Fever remains a challenge for physicians, more so when it lasts a month. Although infections remain the most common cause, non-infective causes should also be looked for. Adult Onset Still’s Disease (AOSD) is a rare cause of fever. It is a diagnosis of exclusion. Here, we present the case report of a young male patient, admitted with high grade fever, for more than a month and after excluding infective causes and common autoimmune diseases we kept the possibility of Still’s disease. He was treated with steroid pulse therapy followed by oral steroid. He was on follow-up for six months and is doing well.
Multisystem inflammatory disorder, Pyrexia of unknown origin, Serum ferritin
Case Report
An 18-year-old boy presented with fever with chills and rigors since past one month. There were no localising symptoms. Fever was continuous, high grade (102-104°F), associated with decrease appetite. There were no rashes, cough, headache and red eyes. He had joint pain for 10-14 days involving right knee, both elbow and both shoulder, which subsided on its own. There was no swelling accompanying the joint pain. There was no family history of any autoimmune disorder, tuberculosis and joint pain and there was no significant medical history.
On examination, he had temperature of 104°F. There was no lymphadenopathy, or pallor. Systemic examination revealed no abnormality. We kept the possibility of tuberculosis with unknown site, or enteric fever. Basic investigations were done along with paired blood and urine culture. Serial haemogram are summarised in [Table/Fig-1]. All cultures were sterile.
Serial haemogram of the patient.
| At admission | After pulse steroid | 1 week after discharge |
|---|
| Hb (gm%) | 8.8 | 9 | 10.4 |
| TLC (per cumm) | 43130 (P92L6) | 5080 (P72L25) | 17000 (P62L30) |
| Platelet (x103/cumm) | 228 | 286 | 371 |
| ESR (mm in1st hour) | 54 | 40 | 30 |
Treatment was started with Ceftriaxone and Azithromycin along with antipyretics. The fever did not subside. We further investigated him with CECT chest and abdomen, ANA /RA factor, Rk-39, Mantoux test, and TSH-all of which came out to be normal. On 10th day, he developed sudden pulmonary oedema. He was shifted to ICU, his Brain-Type Natriuretic Peptide (BNP) was significantly raised, echocardiography revealed moderate pericardial effusion without tamponade. Chest radiograph showed bilateral pleural effusion and cardiomegaly [Table/Fig-2]. His fluid intake was restricted and diuretics (Furosemide and Aldactone) added.
X-ray chest PA view: a) At admission; b) After 10 days when patient develop pericardial and pleural effusion; c) 10 days post treatment with steroids and diuretics.
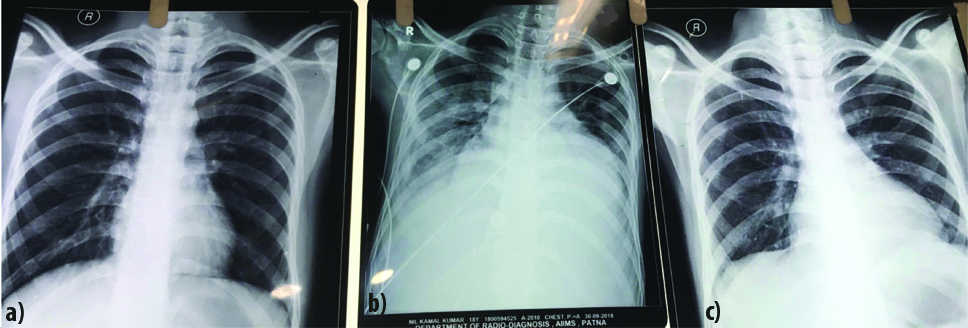
He improved in 4-5 days. Pleural tap was transudative. Sequential chest radiographs showed improvement on negative fluid balance. Bone marrow aspiration and biopsy were done, which ruled out abnormal cells or LD bodies. The serum ferritin was >1650 (normal <248 ng/mL). After excluding all the possible diagnoses, we retained the possibility of Still’s disease. We started high dose Methylprednisolone (1 gm daily for 5 days). His fever responded, TLC, ESR and CRP went down and the patient felt better.
On discharge, he received oral Prednisolone 60 mg/day for 2 weeks, then tapered slowly 5 mg/2 week. We advised him PET-CT, which showed no abnormal uptake. He was on follow-up for six months and is doing his regular activity.
Discussion
AOSD is a rare multisystem inflammatory disorder of unknown origin. Other synonyms are juvenile rheumatoid arthritis, Wisseler’s fanconi syndrome, or subsepsis allergic [1].
This disease generally affects females more than males and affects 16-35 year of age; although a retrospective study in France showed no sex bias with bimodal peak at 15-25 and 36-46 years [2], but in various studies, elderly were also found to be affected [3-5]. Pathophysiology involve genetic predisposition and a trigger by some viral or bacterial infection or stress [6,7]. HLA- B17, 8, B14, B35, DR2, DR 7, and Dw 6 are associated with increased risk. Various bacterial and viral infections were implicated for triggering the disease in various different case reports [8,9].
Clinically, it is characterised by triad of quotodian fever, salmon rash over trunk and arthralgia/arthritis. Overall incidence of these are 95.7%, 51-87% and 67-100% respectively in different studies [10,11].
Fever typically occurs at late evening, associated with sore throat, increase in arthralgia, and rash. Sometimes rashes are confused with drug allergy. Rashes are mostly seen on trunk and proximal limb, and rarely involve face. They may be mildly pruritic and occasionally show Koebner’s phenomenon [12].
Knee, wrist and ankle are the most commonly involved joints, although small joints can also be involved. Joint pain is symmetrical and usually increased during fever. Other common manifestations are myalgia, liver dysfunction, pleuritis (26.3%), pericarditis (23.8%) and splenomegaly (43%) [12].
Other rare complications include cardiac tamponade, myocarditis, Acute Respiratory Distress Syndrome (ARDS), interstitial nephritis, amyloidosis, collapsing glomerulopathy, pure red cell aplasia, Thrombotic Thrombocytopenic Purpura (TTP), seizure, and aseptic meningoencephalitis [13]. For diagnosis, various criteria are purposed [Table/Fig-3] [12,14,15].
Diagnostic criteria of adult onset Still’s disease [12,14,15].
| Yamaguchi M et al., [14] | CushJJ et al., [15] | Fautrel B et al., [12] |
|---|
| MajorFever >39°, intermittent, ≥1 week Typical rashWBC >10 000 (>80% granulocytes) | Major(2 points each)Quotidian fever >39Still’s (evanescent) rashWBC >12.0+ESR >40 mm/1st hNegative RF and ANA Carpal ankylosis | MajorSpiking fever ≥39°Arthralgia Transient erythema PharyngitisPMN ≥80%Glycosylated ferritin ≥20% |
| MinorSore throatLymphadenopathy and/orsplenomegaly LFT abnormal(−)ve ANA and RF Diagnostic combination | Minor(1 point each)Onset age <35 yearsArthritis Prodromal sore throatCervical or tarsal ankylosis | MinorMaculopapular rashLeucocytes ≥10×109/lRES involvement or abnormal LFTs Serositis |
| Exclusion criteriaInfections Malignancies Rheumatic diseasesDiagnosis5 criteria (at least 2 major) | DiagnosisProbable AOSD: 10 points with 12 wksDefinite AOSD: 10 points with 6 months | Diagnosis4 major criteria or 3 major+2 minor |
Course of disease may vary depending upon the predominant symptom. Patients with systemic disease have better prognosis than those with chronic articular defect [16].
Treatment of AOSD involves NSAID, steroids and anti-rheumatic drugs. About 70% of patients require steroids for remission. Other treatment options are methotrexate, cyclosporine A, hydroxychloroquin, azathioprin, and cyclophosphamide. Anti-rheumatic agents are used in those who are either not tolerating steroids and NSAIDS or developed adverse effects on them. They are not of proven benefit. IVIg can also be used during flares of the disease. TNF-blocker etanercept, monoclonal chimeric anti TNF-antibody infliximab, IL-1 antagonist anakinra are being used in refractory disease [17].
Conclusion
Infections predominate in the world of pyrexia, but non-infectious causes should be looked for especially in differential of Pyrexia of Unknown Origin (PUO).
[1]. Larson EB, Adult Still’s disease-recognition of a clinical syndrome and recent experienceWest J Med 1985 142(5):665-71.Available from: http://www.ncbi.nlm.nih.gov/pubmed/4013282 [Google Scholar]
[2]. Magadur-Joly G, Billaud E, Barrier JH, Pennec YL, Masson C, Renou P, Epidemiology of adult Still’s disease: Estimate of the incidence by a retrospective study in west FranceAnn Rheum Dis 1995 54(7):587-90.Available from: http://www.ncbi.nlm.nih.gov/pubmed/766890310.1136/ard.54.7.5877668903 [Google Scholar] [CrossRef] [PubMed]
[3]. Uson J, Peña JM, del Arco A, Barbado FJ, Vazquez JJ, Still’s disease in a 72-year-old manJ Rheumatol 1993 20(9):1608-09.Available from: http://www.ncbi.nlm.nih.gov/pubmed/8164226 [Google Scholar]
[4]. Steffe LA, Cooke CL, Still’s disease in a 70-year-old womanJAMA 1983 249(15):2062-63.Available from: http://www.ncbi.nlm.nih.gov/pubmed/683459610.1001/jama.249.15.20626834596 [Google Scholar] [CrossRef] [PubMed]
[5]. Chinthaka SWGJW, Satarasinghe RL, Senanayake S, Weerarathne WAPSR, Anfaz AAM, Deraniyagala MP, Noncaseating suppurative granulomatous lymphadenitis in adult onset Still’s disease - A diagnostic dilemma in a tuberculosis-endemic region: a case reportJ Med Case Rep 2018 12(1):299Available from: http://www.ncbi.nlm.nih.gov/pubmed/3031801610.1186/s13256-018-1816-730318016 [Google Scholar] [CrossRef] [PubMed]
[6]. Wouters JM, van Rijswijk MH, van de Putte LB, Adult onset Still’s disease in the elderly: A report of two casesJ Rheumatol 1985 12(4):791-93.Available from: http://www.ncbi.nlm.nih.gov/pubmed/4057203 [Google Scholar]
[7]. Sampalis JS, Medsger TA, Fries JF, Yeadon C, Senécal JL, Myhal D, Risk factors for adult Still’s diseaseJ Rheumatol 1996 23(12):2049-54.Available from: http://www.ncbi.nlm.nih.gov/pubmed/8970040 [Google Scholar]
[8]. Escudero FJ, Len Ó, Falcó V, Sevilla TF DE, Sellas A, Rubella infection in adult onset Still’s diseaseAnn Rheum Dis 2000 59(6):493Available from: http://ard.bmj.com/cgi/doi/10.1136/ard.59.6.490c10.1136/ard.59.6.490c10885978 [Google Scholar] [CrossRef] [PubMed]
[9]. Kádár J, Petrovicz E, Adult-onset Still’s diseaseBest Pract Res Clin Rheumatol 2004 18(5):663-76.Available from: https://www.sciencedirect.com/science/article/pii/S152169420400088910.1016/j.berh.2004.05.00415454125 [Google Scholar] [CrossRef] [PubMed]
[10]. Gerfaud-Valentin M, Jamilloux Y, Iwaz J, Søve P, Adult-onset Still’s diseaseAutoimmun Rev 2014 13(7):708-22.Available from: https://linkinghub.elsevier.com/retrieve/pii/S156899721400098610.1016/j.autrev.2014.01.05824657513 [Google Scholar] [CrossRef] [PubMed]
[11]. Efthimiou P, Paik PK, Bielory L, Diagnosis and management of adult onset Still’s diseaseAnn Rheum Dis 2006 65(5):564-72.Available from: http://www.ncbi.nlm.nih.gov/pubmed/1621970710.1136/ard.2005.04214316219707 [Google Scholar] [CrossRef] [PubMed]
[12]. Fautrel B, Zing E, Golmard J-L, Le Moel G, Bissery A, Rioux C, Proposal for a new set of classification criteria for adult-onset still diseaseMedicine (Baltimore) 2002 81(3):194-200.Available from: http://www.ncbi.nlm.nih.gov/pubmed/1199771610.1097/00005792-200205000-0000311997716 [Google Scholar] [CrossRef] [PubMed]
[13]. Kumar S, Sheaff M, Yaqoob M, Collapsing glomerulopathy in adult still’s diseaseAm J Kidney Dis 2004 43(5):e19.1-e19.7.Available from: https://www.sciencedirect.com/science/article/pii/S027263860400231810.1053/j.ajkd.2003.11.02515112192 [Google Scholar] [CrossRef] [PubMed]
[14]. Yamaguchi M, Ohta A, Tsunematsu T, Kasukawa R, Mizushima Y, Kashiwagi H, Preliminary criteria for classification of adult Still’s diseaseJ Rheumatol 1992 19(3):424-30.Available from: http://www.ncbi.nlm.nih.gov/pubmed/1578458 [Google Scholar]
[15]. Cush JJ, Medsger TA, Christy WC, Herbert DC, Cooperstein LA, Adult-onset Still’s disease. Clinical course and outcomeArthritis Rheum 1987 30(2):186-94.Available from: http://www.ncbi.nlm.nih.gov/pubmed/382795910.1002/art.17803002093827959 [Google Scholar] [CrossRef] [PubMed]
[16]. Masson C, Le Loët X, Lioté F, Renou P, Dubost JJ, Boissier MC, Adult Still’s disease. Part II. Management, outcome, and prognostic factorsRev Rhum Engl Ed 1995 62(11):758-65.Available from: http://www.ncbi.nlm.nih.gov/pubmed/8869217 [Google Scholar]
[17]. DeWitt EM, Kimura Y, Beukelman T, Nigrovic PA, Onel K, Prahalad S, Consensus treatment plans for new-onset systemic juvenile idiopathic arthritisArthritis Care Res (Hoboken) 2012 64(7):1001-10.Available from: http://doi.wiley.com/10.1002/acr.2162510.1002/acr.2162522290637 [Google Scholar] [CrossRef] [PubMed]