed a significant difference on comparing LSIL with HSIL and LSIL with SCC [18]. Viajyshree R et al., and Chen YF et al., also found a significant difference in comparing mean of nuclear area [Table/Fig-10] [20,21].
Comparison of result of nuclear area in different categories.
| Normal cell | Reactive cases | ASC-US | ASC-H | LSIL | HSIL | SCC |
|---|
| Present study (n=183) | 97.31±23.35 μm | 165.51±35.91 μm | 183.30±42.76 μm | 182.18±76.93 μm | 188.68±23.59 μm | 237.14±74.19 μm | 314.23±26.17 μm |
| Divya Rani MN et al., [18] Study (n= 60) | - | - | - | - | 109.54±11.13 μm | 132.7±17.31 μm | 142.27±26.67 μm |
| Viajyshree R et al., [20] | 710.35±100.25pixels | 974.32±329.56pixels | 1866.57±1169.33pixels | - | 1784.73±1187.11pixels | 2486.16±1229.84pixels | 2340.19±1515.57pixels |
The gradual increase in mean diameter with lesion was observed in present study. Similar findings were observed by Divya Rani MN et al., [18]. However, Vijayshree R and Rao KR, in their study found that the mean nuclear diameter of LSIL was smaller than ASC-US and of SCC was less than HSIL [Table/Fig-11] [20]. Chen YF et al., also found a significant difference in diameter of normal cell from dysplastic epithelial cell [21].
Comparison of result of nuclear diameter in different categories.
| Normal cell | Reactive cases | ASC-US | ASC-H | LSIL | HSIL | SCC |
|---|
| Present study (n=183) | 12.92±1.87 μm | 15.93±2.26 μm | 16.69±1.96 μm | 16.72±1.58 μm | 18.13±1.41 μm | 20.04±4.13 μm | 26.98±2.02 μm |
| Divya Rani MN et al., [18] Study (n=60) | - | - | - | - | 7.72±0.45 μm | 8.48±0.56 μm | 9.06±0.86 μm |
| Viajyshree R et al., [20] | 29.99±2.09pixels | 35.21±20.46pixels | 48.73±38.57pixels | - | 47.65±38.87pixels | 56.25±39.59pixels | 54.57±43.91pixels |
Another parameter analysed were N:C ratio, cell area and cell perimeter of different categories. Cell area and cell perimeter of ECA are the two perimeters that are least observed by morphometry till date. Cell area and cell perimeter are generally large in ASC-US as it is observed in large mature cells and gradually decreases to HSIL as it is observed in small immature cells [9]. In present study, mean cell area and mean cell perimeter of different lesion gradually decreased in size except for ASC-H which has lowest mean cell area and cell perimeter. In present study, mean cell area and mean cell perimeter of different lesion gradually decreased in size except for ASC-H which has lowest mean cell area and cell perimeter. The reason behind lower mean area of ASC-H could be because of lower sample size of ASC-H cases which makes it incomparable with other categories. The present authors could not find any study in the literature to our best knowledge to compare the results of mean cell area and cell perimeter.
In present study, on comparing normal control group with reactive cases, normal with ECA cases, reactive cases with ECA cases and Reactive with ASC-US, all the five parameters observed i.e., cell area, cell perimeter, nuclear area, nuclear diameter and N:C ratio were found to be statistically significant [Table/Fig-3]. Divya Rani MN et al., found that nuclear diameter showed a significant difference (p<0.01) between LSIL and HSIL, LSIL and SCC, LSIL and HSIL and nuclear area showed a significant difference in comparing LSIL with HSIL and LSIL with SCC [18]. However, statistically no significant difference was seen on comparing mean nuclear area of HSIL and SCC in their study. Vijayshree R and Rao KR, and Chen YF et al., also found a significant difference in comparing mean of nuclear area, nuclear diameter, N:C ratio between normal cervical cells and dysplastic cells [20,21].
Limitation
However, no reference range of morphometric parameters is available. There is need for further extensive study to establish range of morphometric parameters of cervical lesions so that morphometry can be applied to improve accuracy in cervical smear screening.
Conclusion
Nuclear morphometry is a useful quantitative tool that can be used to differentiate reactive and ECA in cervical Pap smear. They especially aid in diagnosing difficult cases that fall under the grey zone areas. So, it is concluded that nuclear morphometry if applied along with Pap smear examination can aid in differentiating and diagnosing the borderline cases and early diagnosis of squamous intraepithelial lesion. There is a need for further extensive study to establish range of morphometric parameters of cervical lesions so that morphometry can be applied to improve accuracy in cervical smear screening.
*VS: Very significant