Osteoma is a benign, exophytic neoplasm composed of osteoids and bone tissue of uncertain origin. It can occur in any bone, but is more common in the bones of face and paranasal sinuses. Its involvement with the orbital cavity is rare. When this occurs, the lesion usually arises from the paranasal sinuses with extension to the orbit. This paper presents the case of a patient with a supraorbital border osteoma without the involvement of any sinus of the face. A 34-year-old patient sought care due to a volumetric increase and aesthetic defect in the supraorbital region. Information from anamnesis, clinical examination and imaging tests led to the diagnostic hypothesis of osteoma. Surgical excision of the lesion and reconstruction of the defect on the right supraorbital border with titanium mesh was performed. Histological analysis confirmed the initial hypothesis. Although rare, the primary involvement of the osteoma with the orbital cavity was evidenced. Reconstruction of the bone defect caused by the excision of the lesion with titanium mesh proved to be a satisfactory therapeutic option to restore the anatomical contour of the patient.
Case Report
A 34-year-old female patient was referred to the Department of Dentistry of a philanthropic hospital in Cuiabá, Mato Grosso. The patient complained of “a growth in the bone above the right eye” since 2 years. Medical history was not significant. At anamnesis, she did not report any vision changes, ocular pain, pain with eye movement, or headache, or the use of any medication.
On physical evaluation, a volumetric increase was observed in the right supraorbital border, causing palpebral ptosis and aesthetic defect [Table/Fig-1]. Ocular motor and visual acuity were within normal ranges.
Volumetric increase in right supraorbital border.

Computed tomography showed a volumetric increase in the right supraorbital border region resembling the proliferation of bone tissue, measuring 25×25×10 mm. Scintigraphy showed hypercaptation at the right supraorbital area, indicating metabolic activity in the region [Table/Fig-2].
Red arrows show (a, c and d) tissue proliferation in the right supraorbital border and (b) hypercaptation area in the region of the right supraorbital border.

From the complementary examinations, the diagnostic hypotheses of osteoma, ossifying fibroma and osteoblastoma were made. Preoperative examinations were performed with the objective of excision of the lesion and reconstruction of the supraorbital border.
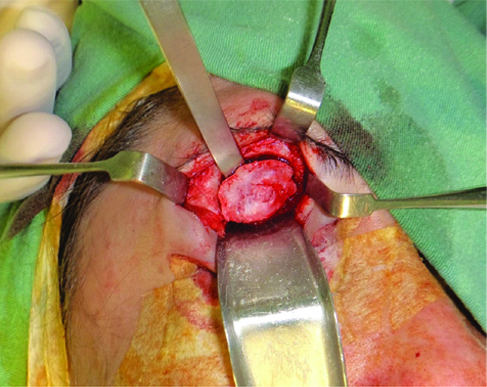
Surgery was performed under general anaesthesia. The chosen access was superciliar, with incision and periosteal detachment. After total exposure and good visualisation [Table/Fig-3], a drill osteotomy was performed surrounding the entire lesion. With a straight chisel and hammer, the lesion was detached. Peripheral osteotomy was performed with a spherical multi-laminate drill to eliminate any lesion residues [Table/Fig-4].
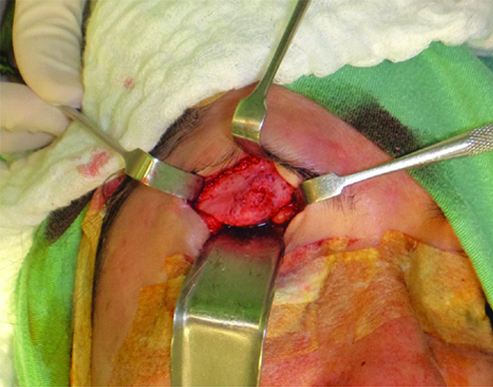
Osteotomy and detachment using a 6 mm chisel.
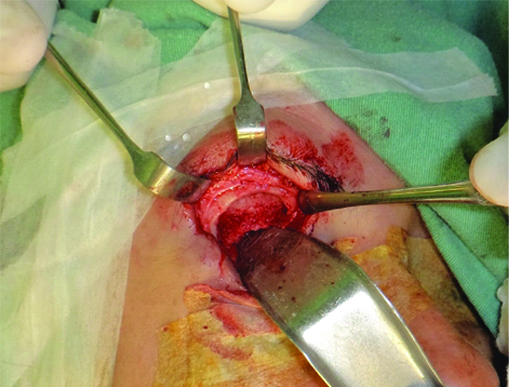
As the bone defect could cause an aesthetic defect even worse than the lesion [Table/Fig-5], it was planned to reconstruct the upper edge of the orbit with titanium mesh of the 1.5 system and equivalent screws (MDT-Víncula, Rio Claro, Brazil) [Table/Fig-6].
Bone defect after surgical excision.
Titanium mesh being positioned and fixed.
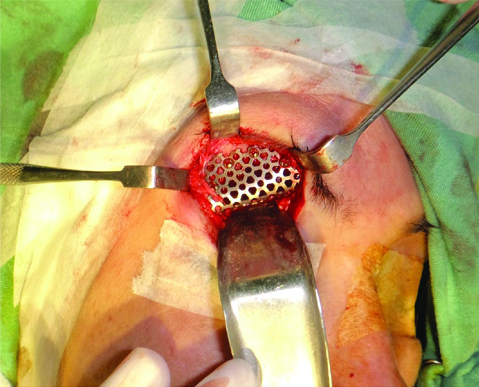
After stabilisation and fixation of the titanium mesh, its stability was verified with a detacher tip and the muscles showed to be free of incarceration. Abundant irrigation with 0.9% saline solution was performed and suturing by planes with vicryl 4-0 for internal suture and nylon 5-0 for intradermal suture was performed. A compressive dressing was made on the operated area with gauze and micropore.
Histological sections revealed a fragment of dense, compact, and lamellar bone tissue with deposition lines and gaps with osteocytes dispersed in the bone matrix. The histology along with the clinical data led to the diagnosis of osteoma [Table/Fig-7].
Histological section reveals a fragment of dense, compact, and lamellar bone tissue with deposition lines and gaps with osteocytes dispersed in the bone matrix HE 40X.

As the condition of the patient improved, she was discharged on the next day. She was followed-up regularly, and it was observed that ocular globe motility and visual acuity were preserved. The patient reported a loss of sensitivity in the right supraorbital region, which was expected due to the damage of the supraorbital nerve, involved in the lesion. The tomographic image obtained at 7 months postoperatively, showed good positioning of the titanium mesh, mimicking the contour of the supraorbital border [Table/Fig-8]. The result was considered satisfactory. The case currently has an 18 month follow-up period [Table/Fig-9].
Seven months post-operative computed tomography showing good positioning of the titanium mesh and absence of recurrence.

Clinical image at 18 months follow-up.

Discussion
This paper described the case of a patient with osteoma in the right supraorbital border involving palpebral ptosis, and aesthetic defect, as well as its treatment.
Osteomas are benign skeletal neoplasms, composed of bone and osteoid tissue [1], which develop at the expense of facial bones and paranasal sinuses [2] in approximately two-thirds of cases [3]; they mostly affect men [4] between the fourth and fifth decade of life [1,5]. The most frequent sites of origin in the skull and face are the frontal sinus (71.8% of the cases), ethmoid sinus (16.9%), maxillary sinus (6.3%) and sphenoid sinus (4.9%) [2]. Its occurrence in the orbit is particularly rare, and corresponds to 0.9 to 5.1% of all orbital tumours [3]. When present at the orbit, the osteoma is usually an invasion of the lesion from the paranasal sinuses [2], which also occurs rarely [6]. The reported case shows the rare condition of a 34-year-old woman with osteoma in the supraorbital border.
The growth rate of osteomas is very slow, from 12 to 30 years according to reported series, and they are often detected in imaging tests requested for another reason [7]. In the present case, the lesion had an evolution of two years. The location of the lesion, with aesthetic alterations favoured its diagnosis in a shorter time.
Tumour growth in the orbit may cause displacement of the globe with gradual proptosis and diplopia, with eventual restriction of the globe’s motion [2]. In the present case, the patient presented with palpebral ptosis.
Radiographically, osteoma is a bone-forming radiopaque lesion [6]. It frequently appears as dense, lobulated, well-defined sclerotic masses that form a polypoid configuration [2,3,6,8], as observed in the tomography images for this case.
No cause of lesion development was found in this case. Theories that explain the formation of an osteoma have been raised, such as infection, trauma and genetic factors, but without much scientific support to date [1].
The diagnosis of osteoma is clinical, radiographic and histopathological. Histologically it is composed of mature bone tissue, which is characterised by the arrangement of the collagen fibers in the same direction and the osteocytes within their gaps reveals the viability of that tissue [9], as normal osseous tissue [10,11]. The presence of mature bone and osteoid cells, as well as the absence of multicellular tissue with loose connective tissue, discarded the diagnosis of fibro-osseous lesions, while the absence of cellular pleomorphism and cells in division phases ruled out the diagnosis of malignant neoplasia [9].
Complete excision of the osteoma is the treatment of choice [3] with endoscopic or external surgical interventions [3,12]. The selection of surgical technique depends on the size and localisation of the osteoma, the experience of the surgeon [3,12] and the excision technique [3]. Other options are recently developed methods, such as percutaneous CT-guided drill ablation or thermo-coagulation with a laser; however, they require specialised surgical equipment and are expensive [13]. Partial resection has also been described as an alternative when complete resection is at risk of excessive morbidity or unnecessary surgical complexity [8]. However, in cases of incomplete excision, relapse may occur after 2 to 8 years [7]. In the present case, the complete resection of the osteoma was chosen due to the lesion’s activity indications given by the patient’s report regarding its progressive development and the hypercapting images in the supraorbital border region seen in the scintigraphy and the lower potential of recurrence [7].
Surgical approach must minimise any damage to adjacent structures, obtaining the maximum aesthetic result by the appropriate planning of incisions for surgical access [3]. For osteoma in the facial region, resection with an endoscopic holmium-doped yttrium aluminium garnet laser with a long flexible fibre is a good treatment option, as it does not leave a scar, is minimally invasive, and causes less post-operative pain [14]. The option in this case for the external surgical approach took into account due to the inexistence of the endoscopic laser in our hospital and the necessity of reconstruction of the supraorbital border with the titanium mesh fixation. It proved to be good, as it facilitated the adaption of the mesh to the contour of the orbit, allowing the patient to regain her anatomy and function. Restoration of the orbit in its pre-operative volume and anatomy is one of the most difficult surgical tasks. The restoration of the pre-operative anatomy and the volume of the internal orbit is the most important component of orbital reconstruction [15].
Conclusion
The occurrence of osteomas involving the ocular orbit is rare, with the primary occurrence of this tumour in the orbit being even rarer. The total resection of the osteoma in the orbit combined with the immediate reconstruction with titanium mesh in this case was satisfactory, recovering the patient’s anatomical contour without interfering with the function of the ocular globe.
Informed consent: Informed consent was obtained from the patient involved in the case.
[1]. Selva D, White VA, O’Connell JX, Rootman J, Primary bone tumors of the orbitSurv Ophthalmol 2004 49(3):328-42.10.1016/j.survophthal.2004.02.01115110669 [Google Scholar] [CrossRef] [PubMed]
[2]. Sanchez Burgos R, González Martín-Moro J, Arias Gallo J, Carceller Benito F, Burgueño García M, Giant osteoma of the ethmoid sinus with orbital extension: craniofacial approach and orbital reconstructionActa Otorhinolaryngologica Italica 2013 33:431-34. [Google Scholar]
[3]. Gundewar S, Kothari DS, Mokal NJ, Ghalme A, Osteomas of the craniofacial region: A case series and review of literatureIndian J Plast Surg 2013 46:479-85.10.4103/0970-0358.12198224459335 [Google Scholar] [CrossRef] [PubMed]
[4]. Blanco Domínguez I, Oteiza Álvarez AV, Martínez González LM, Moreno García-Rubio B, Franco Iglesias G, Riba García J, Frontoethmoidal osteoma with orbital extension. A case reportArch Soc Esp Oftalmol 2016 91(7):349-52.10.1016/j.oftal.2016.01.02526922136 [Google Scholar] [CrossRef] [PubMed]
[5]. Rogers GM, Carter KD, Orbital OsteomaEyeRounds.org June 3, 2011 Avaliable from: http://EyeRounds.org/cases/133-orbital-osteoma.htm [Google Scholar]
[6]. Ata N, Tezer MS, Koç E, Övet G, Erdur Ö, Large frontoorbital osteoma causing ptosisJ Craniofac Surg 2017 28(1):e17-e18.10.1097/SCS.000000000000316427831979 [Google Scholar] [CrossRef] [PubMed]
[7]. Benatiya Andaloussi I, Touiza E, Bhallil S, Oudidi A, Bouayed MA, Daoudi K, Orbital osteoma: three case reportsBull Soc Belge Ophtalmol 2006 (300):73-79. [Google Scholar]
[8]. Wei LA, Ramey NA, Durairaj VD, Ramakrishnan VR, Cruz AV, Dolman PJ, Lucarelli MJ, Orbital osteoma: clinical features and management optionsOphthalmic Plast Reconstr Surg 2014 30(2):168-74.10.1097/IOP.000000000000003924614547 [Google Scholar] [CrossRef] [PubMed]
[9]. Neville B, Damm DD, Allen C, Bouquot J, Oral and Maxillofacial Pathology 2009 3rd edSaunders, St Louis [Google Scholar]
[10]. Takeuchi S, Tanikawa R, Tsuboi T, Noda K, Miyata S, Ota N, Surgical case of intracranial osteoma arising from the falxOncol Lett 2016 12(3):1949-52.10.3892/ol.2016.483327588144 [Google Scholar] [CrossRef] [PubMed]
[11]. Manjunatha BS, Das N, Sutariya R, Ahmed T, Peripheral osteoma of the body of mandibleBMJ Case Rep 2013 2013:pii: bcr201300985710.1136/bcr-2013-00985723929608 [Google Scholar] [CrossRef] [PubMed]
[12]. Samil KS, Yasar C, Ercan A, Hanifi B, Hilal K, Nasal cavity and paranasal sinus diseases affecting orbitJ Craniofac Surg 2015 26(4):e348-51.10.1097/SCS.000000000000182726080260 [Google Scholar] [CrossRef] [PubMed]
[13]. Gökalp MA, Gözen A, Ünsal Sş, Önder H, Güner S, An alternative surgical method for treatment of osteoid osteomaMed Sci Monit 2016 22:580-86.10.12659/MSM.89698826898923 [Google Scholar] [CrossRef] [PubMed]
[14]. Han BL, Shin HS, Alternative treatment of osteoma using an endoscopic holmium-YAG laserArch Plast Surg 2012 39(4):422-25.10.5999/aps.2012.39.4.42222872849 [Google Scholar] [CrossRef] [PubMed]
[15]. Gabrielli MF, Monnazzi MS, Passeri LA, Carvalho WR, Gabrielli M, Hochuli-Vieira E, Orbital wall reconstruction with titanium mesh: retrospective study of 24 patientsCraniomaxillofac Trauma Reconstr 2011 4(3):151-56.10.1055/s-0031-128612022942944 [Google Scholar] [CrossRef] [PubMed]