Introduction
The nursing principles and skills training are considered to be the cornerstone of clinical education. Since traditional training techniques leads to lack of practical learning of students, the use of new educational methods seems to be necessary.
Aim
To compare the effects of video assisted and supervised group training on nursing students’ clinical skills.
Materials and Methods
The present quasi-experimental study was conducted in 2016 on 56 students of the Iranshahr University of Medical Sciences who were randomly assigned to two groups of control and intervention. The data were collected using a clinical skills checklist. The intervention was performed in 12 sessions for both groups. Participants in the video preparation group collectively produced a video about the correct implementation of a skill and received feedback from their instructor. Those in the group training practised the same skill supervised by the instructor. At the end of the intervention, the participants took the Objective Structured Clinical Evaluation (OSCE). Data were then analysed by using independent t-test in SPSS, version 16.0.
Results
A significant difference (p<0.05) was observed in the mean total score of clinical skills in the intervention group (17.0±0.4) and the control group (15.8±0.7).
Conclusion
In the “Principles and Skills” course, video preparation group training can be employed to increase the nursing students’ practical learning.
Introduction
Clinical skills are a series of practices aiming at expanding the competence indispensable for appropriate professional practice. These skills are any observable and discrete acts in the patient care procedure. The clinical nursing skills for nurses are extremely important not only to promote clinical competency but also to offer comprehensive care [1].
The basic clinical and practical skills training is a challenging part of nursing education, accounting for 50% of the nursing education program to train competent and qualified nurses with sufficient attitude, knowledge, and skills in order to promote and maintain the community health [2].
Given the complexity of nursing knowledge together with technological advancement, applying meaningful and effective learning methods seems essential and nursing education, to keep up with the growing trend, must cross the boundaries of time, space and move towards innovation, development and use of new teaching approaches. Applying new teaching strategies leads to deeper learning and the use of metacognitive skills leads to the development of critical thinking [3]. One of these new approaches is Collaborative Learning (CL), in which learners work at different executive levels in small groups in order to achieve a common goal. Patient care can also be part of CL [4].
The findings of Kanthan R and Mills S, showed that CL improves the individual and professional skills of medical students [5]. Bunger AC et al., found out that CL enhances the interaction between patients and students and also between studious and weak students [6]. Critical thinking and problem-based learning is associated with lifelong learning [7]. Findings of the study by Klein CJ and Fowles ER, and Baumberger-Henry M, showed that the use of participatory approach improves critical thinking and clinical care skills [8,9].
Hoke MM and Robbins LK, concluded in their study that the clinical score of students in the participatory approach was higher than the lecture approach [10].
In Iran, the use of smartphone and smart learning has considerably increased. By utilising a video recording of nurses’ progress in basic nursing performance via a smartphone for learning, their progress of skill practice can be objectively monitored; therefore, immediate feedback is possible. This can be an effective and interesting way of learning [11].
Jeong H, conducted a study in Korea to investigate the effect of video practice development. In the mentioned study, the nursing students were regarded as a single experimental group. The results showed that the smartphone video recording practice method applied to nursing students significantly and positively promoted learning satisfaction and fundamental nursing practice competency [11]. Lee SG and Shin YH, in their study demonstrated that self-directed feedback practice utilising smartphone videos could promote basic nursing skills [12].
Few studies have been conducted on smart learning targeting nursing students. Thus, it is indispensable to examine the intervention effect of pure smart learning with a control group on the basis of various variables. Furthermore, nursing students still experience the training process, and their basic nursing competency is still undeveloped. Through watching videos, the instructor is able to appropriately assess the students’ performance levels during the practice and the learners are able to assess themselves. In this regard, a repeated learning effect will occur even after completing the practice in the case where the students are instructed to study by watching their recorded videos.
It is assumed that nursing students can apply the knowledge of clinical care after learning in practice laboratory. Studies have shown that such training in apprenticeship, due to the use of traditional methods rarely leads to the development of decision-making power, attitude and education. In other words, traditional teaching methods in practice labs do not provide an adequate level of practical learning for students to use in clinical settings [13,14]. Considering the importance of “Clinical Principles and Skills Course” for nursing students and the effectiveness of CL methods, the present study aimed to determine and compare the effects of supervised group training and video preparation group training on clinical skills of nursing students.
Materials and Methods
Study Design
The present research was a quasi-experimental study that was conducted on 56 undergraduate students of Nursing, Anaesthesiology, and Operating Room of Iranshahr University of Medical Sciences from September 2016 to January 2017. The participants were selected based on complete enumeration. The inclusion criteria were being a freshman of Iranshahr University of Medical Sciences and taking “Clinical Principles and Skills Course” and the only exclusion criterion was the absence in more than two sessions of the practical course.
Sample and Recruitment
With a confidence level of 95% and a statistical power of 90%, the sample size was calculated according to the following formula:
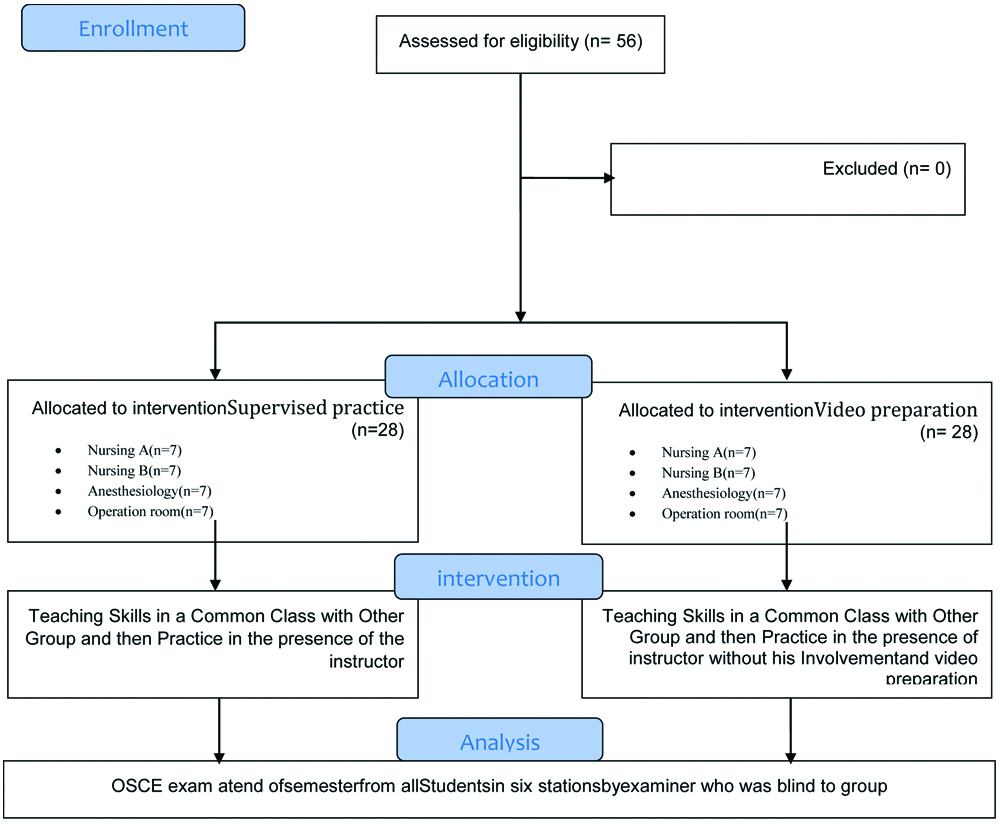
In each group, 20 individuals were estimated. A total of 56 subjects (28 nursing students, 14 anaesthesiology students, and 14 operating room students) were determined to increase the study validity and to achieve more generalisability. The sample size was calculated equal in all groups, since it was a pilot study. The samples were selected from among the first and second semester students. No sample was excluded during the study [Table/Fig-1].
Consort diagram of methodology
Instruments
The data collection tools included a demographic form and a clinical skills checklist. Developed based on the research objectives and review of the latest articles, the demographic form consisted of eight items about individual and educational information. The clinical skills checklist included the control of vital signs including the measurement of pulse (nine items), respiratory rate (six items), body temperature (six items), and blood pressure (14 items) as well as wound dressing (17 items), gastric intubation (19 items), urinary catheterisation (28 items), intravenous catheterisation (20 items), and oxygen therapy and suction (24 items). In this checklist, a score of zero, one, and two is given to choices “Not done”, “Incompletely done”, and “Correctly done”, respectively [15]. The approach proposed by Lawshe was used to quantitatively determine the content validity. To this end, Content Validity Ratio (CVR) and Content Validity Index (CVI) were calculated. The clinical skills checklist was given to 10 lecturers of Nursing and Midwifery Faculty of Iranshahr University of Medical Sciences and they were asked to evaluate each item by choosing one of the following choices: “Necessary”, “Useful but not necessary”, and “Not necessary”. The CVI was obtained by calculating the mean CVR of all items. All 10 lecturers selected the choice “Necessary” for all items of the checklist and the CVR was equal to 1 for all of the items. As a result, the CVI, as the mean CVR, was obtained equal to 1. The reliability of this checklist was assessed using the inter-rater agreement. Accordingly, clinical skills of 10 students were evaluated in Clinical Skills Centre of the studied university. Pearson correlation coefficient was obtained 0.87 for vital signs measurement, 0.92 for wound dressing, 0.94 for gastric intubation, 0.96 for urinary catheterisation, 0.92 for intravenous catheterisation, and 0.89 for oxygen therapy and suction.
Procedure
The participants were equally divided into two groups of video preparation group training and supervised group training (28 students in each group). In order to provide similar skills training to the participants, one subgroup from the supervised group training and one subgroup from the video preparation group training formed a larger group, by drawing, to attend the practice lab for skill training and practice session at the same time. The six main nursing skills selected for training in this study included measurement of vital signs, wound dressing, oxygen therapy and suction, gastric intubation, urinary catheterisation, and intravenous catheterisation. The intervention was performed in 12 sessions and each sessions was of 90-minutes for each large group twice a week (one training session and one practice session). The intervention sessions were held in Clinical Skills Centre of Iranshahr University of Medical Sciences. The training session for each skill was attended by a subgroup of supervised training and a subgroup of video preparation. In these sessions, the desired skill was explained and practically performed on a moulage by the instructor and also the necessary tips were specified in detail. At the end of each session, participants of both groups were asked to complete the checklist of that skill. One week later, the same skill was simultaneously practised by the same groups in two separate rooms. Participants in the video preparation group collectively practised the skill and the instructor guided them whenever necessary. Then, they filmed the correct implementation of the skill by one of the participants using their mobile phone camera (in the presence of the instructor) and submitted the video to their instructor. The instructor reviewed the video in the presence of the participants and provided them with the necessary feedback. Participants in the group training also practised the skill supervised by the instructor. In the end, one of the participants performed the skill in the presence of the instructor and received feedback.
After training and practice of all skills, at the end of the semester, the participants took the Objective Structured Clinical Evaluation (OSCE), including six stations for the above-mentioned skills. At each station, an examiner (one of the instructors of Nursing and Midwifery Faculty. who was blind to the group and was not part of the research team and) assessed the participants based on the related skill checklist.
The Ethics Committee affiliated with Iranshahr University of Medical Sciences approved the conductance of this study as well as the consent procedure (Medical Ethic No: IR.IRSHUMS.REC.1394.12). Then verbal agreement of the participants was obtained, and they were ensured in terms of confidentiality and anonymity of the data as well as voluntary participation in the study. Informed consent was implied from returning the completed questionnaires.
Statistical Analysis
The statistical analysis was done using SPSS version 16.0. The mean and standard deviation were calculated for quantitative data and independent t-test was used to compare the two groups in terms of the pre- and post-intervention scores on the clinical skills. The confidence interval and the significance level were determined to be 95% and 0.05, respectively.
Results
Study Participants’ Characteristics
The participants were aged 18-21 years with a mean of 18.9±0.8 years. In terms of gender, 10 (35.7%) of the participants in the supervised training group and 15 (53.6%) in the video preparation group were male. Most of the participants (17) (60.7%) in the supervised training group and 23 (82.1%) in the video preparation group) were residing in a dormitory. In terms of major, 26, 16, and 14 participants were studying Nursing, Anaesthesiology, and Operating Room, respectively. In addition, 27 (96.4%) participants in the supervised training group and 26 (92.9%) in the video preparation group were married. Regarding the background variables, the results indicated no significant difference between the two groups [Table/Fig-2].
Comparison of the demographic variables between the two groups of video preparation and supervised practice.
| Variable | Group | p-value |
|---|
| Supervised practice | Video preparation |
|---|
| Number (%) | Number (%) |
|---|
| Gender | Male | 10 (35.7) | 15 (53.6) | *p=0.179 |
| Female | 18 (64.3) | 13 (46.4) |
| Age (Mean±SD) | | 18.0±8.8 | 19.0±9.0 | **p=0.521 |
| Marital status | Single | 27 (96.4) | 26 (96.9) | ***p=0.553 |
| Married | 1 (3.6) | 2 (7.1) |
| Residence | Dormitory | 17 (60.7) | 23 (82.1) | ***p=0.553 |
| Native | 11 (39.3) | 5 (17.9) |
| Discipline | Nursing | 13 (46.4) | 13 (46.4) | *1.000 |
| Operating room | 8 (28.6) | 8 (28.6) |
| Anaesthesiology | 7 (25.0) | 7 (25.0) |
SD: Standard deviation; *Chi-square; **Independent t-test; ***Fischer’s-exact
Comparison of the Clinical Skills between Video Preparation and Supervised Practice Groups
The mean total score of clinical skills was 15.8±0.7 in the supervised training group and 17.0±0.4 in the video preparation group. The independent t-test showed a significant difference between the two groups in this regard, as the mean total score in the video preparation group was significantly higher than the training group (p≤0.001) [Table/Fig-3].
Comparison of the clinical skills post test mean scores between the two groups of video preparation and supervised practice.
| Variable | Group | Independent t-test (p-value) |
|---|
| Supervised practice | Video preparation |
|---|
| Mean±SD | Mean±SD |
|---|
| Vital signs | 16.5±1.1 | 17.2±1.0 | 0.019 |
| Gastric intubation | 15.8±1.3 | 16.8±0.9 | 0.002 |
| Dressing | 15.4±1.1 | 17.1±1.0 | ≤0.001 |
| Urinary catheterisation | 15.5±1.0 | 16.8±0.7 | ≤0.001 |
| Oxygen therapy and suction | 15.9±0.9 | 17.1±0.8 | ≤0.001 |
| Intravenous catheterisation | 15.5±1.0 | 17.0±0.7 | ≤0.001 |
| Total score | 15.8±0.7 | 17.0±0.4 | ≤0.001 |
SD: Standard deviation
As shown in [Table/Fig-3], the mean score of participants in the video preparation group in all studied clinical skills presented an increase compared to that of the training group. This increase was equal to 0.7 in measurement of vital signs, 1.7 in wound dressing, 1 in gastric intubation, 1.2 in oxygen therapy and suction, 1.3 in urinary catheterisation, and 1.5 in intravenous catheterisation. The results of the independent t-test indicated a significant difference between the two groups in the mean score of all clinical skills. In addition, analysis of covariance demonstrated that there was no significant difference between the two groups in terms of the mean score of all clinical skills considering the background variables.
Discussion
The findings of the present study showed that the mean score of clinical skills in the video preparation group was significantly higher than that of the supervised training group. This indicates the positive impact of video preparation group training on the clinical skills of nursing students. Due to the innovative nature of this technique, there was no similar study to investigate its effects on the clinical skills of students. Therefore, the findings were compared to studies that used other CL methods.
The results of Hoke MM and Robbins LK, showed that CL in small groups increases the clinical skills of nursing students in caring for cardiovascular patients [10], which is consistent with the findings of the present study. As an explanation of this finding, it can be stated that since students who were under CL could collaborate with members of their group and they presented with higher self-motivation and desire for learning.
In a study conducted by Bambini D et al., on 112 nursing students, it was found that CL can significantly increase students’ self-efficacy in performing postpartum and newborn care [16]. This is consistent with the findings of the present study.
The results of the present study are also consistent with the previous findings who concluded that practice-based learning in small groups increases the knowledge and skills of nursing students and improve the quality of patient care [17-20].
The findings of Mahram M et al., Dusold R and Sadoski M, and Fischer RL et al., demonst rate that there was no significant difference between traditional methods and student-centered methods [21-23], which is not consistent with the findings of the present study.
Although active learning methods are an effective educational intervention for medical students, teacher-centered methods dominate the educational system and student-centered methods, such as problem-solving, group discussion, and peer learning, are not as familiar to teachers and they need mental readiness to adopt such methods. The similarity of the reliability results can be attributed to students’ attempt to learn and master the content taught in both methods in order to obtain a good mark. Roseth CJ et al., also found that CL does not always outdo other learning approaches in learning level development, it creates a great sense of success in students and positive outcomes in their learning styles that make for lifelong learning [24].
Limitation
Sampling from only one faculty reducing the generalisability of findings, small sample size, and impossibility of measuring long-term learning were the main limitations of the current study.
Conclusion
The present study findings indicate the effect of group video training on promoting students’ practical learning. The findings can be employed to teach the principles and clinical skills of nursing faculties. It also suggested that future studies should be conducted with a larger sample size in other departments and in different practical courses and longer follow-up periods by employing this method of teaching.
The study findings also demonstrate the effectiveness of CL in promoting nursing students’ practical learning in the “Principles and Skills” course. Accordingly, the use of active educational methods is recommended to broaden the students’ participation in the training process and promote their learning level.
[1]. Papathanasiou IV, Kleisiaris CF, Fradelos EC, Kakou K, Kourkouta L, Critical thinking: the development of an essential skill for nursing studentsActa Inform Med 2014 22(4):283-86.10.5455/aim.2014.22.283-28625395733 [Google Scholar] [CrossRef] [PubMed]
[2]. James A, Chapman Y, Preceptors and patients- the power of two: Nursing student experiences on their first acute clinical placementContemporary Nurse 2010 34(1):34-47.10.5172/conu.2009.34.1.034 [Google Scholar] [CrossRef]
[3]. Sadeghi H, Shahbazi S, Naseri Borujeni N, Pooiesh V, Comparison of the effects of concept mapping and conventional teaching methods on critical thinking of nursing studentsJournal of Nursing Education 2016 5(4):27-33.10.21859/jne-05044 [Google Scholar] [CrossRef]
[4]. Vafadar Z, Vanaki Z, Ebadi A, An overview of the most prominent applied models of inter-professional education in health sciences in the worldResearch in Medical Education 2017 8(4):69-80.10.18869/acadpub.rme.8.4.69 [Google Scholar] [CrossRef]
[5]. Kanthan R, Mills S, Cooperative learning in the first year of undergraduate medical educationWorld J Surg Oncol 2007 5(1):13610.1186/1477-7819-5-13618045477 [Google Scholar] [CrossRef] [PubMed]
[6]. Bunger AC, Doogan NJ, Hanson RF, Supporting implementation through collaborative learning: facilitating access to clinical expertiseImplement Sci 2015 Springer10.1186/1748-5908-10-S1-A25PMC4551839 [Google Scholar] [CrossRef] [PubMed]
[7]. Davis L, Taylor H, Reyes H, Lifelong learning in nursing: a Delphi studyNurse Educ Today 2014 34(3):441-45.10.1016/j.nedt.2013.04.01423664106 [Google Scholar] [CrossRef] [PubMed]
[8]. Klein CJ, Fowles ER, An investigation of nursing competence and the competency outcomes performance assessment curricular approach: senior students’ self-reported perceptionsJ Prof Nurs 2009 25(2):109-21.10.1016/j.profnurs.2008.08.00619306834 [Google Scholar] [CrossRef] [PubMed]
[9]. Baumberger-Henry M, Cooperative learning and case study: does the combination improve students’ perception of problem-solving and decision making skills?Nurse Educ Today 2005 25(3):238-46.10.1016/j.nedt.2005.01.01015795027 [Google Scholar] [CrossRef] [PubMed]
[10]. Hoke MM, Robbins LK, The impact of active learning on nursing students’ clinical successJ Holist Nurs 2005 23(3):348-55.10.1177/089801010527764816049122 [Google Scholar] [CrossRef] [PubMed]
[11]. Jeong H, Effects of nursing students’ practices using smartphone videos on fundamental nursing skills, self-efficacy, and learning satisfaction in South KoreaEurasia Journal of Mathematics, Science & Technology Education 2017 13(6):2351-65.10.12973/eurasia.2017.01229a [Google Scholar] [CrossRef]
[12]. Lee SG, Shin YH, Effects of self-directed feedback practice using smartphone videos on basic nursing skills, confidence in performance and learning satisfactionJ Korean Acad Nurs 2016 46(2):283-92.10.4040/jkan.2016.46.2.28327182024 [Google Scholar] [CrossRef] [PubMed]
[13]. Şenyuva E, Çalışkan F, Lifelong learning perception metaphoric of nursesProcedia-Social and Behavioral Sciences 2014 152(0):372-78.10.1016/j.sbspro.2014.09.214 [Google Scholar] [CrossRef]
[14]. Svejda M, Goldberg J, Belden M, Potempa K, Calarco M, Building the clinical bridge to advance education, research, and practice excellenceNursing Research and Practice 2012 2012:82606110.1155/2012/82606122548162 [Google Scholar] [CrossRef] [PubMed]
[15]. Potter PA, Perry AG, Stockert P, Hall A, Fundamentals of Nursing-E-Book 2016 Elsevier Health Sciences [Google Scholar]
[16]. Bambini D, Washburn J, Perkins R, Outcomes of clinical simulation for novice nursing students: Communication, confidence, clinical judgmentNurs Educ Perspect 2009 30(2):79-82. [Google Scholar]
[17]. Sommers LS, Morgan L, Johnson L, Yatabe K, Practice inquiry: clinicaluncertainty as a focus for small-group learning and practice improvementJ Gen Intern Med 2007 22(2):246-52.10.1007/s11606-006-0059-217356994 [Google Scholar] [CrossRef] [PubMed]
[18]. Armson H, Kinzie S, Hawes D, Roder S, Wakefield J, Elmslie T, Translating learning into practice. Lessons from the practice-based small group learning programCan Fam Physician 2007 53(9):1477-85. [Google Scholar]
[19]. Murrihy RC, Byrne MK, Gonsalvenz CJ, Testing an empirically derived mental health training model featuring small groups, distributed practice and patient discussionMed Educ 2009 43(2):140-45.10.1111/j.1365-2923.2008.03256.x19161484 [Google Scholar] [CrossRef] [PubMed]
[20]. Kanisin-Overton G, Mccalister P, Kelly D, Macvicar R, The Practice based Small Group Learning Programme: experiences of learners in multiprofessional groupsJ Interprof Care 2009 23(3):262-72.10.1080/1356182080269762819415563 [Google Scholar] [CrossRef] [PubMed]
[21]. Mahram M, Mahram B, Mousavinasab SN, Comparison between the effect of teaching through student-based group discussion and lecture on learning in medical studentsStrides in Development of Medical Education 2009 5(2):71-79. [Google Scholar]
[22]. Dusold R, Sadoski M, Self-directed learning versus lecture in medicineAcademic Exchange Quarterly 2006 10(4):29 [Google Scholar]
[23]. Fischer RL, Jacobs SL, Herbert WN, Small-group discussion versus lecture format for third-year students in obstetrics and gynecologyObstet & Gynecol 2004 104(2):349-53.10.1097/01.AOG.0000133485.02727.ba15292010 [Google Scholar] [CrossRef] [PubMed]
[24]. Roseth CJ, Johnson DW, Johnson RT, Promoting early adolescents’ achievement and peer relationships: The effects of cooperative, competitive, and individualistic goal structuresPsychological Bulletin 2008 134(2):223-24.10.1037/0033-2909.134.2.22318298270 [Google Scholar] [CrossRef] [PubMed]