The success of full denture rehabilitation is directly related to factors such as retention and stability. In overdenture prostheses, retention and stability are increased, restoring oral functions such as mastication and speech, thus providing greater comfort and self-confidence for the patient [1-3]. Treatment with mandibular overdentures has become routine. This type of treatment is preferable due to improved comfort, functionality, and patient satisfaction, as well as presenting better prosthetic outcomes than those of complete removable dental prostheses [1-8]. There is no consensus in published literature on what is the ideal number of implants for the planning of overdenture prostheses, which is an important issue for correct treatment planning. Many studies [1,2,5-7,9,10] have been carried out to define the ideal quantity to be used, varying 1 to 4, but no study has been able to determine the minimal implant quantity [5,10].
Several published studies reported that two implants are the first choice for rehabilitation of mandible atrophic since it is more satisfying for the majority of patients than a conventional prosthesis [1,3,5,8,9]. However, as the bigger number of implants, the cost increases and more invasive the surgery becomes. Recent reports suggest that a single implant in the mandibular midline region is adequate for overdenture retention, and can result in a high success rate comparable to overdentures supported by multiple implants [1,5,9]. Furthermore, single implants present lower costs and minimal tissue trauma [1-3,5,7,8,11-15]. However, some authors [8,16,17] have reported high failure rates (implant losses, denture base fractures) for single-implant retained mandibular overdentures and have shown that single-implant prostheses present rotational movement when subjected to masticatory forces, becoming a larger disadvantage. Although it is already considered a viable treatment method to overdentures with a mandibular implant, there is no scientific evidence exploring the biomechanics of this type of treatment. For correct prosthetic planning, it is of fundamental importance to understand the distribution of stresses around the implant [5,8].
Beyond the number of implants, the type of connection between the abutment and implant is an essential parameter to evaluate the biomechanical behaviour of implant-supported overdentures [18,19]. There are several types of implant connections, being internal and external connections. The connections most used and studied are Morse Taper (MT), External Hexagon (EH) and Internal Hexagon (IH) [14,19]. There is also disagreement as to the best connection system. The distribution of tension in mandibular overdentures is well documented, mainly for external connections [14]. However, the internal connection has been widely used because of the stable self-locking interface and fewer mechanical complications [18,19], though it is not yet known if one connection is superior to another since the lack of comparative studies of overdentures retained with different number and connections of implant.
Many complications which are related to the excess load transmitted to the implant can occur and may be related to the number and location of implants in the arch. These complications suggest that excessive force is being dissipated in the bone surrounding the implant [7]. Clinically, this distribution of stress directly implies the choice of prosthetic planning [8,20]. Scientific researches have been conducted to introduce methods of assessing bone tissue behaviour in the surrounding region of implants [4-9]. Among them are the methodologies adopted in this study: photoelastic and strain gauge analysis. It is important to emphasize that several studies [21-24] showed that no type of analysis has complete preponderance over another (Finite Element, Stain Gauge, and Photoelastic analysis) have reported high failure rates mostly implant losses and prostheses fractures [23], resulting in a consensus among researchers that different analyses complement each other, and are used in association with their studies. Although single-implant retained overdentures are a promising alternative for edentulous patients, the limited research dedicated to this treatment concept has restricted its acceptance and implementation. Unfortunately, up-to-date published data on single-implant overdentures are scarce, and this treatment concept needs to be investigated thoroughly. Beyond this, there are no known studies that evaluated the biomechanics of implant-supported overdentures with a morse taper connection compared to those with external hexagon implants, and especially by means of association of two tension-analysis methods. The objective of this study was to use PA and SGA analysis to evaluate the biomechanics of overdentures supported by 1 or 2 implants with different types of connections (morse taper or external hexagon) submitted to different loading conditions {anterior (AR) and the posterior (PR) regions}. The hypotheses of this study are: 1) the morse taper systems will present smaller values of tension, independent of the number of implants; 2) the overdentures supported by two implants will have greater tension than overdentures supported by one implant.
Materials and Methods
This study was an in-vitro study, conducted over a period of one year, from July 2017 to July 2018, at the Department of Dental Materials and Prosthodontics of Aracatuba Dental School- Sao Paulo State University (UNESP). This study used 20 models of an atrophic jaw for Strain Gauge analysis and four models for Photoelastic analysis.
Division of Groups
The specimens were divided into four groups of one specimen each for photoelastic analysis and five specimens each for strain gauge analysis, according to the number of implants and type of connection as shown in [Table/Fig-1].
Divided four groups, according to the number of implants and type of connections.
| Groups | Connection system | Number of implants | Dimension | Attachments system |
|---|
| MT-S | Morse taper | 01 | 4×11 mm | O’ring |
| MT-T | Morse taper | 02 | 4×11 mm | O’ring |
| EH-S | External hexagon | 01 | 4×11 mm | O’ring |
| EH-T | External hexagon | 02 | 4×11 mm | O’ring |
MT-S: Morse taper single implant; MT-T: Morse taper two implants; EH-S: External hexagon single implant; EH-T: External hexagon two implants
Fabrication of Casts
Four specimens were fabricated of photoelastic resin (PL-2, Vishay, Micro-Measurements Group) and 20 specimens of polyurethane resin (F160 Axson Brazil). One overdenture was fabricated for each group.
Initially, a laboratory cast of one edentulous mandible was duplicated by using artisanal silicone (Sapeca Artesanato) to obtain a mould that was formed with Type IV dental stone (Durone, Dentsply Ind.,) for the fabrication of four stone casts [21,22]. Subsequently, the casts were perforated to receive dental implant analogues (DSP Biomedical) by using a parallelometer to standardise the insertion on its long axis. Implant analogues were screwed to the corresponding transfer (DSP Biomedical). The transfers in the MT-T and EH-T groups were united to each other by using bars of Duralay resin (Duralay Reliance Dental).
Artisanal silicone (Sapeca Artesanato) was again used to obtain an impression of the mould for the preparation of the photoelastic and polyurethane casts. After the silicone polymerisation, the transfer screw was unscrewed and removed to permit the plaster cast removal from the mould without moving the transfer position. Thus, the silicone matrix with the transfer already positioned was obtained, beginning with those which were adopted to the implants (DSP Biomedical) from each group, according to the specifications of each [Table/Fig-1] through the help of hemostatic forceps.
Initially, the silicone matrixes described above were used for the fabrication of five photoelastic models. For this, photoelastic resin (PL-2, Vishay, Micro-Measurements Group) was manipulated according to the manufacturer’s instructions and inserted into the silicone mould with the implants. The assembly was submitted to a 40 lbf/pol2 pressure to remove internal bubbles. The photoelastic cast was separated from the mould after polymerisation and polished with fine-grit abrasive paper of different granulations #300, #400, #600 and #1200 (Buehler).
Five specimens were fabricated for each group for the strain gauge analysis. The same silicon previously described was used, where the respective implants were positioned and later filled with the F160 polyurethane resin (F160 Axson Brazil).
Four overdenture prostheses were fabricated according to the number of implants. A conventional laboratory technique was used for their fabrication over the plaster moulds with the analogues in position. A colourless thermo-polymerisable resin was used (Vipi) to improve the observation of tension expressed by means of fringes during the photoelastic analysis. An O-ring retention system was used for the retention of the overdentures (DSP Biomedical).
The assembly was placed in mineral oil to minimise the refraction of white light and viewed with a circular polariscope for photoelastic analysis. Thereafter, 100 N axial loads were applied individually at fixed points on the occlusal surface of all crowns for 10 seconds with a universal testing machine (EMIC-DL 3000). Data were photographed (Rebel T5i, Canon) and transferred to a computer for qualitative analysis by using imaging software (Adobe Photoshop CS6; Adobe Systems). The Photoelastic analyses were classified according to the number of fringes and concentration of tension of each image. For the number of fringes analyses, it was verified fringes of moderate (green-red) and high tension (green-pink). For the concentration of tension analyses, the closer the fringes, the greater the tension. In order to facilitate the analysis of concentration of tension, the implant region was divided into three regions: cervical, middle and apical third [21,22]. All images were evaluated by the blinded corresponding author (AAP) and were analysed qualitatively.
For strain gauge analysis, two strain gauges were bonded in the region which corresponds to the mesial and distal bone crest of each implant. They were configured into a one-quarter Wheatstone bridge and the data were transferred through a data acquisition system (ASD 2000; Lynx Tecnologia Eletronica Ltd.,). The same load application used for the photoelasticity tests was repeated for the strain gauge test. Each test was performed five times and the stress values (microstrains) were recorded. The next tests were performed after the microstrain values were reset to verify the absence of plastic deformation.
Statistical Analysis
The three-way (factor 1: loading area; factor 2: number of implants; factor 3: connection system) analysis of variance (ANOVA) was used for the Strain Gauge Analyses, and the Bonferroni, as post-hoc test for multiple comparisons, was performed afterwards with a 5% level of significance (SPSS v. 20.0; SPSS Inc).
Results
Photoelastic Analysis
The same number of high-intensity (pink-green transition) and moderate (green/red) fringes was presented by single-implant supported overdentures (03), independent of the connection type in the posterior region. The greatest number of tension fringes was presented by the two-implant supported overdentures when compared with the one-implant supported overdentures, in both connection types, mainly in the posterior region [Table/Fig 2a-l,3].
Distribution of tension in photoelastic models of each groups evaluated. a) application of load in Morse taper single implant (MT-S) model-right molar region; b) application of load in Morse taper single implant (MT-S) model-incisors region; c) application of load in Morse taper single implant (MT-S) model-left molar region; d) application of charge in Morse taper two implants (MT-T) model-right molar region; e) application of load in Morse taper two implants (MT-T) model-incisors region; f) application of load in Morse taper two implants (MT-T) model-left molar region; g) application of charge in External hexagon single implant (EH-S) model-right molar region; h) application of load in External hexagon single implant (EH-S) model-incisors region; i) application of load in External hexagon single implant (EH-S) model-left molar region; j) application of charge in External hexagon two implants (EH-T) model-right molar region; k) application of load in External hexagon two implants (EH-T) model-incisors region; l) application of load in External hexagon two implants (EH-T) model-left molar region.

Number of tension fringes was presented by the two-implant supported overdentures when compared with the one-implant supported overdentures, in both connection types. (MT-Morse taper/EH-External hexagon)
| Groups | Number of Implants |
|---|
| One implant | Two implant |
|---|
| MT | 3 | 6 |
| EH | 3 | 5 |
Similar stress distribution patterns were shown in all casts according to the region of fringe concentration, regardless of the connection type. It was observed that the tension was concentrated at the apex of the implant. However, tension was also concentrated in the cervical region of the implant [Table/Fig-2a-l,3].
Strain Gauge Analysis
The three-way ANOVA analysis showed that all factors analysed (loading area, number of implants and connection system) were significant ([Table/Fig-4], p<0.0001). The average tension values (μ strains) (p<.0001), measured by using strain gauges for each type of connection system [Table/Fig-5], showed that values were influenced by the type of connection system and number of implants. There were higher tension values when the prosthesis was supported by two implants compared to those supported by a single implant (p<.0001).
Three-way repeated-measures ANOVA results for μ strain and all variable were significant (loading area, number of implants and connection system).
| Source | df | Type III Sum of squares | Mean square | F | p-value |
|---|
| Within-subjects effects |
| Loading area | 1 | 20600.252 | 20600.252 | 9847.698 | <0.0001* |
| Loading area×implant number | 1 | 1075.888 | 1075.888 | 514.315 | <0.0001* |
| Loading area×connection system | 1 | 374.238 | 374.238 | 178.900 | <0.0001* |
| Loading area×implant number×connection system | 1 | 34.615 | 34.615 | 16.547 | 0.001* |
| Error | 16 | 33.470 | 2.092 | | |
| Between-subjects effects |
| Implant number | 1 | 3933.281 | 3933.281 | 1709.221 | <0.0001* |
| Connection system | 1 | 341.933 | 341.933 | 148.588 | <0.0001* |
| Implant number×connection system | 1 | 193.028 | 193.028 | 83.881 | <0.0001* |
| Error | 16 | 36.819 | 2.031 | | |
*p<0.0001 denotes statistically significant difference
Mean values (standard deviation) of connection type and number of implants in implant-supported overdentures. Bars connected by whole lines show statistical difference between MT and EH within the same region of stress evaluation and same number of implants (p<0.0001). Dotted lines show a statistical difference between the 1 and 2 implants retained within the same region of stress evaluation and the same type of connection (p<0.0001).
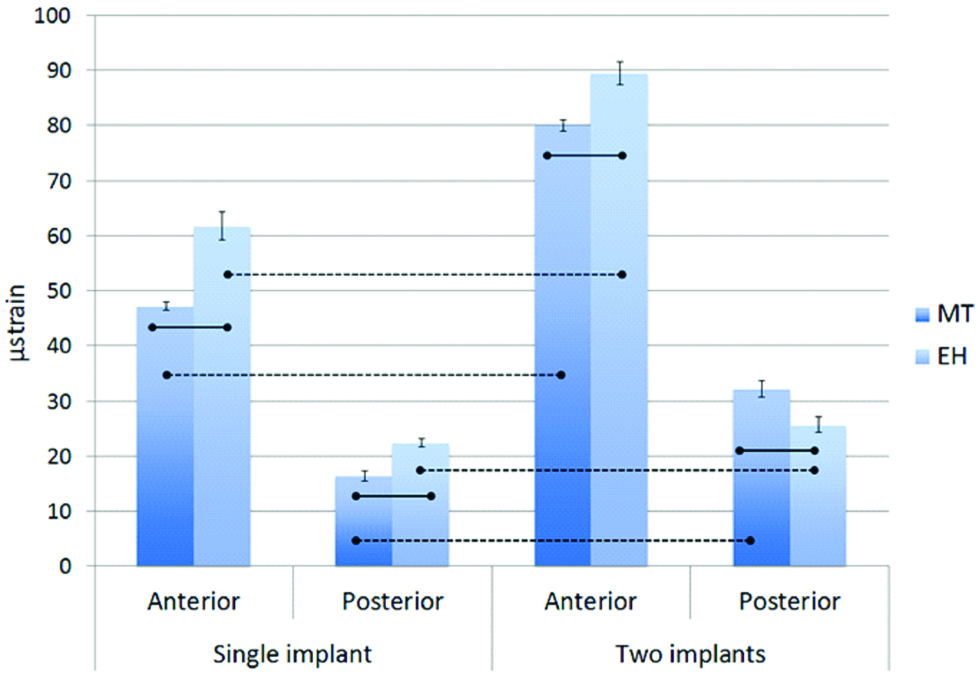
Smaller tension values were presented by single-implant supported overdentures under compression as compared to overdentures supported by two implants, equally for morse taper (p<0.0001) and external hexagon (p<0.0001) connections [Table/Fig-5].
A statistically significant difference (p<0.0001) was presented between the two connection systems for the single-implant supported overdentures. Lower tension values (26.72±0.60) were presented for the MT-S group and the greatest values (35.55±0.80) were presented by the EH-S group. Also, statistically significant difference was presented for the two-implant supported overdentures, independent of the connection system (p<0.0001).
Discussion
The first hypothesis was accepted because there was statistically significant difference between the connections of the two-implant supported overdentures for the strain gauge analysis, and between the single-implant supported overdentures for the photoelastic analysis. The second hypothesis was accepted because greater tension values were presented for the two-implant supported overdentures when compared with the single-implant overdentures in both analysis methods.
Some edentulous patients report problems during the use of their complete prosthesis, being the implant-supported mandible overdenture prosthesis an alternative for those patients. The principle advantages are the reduced number of implants required, facilitated surgical process, simple restoration technique, and efficient retention [1-8]. Beyond retention, it is also of vital importance for the longevity of the rehabilitation treatment with overdentures to not cause excessive loads on implants. For this, it is fundamental that the implant faces the minimum load possible since high strain gradients exceed the physiological limits of the bone when overloading occurs, causing much damage to the bone/implant/prosthesis system [7,8,20]. In addition, the selection of the number of implants and connection system are critical factors for the success of implant-retained overdentures. However, due to the scarcity of published literature concerning the effects of the number of implants and connection system on stress distribution in the upper structure of the overdenture, there is no reliable evidence demonstrating that a particular number of implants or connection system offers a better outcome as compared to another [5,8,10,25-29].
Clinically, it was expected that the tensions transmitted to the peri-implant bone would gradually decrease as the number of implants increased, due to the tension being more evenly distributed. This argument was based on the assumption that more implants to anchor and support, would distribute the tensions of the generated chewing force, thus decreasing bone deformation [8]. Nevertheless, this was not observed in the present study according to the results. Photoelastic analysis was used, and it was observed that all groups presented a similar number of high intensity fringes, regardless of the number of implants and connection system. Also, there were a higher number of fringes in two-implant supported groups when compared with the single-implant groups, in both types of connections [Table/Fig-3].
A statistically significant difference was verified between the number of implants (p<0.0001) by using strain gauge analysis; smaller tension values were presented in single-implant retained overdentures when compared with two-implant retained overdentures in both types of connection systems. This fact corroborates with other studies [4,5,8,30,31] which evaluated and compared stress distribution between single and two-implant retained overdentures for the rehabilitation of the edentulous mandible. A favourable concentration and distribution of tension was shown in the single-implant retained overdenture, while higher tension was produced in the two-implant retained overdenture. The lowest tension values were encountered in the single-implant retained overdentures, explained by the fact that masticatory stress distribution in a single-implant overdenture uses full mucosal support and develops a more favourable stress tension distribution in the horizontal dimension. This may limit the problems encountered with the standard mandibular overdenture approach [31]. In addition, a single-implant design is less conducive to rotational forces, as it permits more even distribution of occlusal forces [12].
Nascimento JFM et al., observed that an overdenture with an implant presented better distribution of tension in the peri-implant tissue, with the load being transferred mostly in the mucosal tissue that supports the prosthesis [5]. These features approximate the overdenture-type prosthesis with one implant with the conventional-type prosthesis with respect to biomechanical features, with the advantage of having an implant to improve retention.
However, increasing the number of implants shifted the support from the mucosal surfaces to the implants [9,32]. Also, the denture base of a two-implant mandibular overdenture tends to have a rotational movement around the fulcrum line between the two implants, and a considerable bending motion may be transferred to the implants by the attachments [5,30]. Another advantage of the single-implant is its installation in the anterior region of the mandible, which is preferred due to thicker cortical bone and lowered surgical risk by avoiding the inferior alveolar nerve and blood vessels. In addition, there is a larger tissue-supporting region to prevent overloading on the implant. However, there was some concern regarding the potential risk of mandibular fracture because of the anatomical structure [2].
On the other hand, Maeda Y et al., observed that there was no difference between the tension generated in single-implant overdentures and two-implant overdentures applying loads in different regions of the prosthesis [25]. Liu J et al., performed in-vitro studies in which they founded a displacement of the overdenture-type prosthesis with an implant when submitted to vertical loading in the anterior region [8]. However, there were no significant changes in tension in the peri-implant region yet, according to the authors, single-implant overdenture use does not lead to tension concentrations beyond the physiological limits in the bone around the implant, and could be a feasible choice for edentulous patients.
Published clinical studies [1,2,8,12,15,33] observed that the bone around the implant was within the acceptable physiological limits, noting that there was no significant difference in bone resorption around the implant when compared to overdentures with one and two implants, thus the number of implants has little influence on the longevity of the prosthesis with regard to bone absorption. Due to the advantages presented by the treatment with a single-implant overdenture, it has become a successful and beneficial treatment option for adults with a high degree of bone resorption. Furthermore, they demonstrated that the single-implant supported overdenture increased retention and stability compared with the conventional complete overdenture and that the biomechanical effects were comparable to those observed in a mandibular two-implant retained overdenture.
Also, various published studies [12,18,19,34-37] emphasise the mechanical advantages of the morse taper connection system in relation to the external hexagon, such as higher resistance and stability, a smaller micro gap and bone loss, greater mechanical friction, fewer mechanical complications, and more evenly distributed tension.
In the present study, biomechanical superiority of the morse taper system in relation to the external hexagon was only seen in the single-implant retained overdenture. There was statistically significant difference in the two-implant retained overdentures between the two connected systems. Based on this, despite the advantages of the internal connections in unitary prostheses, there is some doubt in the biomechanical behaviour when using multiple prostheses. Some authors reported higher tensions surrounding the implant connections than when using the external hexagon, and the indication of multiple implants attached with an external hexagon remains [12,37]. It is possible that when the union of the implant with an internal connection is performed, the internal geometric figures of the implant make the correct installation, an aspect of fundamental importance for the success of the rehabilitation. However, a minimal lack of parallelism can influence the concentration of tension caused by the connection system. In addition, the external-hexagon implant platform keeps the abutment in a certain occluso gingival position, and the internal cone, which has no horizontal platform, may allow axial displacement of the abutment [38].
There is no doubt that dental implants can enhance the support, stability, and retention of complete removable dentures. This leads to increased patient comfort, improved chewing ability, and greater acceptance of the prosthesis [1]. Although a single implant is generally less retentive than the two-implant overdenture, patient satisfaction in clinical studies is greatly improved by increasing retention using a single implant with the additional advantages of lower costs and simpler clinical procedures [5].
Single-implant mandibular overdentures may be suggested as an alternative treatment modality for the rehabilitation of edentulous patients who cannot afford the cost of a two-implant overdenture. Thus, it is not possible to judge which form of treatment is better for an edentulous mandible, since it depends on a clinical evaluation by a trained prosthodontist and a well-informed patient to select the best treatment, meeting the expectations of the patient within the limitations of each treatment.
Limitation
Study with larger specimen size in each individual group should be conducted for future prospective.
Conclusion
Within the limits of this study, it was concluded that the number of implants influenced the tension distribution in mandibular overdentures, being greater in two-implant retained overdentures. Also, the connection system was found to have a significant effect on tension values only for the single-implant retained overdentures, with the morse taper system generating lower tension. In addition, biomechanically, the single-implant mandibular overdentures may be suggested as an alternative treatment modality for the rehabilitation of edentulous patients, principally when being used with the morse taper system.
Funding: This work was supported by the Pro-Rectory of Research of Paulista State University “Júlio Mesquita”. Prope-Unesp [protocol: 735].