COPD is a major health problem worldwide characterised by chronic and persistent airway inflammation and airflow limitation and variable degrees of alveolar damage and emphysema. COPD accounted to approximate 6% of total deaths worldwide in 2012 [1]. COPD related deaths mostly occur due to acute exacerbation but may significantly be attributed to its complications and comorbidities. Although the primary site of the inflammation in COPD is lungs and the airways, systemic effects due to “spillover” of the inflammatory mediators have been widely discussed [2] which largely accounts for the various co-morbidities associated with the disease. Of all the co-morbidities of the disease, atherosclerosis is often neglected and remains undiagnosed. Atherosclerosis is a slow and gradually progressive condition characterised by stiffening of the blood vessels and build-up of plaque inside them, believed to start with an injury or insult to inner most lining of the arteries; the endothelium. Many risk factors have been implicated to cause these injuries which include high blood pressure, increased cholesterol intake in diet, systemic inflammatory conditions, cigarette smoking and mental stress. Ageing is the most implicated risk factor, as long as a person lives; more exposed he is to all other implicated risk factors. Cerebrovascular accidents including ischemic stroke and Transient Ischemic Attack (TIA) are second most studied implications of atherosclerosis after cardiovascular accidents. Lately, studies have highlighted towards increased risk of stroke in COPD patients [3-5].
Our study aimed to evaluate atherosclerosis of carotid arteries in terms of intima media thickness, in patients of COPD and compare with various grades of airflow limitation in Indian scenario and avoiding the common risk factors associated with atherosclerosis.
Materials and Methods
This was an observational cross-sectional study carried out at Sir Sunderlal Hospital, Institute of Medical Sciences, Banaras Hindu University from January 2013 to July 2014. The study was approved by the Institutional ethics committee (2013/EC265) and written informed consents were obtained from enrolled patients.
A total of 67 patients diagnosed with COPD were enrolled after meeting the set exclusion criteria.
The exclusion criteria were
Alternate diagnosis of dyspnea like bronchial asthma, bronchiectasis, post-tubercular fibrosis, heart failure etc.,
Associated co-morbidities like diabetes mellitus, systemic hypertension, renal disease, hepatic disease, neurological disease, coronary artery disease, left ventricular disease, arrythmias, dyslipidemia, metabolic syndrome, Obstructive sleep apneas, malignancy, other inflammatory disease.
Receiving treatment with antiplatelet, anticoagulant or statins.
ECG or 2-Dimension Echocardiography suggestive of any cardiac abnormality other than features suggestive of Cor-Pulmonale and Pulmonary Artery Hypertension secondary to COPD.
Patients with multiple organ failure (failure of two or more organ system as a result of inflammation due to injury or infection).
Active exposure to Cigarette/Bidi or Biomass fuel smoke (Patients who had not smoked/quit smoking for last 5 years and not used biomass fuel for cooking).
Haemodynamic instability (circulatory shock requiring inotrope/vasopressor support).
Patients with COPD with concomitant heart failure (on basis of echocardiography by evaluating biventricular function), Atrial fibrillation, Ischemic cardiomyopathy, coronary heart disease or history of coronary revascularization/intervention/drug treatment etc.,
History of stroke, Transient Ischemic Attack.
Those patients who were not willing to participate in study.
All patients underwent thorough physical examination and detailed medical history was recorded. COPD was established as per Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines [1]. Spirometry was performed using SpiroAir (Medisoft) device. Readings of Forced Expiratory Volume in 1st second (FEV1), Forced Vital Capacity (FVC), and FEV1/FVC ratio were recorded. Post Bronchodilator (15 minutes after inhaled Salbutamol 400 mcg) FEV1/FVC <0.7 was used to establish COPD. Severity of airflow limitation was graded based on FEV1 (percentage of predicted) value as per GOLD criteria i.e., Mild (FEV1≥0.8 of predicted), Moderate (0.5≤FEV1>0.8 of predicted), Severe (0.3≤FEV1<0.5 of predicted) and Very Severe (FEV1<0.3 of predicted).
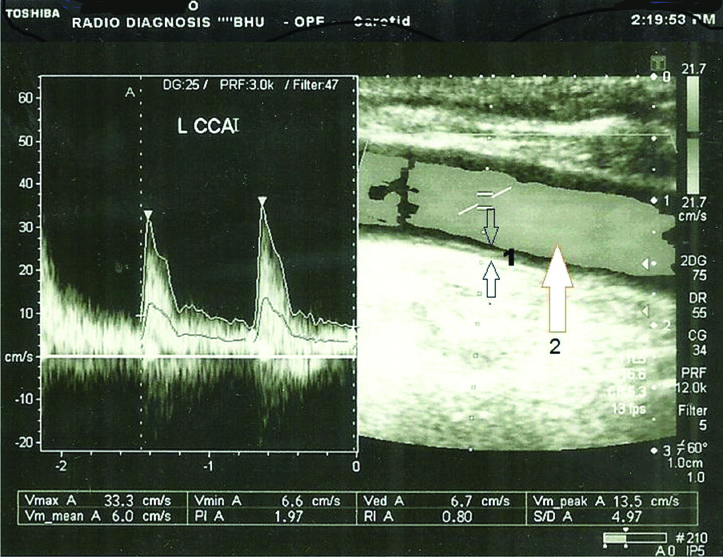
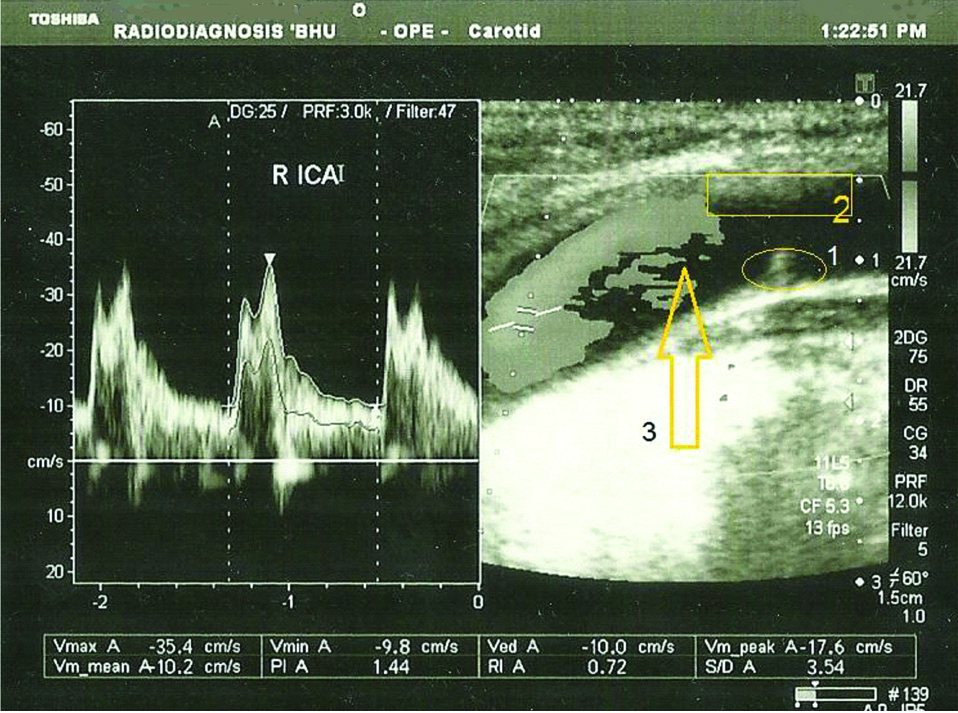
High Resolution Computed Tomography (HRCT) of thorax was done to evaluate for the imaging correlate of COPD and to exclude any other lung pathology. A colour doppler flow imaging of neck for evaluation of extra cranial carotid and vertebro-basilar systems to detect atherosclerotic changes in arterial intima-media complex along with evaluation of hemodynamics. Colour Doppler study was performed using Toshiba Xario X2 model to study axial and sagittal sections of neck vessels by Linear probe (Frequency 8-12 MHz) in supine position with pillow under the shoulder blades of patients [Table/Fig-1,2]. Gray scale images, 2-dimensional color duplex and triplex images were taken.
Colour Doppler study of left common carotid artery of 64-year-old male showing uniform intima media thickness (1) and uniform flow (2).
Colour Doppler study of Right Internal carotid artery of 67-year-old female showing non uniform marked intima media thickening (2), small partially occluding thrombus with calcification (1) and turbulent flow dynamics (3).
Results were statistically analysed using IBM’s SPSS software version 17. Pearson’s Correlation and ANOVA tests were used.
Results
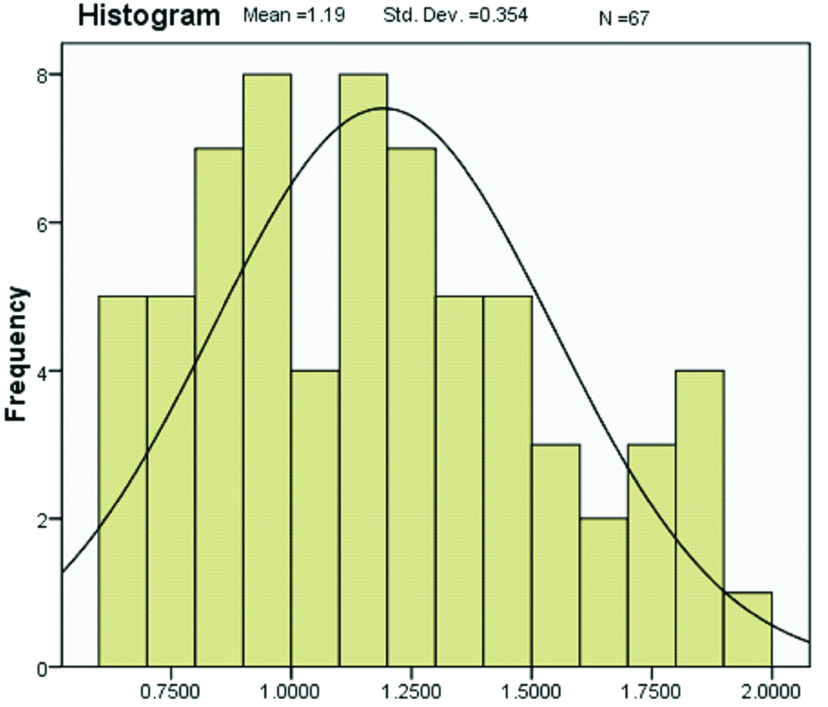
The distribution of data was assessed for normalcy and found to be of near normal distribution [Table/Fig-3] and therefore parametric tests were used. The different factors put under test were tested for significance of association. Baseline patient characteristics of our study group are shown in [Table/Fig-4]. Nearly 67% of the cases belonged to 55 to 75 years age group. The mean age was 61.91±9.07 (Median=63.00). Our study included cases with age more than 45 years only. Only 6 patients (9%) were 75 years or more of age.
Distribution of common carotid intima media thickness.
Baseline patient characteristics.
| Subject (N) | 67 |
| Age (median) | 63 |
| Male | 38 (56.7%) |
| Female | 29 (43.3%) |
| Mean Body Mass Index (Kg/m2) | 23.44±5.55 |
| Mean Total Cholesterol (mg/dL) | 168.2±6.4 |
| Mean SpO2 (%) | 90.1±2.8 |
| Mean FEV1/FVC (%) | 58.4±8.1 |
| Mean PEFR (L/sec) | 1.73±0.71 |
| Mean FEV1 (% predicted) | 42.3±14 |
| Mean CC-IMT (mm) | 1.19±0.35 |
Of the total number of cases included in the study, 55.2% belonged to Grade IV (very severe) airflow limitation while moderate and severe grade cases were equalin number; 22.4% each. No mild grade patients were present in this study.
Mean values of FEV1/FVC (%), FEV1 (% predicted), PEFR (% of predicted) are tabulated in [Table/Fig-4]. Mean CIMT was 1.19 mm±0.35 which was higher for male subgroup (1.234±0.34, N=38) compared to females (1.13±0.36, N=29). The difference in mean CIMT between males and females was not significant (t (65)=1.147, p=0.256).
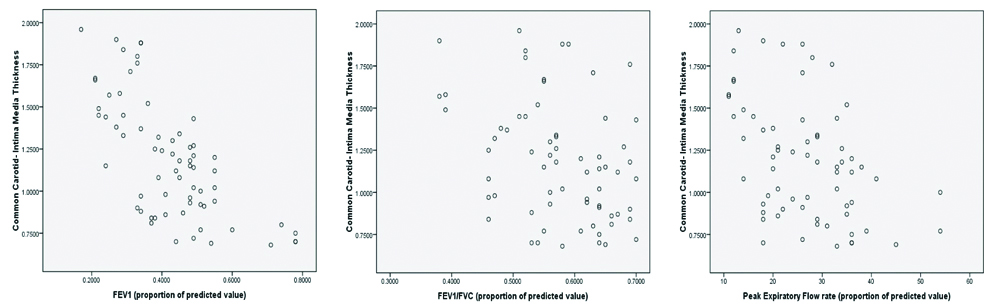
Pearson’s Correlation showed significant inverse correlation between CIMT and FEV1 (% of predicted) values with r=-0.69, p<0.001. Similar inverse and significant correlations of CIMT were found with FEV1/FVC measured (r=-0.359, p=0.003) [Table/Fig-5].
Scattered dot plot diagram showing correlation between carotid intima media thickness and FEV1 (% predicted), FEV1/FVC ratio and PEFR (% predicted).
We found significant difference in mean CIMT values for different grades of airflow limitation (GOLD grades of severity) with ANOVA F-value=32.415 and p<0.001. Post-hoc analysis of variance showed that the mean difference was higher between Grade IV and Grade II airflow limitation (MD=0.555; SE=0.066) than between Grade IV and Grade III airflow limitation (MD=0.436; SE=0.068), significant in both cases with p<0.001 (MD=Mean difference, SE=Standard Error).
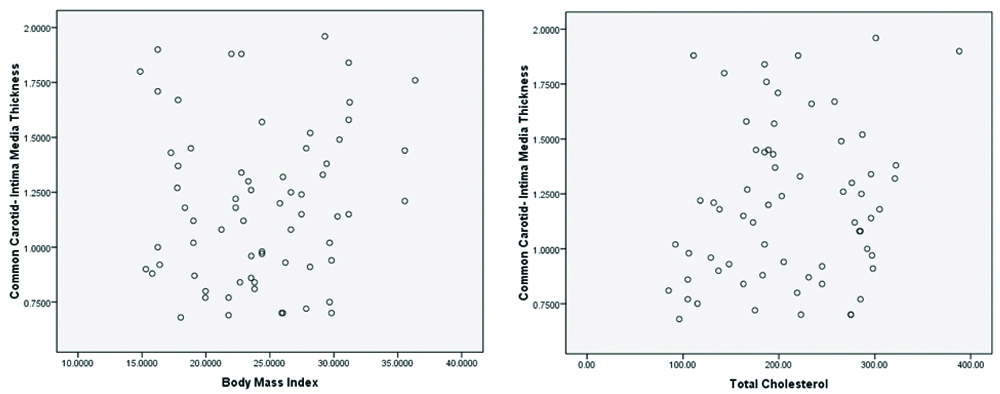
Pearson’s Correlation analysis showed insignificant correlation of CIMT values with Total Blood Cholesterol (r=0.187, p=0.137). Similarly no significant correlation was found with BMI either (r=0.106, p=0.395) [Table/Fig-6].
Scattered dot plot diagram between carotid intima media thickness and BMI and Total Cholesterol.
Discussion
In our study we have tried to ascertain the significance of carotid artery atherosclerosis; objectified by Carotid (Common Carotid) Intima Media thickness (CC-IMT) in patients of COPD. Large studies in past have found risk of stroke in patients with COPD- Truelsen T et al., after adjustment for potential confounders: sex, age, smoking, inhalation, BMI, systolic blood pressure, triglycerides, physical activity in leisure time, education, diabetes mellitus, and antihypertensive treatment, found an inverse association between FEV1 and risk of first-time stroke [6].
One study [7] described the relationship between increased CIMT and increased cardio-vascular disease risk with severity of airway obstruction in patients with COPD patients and concluded high prevalence of intima media hypertrophy and increased cardiovascular disease risk as assessed by carotid ultrasonography in COPD patients with a broad spectrum of airway obstruction severity. In another study by Köseoğlu C et al., found that increased CIMT is associated with the presence of angiographically significant CAD in patients with COPD [8]. Based on these and similar other studies we hypothesised that CIMT could be associated independently with COPD and severity of airflow limitation in absence of factors independently responsible for atherosclerosis.
In our study, the distribution of cases was comparable in males and females with 56.7% males and 43.3% females. This is to note that although the overall prevalence in men is greater in developed countries, the prevalence of COPD in women equals that in men, and there is some evidence that it may even be more severe [9]. This is attributable to the fact that though cigarette and tobacco smoking is more prevalent in men, the rural population of women in developing countries like India are chronically exposed to chulha (open oven) and biomass fuel smoke which are used for cooking purposes. Besides, bidi and hukka are common forms of tobacco smoking not very uncommon in these women.
For the total 67 cases included in the study, mean CC-IMT was 1.19 mm, with minimum thickness 0.68 mm and maximum thickness 1.96 mm. The standard deviation was 0.35. This was significantly higher than the findings of Karakas O et al., where the researchers found mean CIMT of 0.62±0.05 in 30 male Turkish COPD patients [10]. A reasonable explanation for this significant variation in mean could not be reached except for ethnic variation.
Pearson correlation analysis when used to test two continuous variables independently (without interaction with a third variable in conjunction) revealed that degree of airflow limitation (represented by FEV1) had a strong and inverse correlation with CC-IMT which was greatly significant (Correlation coefficient (R) -0.696, p-value< 0.001). This signifies that with decrease in the degree of airflow, the CC-IMT increased. This was in concurrence with all the above mentioned studies. The CC-IMT was also inversely correlated with FEV1/FVC ratio, however the strength of correlation was weaker and 2-tailed significance level (0.003) was >0.001 though <0.05. Although larger studies have previously shown correlation between FEV1 and carotid wall thickness [7,8,11-14], we have tried to evaluate this relationship in absence of potential and known independent risk factors of atherosclerosis which gives significance to ours results.
Limitation
Due to shorter duration of study and various exclusion criteria, only a limited number of cases could be screened and enrolled into the study group. A few statistical models have shown a partial overlap in the 95% confidence interval, which makes the data less reproducible in a different population group or different sample of the same population. The practical significance may differ from the calculated value. However, we have tried our best to avoid any amenable statistical error.
Conclusion
In present study too demonstrates a significant strong correlation of carotid wall thickness with airflow limitation (assessed by FEV1/FVC ratio) in COPD and inverse correlation of FEV1 (% of predicted) and PEFR (% of predicted) with CIMT in absence of independent risk factors for atherosclerosis. No significant correlation of CIMT was observed with total blood cholesterol and BMI. Large scale studies and longer follow-up is necessary to study this relationship in detail.