Hypertension is one of the common complications of Pregnancy and is known to contribute significantly to Maternal and Perinatal Morbidity and Mortality. Hypertensive disorders of pregnancy include Gestational hypertension, Pre-eclampsia, Eclampsia, Chronic hypertension, Chronic hypertension with Superimposed Pre-eclampsia [1]. In developing countries, they rank 2nd only to anaemia with approximately 7-10% of all the pregnancies being complicated by some form of hypertensive disease [2]. Intrauterine growth restriction (IUGR) is a common complication of Hypertensive disorders of pregnancy and is due to failure of normal placental invasion and development [3,4]. Identification of the pregnancies at risk for preventable perinatal morbidity and mortality is a primary goal of obstetric care [5]. Doppler velocimetry provides valuable information about haemodynamic status of the fetus and is an efficient diagnostic test of fetal jeopardy that helps in management of high-risk pregnancy [6].
Umbilical artery Doppler velocimetry is the most rigorously evaluated test among the non-invasive tests of fetal wellbeing. A meta-analysis of randomised controlled trials of umbilical artery Doppler velocimetry in high-risk pregnancies (mainly pregnancies with associated pregnancy induced hypertension and suspected IUGR) demonstrated that its use was associated with trend towards reduction of perinatal mortality [7]. Doppler evaluation of blood flow through cerebral vessels allows detection of altered cerebral circulation, much before significant fetal heart rate changes due to hypoxemia. Middle cerebral artery is the most accessible vessel and has been reported to demonstrate reduction in the Pulsatility index at onset of hypoxemia [8]. Uterine blood flow Doppler waveform shape is unique, characterised by high diastolic velocity similar to those in systole and highly turbulent flow, with many different velocities apparent. Diastolic velocity increases and thus the indices decrease as term approaches [9]. Failure of the pattern to appear or the presence of a notch in the wave form at the end systole has been reported with fetal growth restriction [10].
Doppler flow studies are an important adjunct to fetal biometry in identifying the fetus at risk of adverse outcome. Placental insufficiency is the primary cause of IUGR in normally formed fetuses and can be identified using umbilical artery Doppler velocimetry [11-13]. The most widely used arterial indices are Pulsatility index, systolic/diastolic ratio; resistivity index. The essential vessels to be examined include the umbilical artery, MCA. The fetal protective mechanisms get triggered as the vascular impedance in the placenta increases and it is reflected in Doppler studies. During course of pregnancy the uterine artery changes from a high resistance pattern with notches to a low resistance pattern with no notches. Normally, the notch is seen until 24 weeks of gestation, persistence of notch after 26 weeks is an indication of hypertensive complications/IUGR/both. Risk of perinatal mortality increases by up to 60% with increasing severity from reduced to reversed end diastolic flow velocity. Therefore, in presence of reversal of diastolic flow in umbilical artery, delivery by cesarean section may be considered if fetal viability is achieved.
The most sensitive and specific index in predicting major perinatal adverse outcome is the S/D ratio of MCA/UA is (83% and 75%), while the most sensitive index in predicting any adverse perinatal outcome (including both major, like perinatal deaths and minor outcome, like fetal distress) is the S/D ratio of umbilical artery (66.6%). The most specific index (90.9%) for predicting any adverse perinatal outcome is the MCA Pulsatility Index (PI). By combining multiple vessels, the sensitivity of the Doppler studies can be significantly increased (91.6%). Doppler studies of multiple vessels like Umbilical artery, middle cerebral artery and Uterine artery Doppler in the feto-placental circulation helps in not only monitoring of compromised fetus but also can help in predicting neonatal morbidity [14].
Cerebro-placental ratio incorporates data of both umbilical artery (Placental status) and middle cerebral artery (Fetal response) and is a better index than using either of them alone for predicting adverse perinatal outcome.
IUGR is most commonly caused by placental insufficiency and in response to this; the fetus adapts the circulation to preserve oxy genandnutrient supply to the brain which is called as ‘brain-sparing’ effect [15]. Yalti S et al., in their study showed that 75% of babies with MCA/UA <1 required NICU admission compared to 5.9% babies with MCA/UA >1 [16]. Ebrashy A et al., carried out a case-control study with MCA/UA RI <1.0 considered as abnormal showed a relative risk of 1.4 [17]. These studies have shown that perinatal morbidity is more with abnormal CPR. Thus, the present study aimed to determine the role of CPR in women with hypertensive disorders of pregnancy, so as to assess the fetus at greater risk of adverse perinatal outcome with reference to NICU admissions, APGAR score and birth weight.
Materials and Methods
The cohort study was conducted after the approval of the Institutional Ethical Board Vide Letter No-JSSMC/IEC/04/1506/2016-17, after informed consent on women attending the obstetrics and gynaecology outpatient department in JSS Hospital, Mysore.
Inclusion Criteria
Singleton pregnancy, gestational age of 32 completed weeks at the time of study, women with hypertensive disorders of pregnancy like Gestational hypertension, Pre-eclampsia, chronic hypertension and pre-eclampsia superimposed on chronic hypertension.
Exclusion Criteria
Multiple gestations, fetal anomalies, known maternal metabolic disorders/vascular diseases.
The subjects satisfying inclusion and exclusion criteria of the study from November 2016 to Nov 2018 in JSS Hospital, Mysore were studied. The sample size of 128 was calculated with the assumption of Type 1 error 5%, power of study 80%.
Methodology
After assessment of inclusion and exclusion criteria, 128 Antenatal women of >32 weeks of gestation were selected for the study, their preliminary data were recorded and were examined clinically. They were subjected to ultrasound scan for fetal presentation, placental position, fetal heart rate, approximate ultrasonography age, Umbilical artery pulsatility index, Middle cerebral artery pulsatility index. Cerebro-placental ratio will be calculated from Middle cerebral artery pulsatility index and Umbilical artery pulsatility index. Patients were divided into two groups depending on Cerebro-placental ratio. A Cerebro-placental ratio of >1.0 to be considered as normal and Cerebro-placental ratio <1.0 to be considered as abnormal. Follow-up with respect to fetal outcome for live birth or still birth, the 5 minute APGAR score, birth-weight and admissions to neonatal intensive care unit.
Statistical Analysis
Data were entered into Microsoft Excel (Windows 7; Version 2007) and analyses were done using the Statistical Package for Social Sciences (SPSS) for Windows software (version 22.0; SPSS Inc, Chicago). Descriptive statistics such as mean and Standard Deviation (SD) for continuous variables, frequencies and percentages were calculated for categorical variables were determined. Association between Cerebro-Placental Ratio and other categorical Variables were analysed using chi-square test. Pearson’s Correlation coefficient was used to show correlation between Cerebro-Placental Ratio and other quantitative variables like birth weight. Bar charts and Pie charts were used for visual representation of the analysed data. Level of significance was set at 0.05.
Results
[Table/Fig-1] shows the maternal and perinatal characteristics of study population. Majority of the study population, about 64.1% were primigravida, while the rest 35.9% were multiparous. Among the pregnancy related hypertension, pre-eclampsia was the most common cause (71.1%), followed by eclampsia (20.3%). Most of the deliveries were at term (65.6%).
Maternal and perinatal characteristics of study population (n=128).
| Characteristics | N | Percentage |
|---|
| Parity |
| Primipara | 82 | 64.1% |
| Multipara | 46 | 35.9% |
| Pregnancy complication |
| Eclampsia | 26 | 20.3% |
| Pre-eclampsia | 91 | 71.1% |
| Gestational HTN | 11 | 08.6% |
| Gestational age at delivery |
| Preterm ≤37 weeks | 44 | 34.4% |
| Term >37 weeks | 84 | 65.6% |
| Delivery |
| Normal vaginal delivery | 26 | 20.3% |
| Caesarean section | 102 | 79.7% |
| Fetal outcome |
| Live births | 118 | 92.2% |
| Still birth | 10 | 07.8% |
| APGAR score at 5 minutes |
| Score ≤7 | 28 | 21.8% |
| Score >7 | 100 | 78.2% |
| Birth weight |
| <1 kg | 5 | 3.9% |
| 1 kg-1.5 kg | 13 | 10.2% |
| 1.5 kg-2.5 kg | 44 | 34.3% |
| >2.5 kg | 66 | 51.6% |
| Admission to NICU |
| No | 49 | 38.3% |
| Yes | 79 | 61.7% |
Fetal outcome: about 92.2% babies were live births, while the rest (7.8%) were still born. Among the live births, 6 babies died in neonatal period. The five minutes APGAR score was ≤7 in 21.8% while the rest had a score of >7 (78.2%). Majority of the babies had birth weight >2.5 kg which accounted for nearly about 51.6% and nearly 61.7% babies did not require any NICU care. Mean maternal age was 24.74 years (range 18-37 years) [Table/Fig-2].
Distribution of study subjects according to their age group (N=128).
| Age (in years) | No. |
|---|
| 18-24 | 65 (50.8%) |
| 25-29 | 48 (37.5) |
| 30-34 | 12 (9.4%) |
| ≥35 | 3 (2.3%) |
| Mean (SD) | 24.74 (4.07) |
| Range | 18-37 |
The mean gestational age was around 36.78 weeks (range 32-41 weeks) as shown in [Table/Fig-3]. About 34.4% patients delivered preterm i.e., before 37 completed weeks.
Distribution of study subjects according to the gestational age.
| Gestational age (in weeks) | No. |
|---|
| 32 | 13 (10.2%) |
| 33 | 8 (6.3%) |
| 34 | 4 (3.1%) |
| 35 | 8 (6.3%) |
| 36 | 11 (8.6%) |
| 37 | 24 (18.8%) |
| 38 | 29 (22.7%) |
| 39 | 17 (13.3%) |
| 40 | 11 (8.6%) |
| 41 | 3 (2.3%) |
| Mean (SD) | 36.78 (2.46) |
| Range | 32-41 |
The MCA PI had a mean value of 1.22, with the scores ranging in between 0 to 1.96; The Umbilical artery PI had mean value of 1.34 (range 0-2.6). The CPR was calculated and showed a mean value of 0.92, ranging between 0 to 1.63; the value below 1.0 was considered as abnormal, and value above 1.0 was considered abnormal [Table/Fig-4].
Descriptive statistics of MCA pulsatility, UA pulsatility and CPR.
| Parameter | Mean (SD) | Range |
|---|
| MCA | 1.22 (0.39) | 0-1.96 |
| UA | 1.34 (0.52) | 0-2.6 |
| CPR | 0.92 (0.41) | 0-1.63 |
Based on the CPR values, the study population data were analysed, by applying chi-square test, to look for any association. There was significant association between the Ultrasonographic gestational age and CPR wherein >32 weeks of gestation, showed abnormal CPR (value <1), significantly higher when compared to patients of <32 weeks [Table/Fig-5].
Association between USG GA and CPR.
| USG GA | CPR |
|---|
| Abnormal (n=63)n (%) | Normal (n=65)n (%) |
|---|
| <32 | 11 | 4 |
| ≥32 | 52 | 61 |
Chi-square test; p-value=0.047; Significant
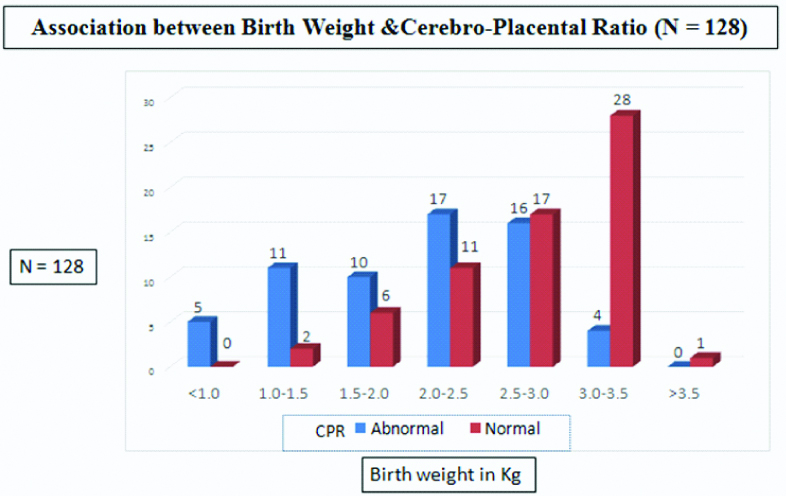
There was a statistically significant association between the birth weight of babies and the CPR values [Table/Fig-6,7].
Association between Birth Weight and CPR.
| Birth weight (kg) | CPR |
|---|
| Abnormal (n=63) n (%) | Normal (n=65) n (%) |
|---|
| <1.0 | 5 | 0 |
| 1.0-1.5 | 11 | 2 |
| 1.5-2.0 | 10 | 6 |
| 2.0-2.5 | 17 | 11 |
| 2.5-3.0 | 16 | 17 |
| 3.0-3.5 | 4 | 28 |
| >3.5 | 0 | 1 |
Chi-Square Test; p-value <0.001; Significant
Association between birth weight and cerebro-placental ratio. It can be seen that, babies with low birth weight had much abnormal CPR values than babies weighing >2.5 kg.
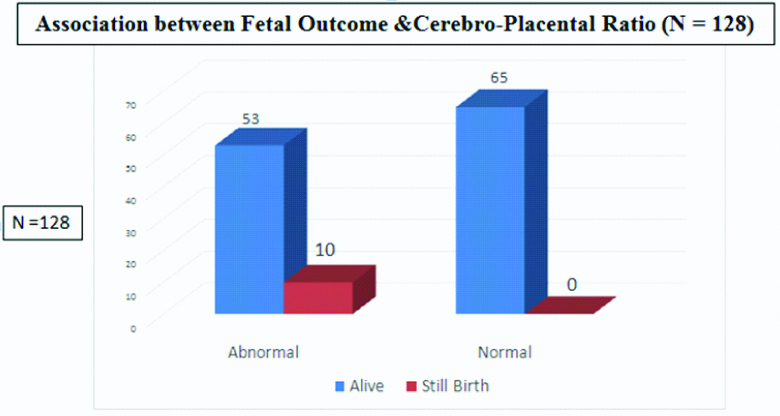
There was a statistically significant association between fetal outcome, in terms of live birth/still birth and CPR value. Among the live births, 53 babies had abnormal CPR values, while about 65 babies had normal CPR values [Table/Fig-8,9].
Association between fetal outcome and CPR.
| Fetal outcome | CPR |
|---|
| Abnormal (n=63) n (%) | Normal (n=65) n (%) |
|---|
| Alive | 53 | 65 |
| Still birth | 10 | 0 |
Chi-square test; p-value=0.001; Significant
Association between fetal outcome and CPR, showing abnormal CPR in all still born babies.
Lower APGAR score at 5th minute was associated with abnormal CPR values, especially the babies with APGAR score of ≤7 at 5 minutes. There was a statistically significant association between APGAR score at five minutes and CPR values, with lower scores having abnormal CPR and higher scores having normal CPR [Table/Fig-10].
Association between APGAR Score at 5 minutes and CPR.
| APGAR score at 5 minute | CPR |
|---|
| Abnormal (n=63) n (%) | Normal (n=65) n (%) |
|---|
| 0 | 10 | 0 |
| 5 | 2 | 0 |
| 6 | 2 | 1 |
| 7 | 10 | 4 |
| 8 | 19 | 23 |
| 9 | 20 | 37 |
Chi-square test, p-value=0.002, Significant
Although abnormal CPR babies were admitted in NICU, more than the normal CPR babies, it was not statistically significant to contribute for NICU care. The babies admitted in NICU had neonatal complications, most common of which was sepsis, followed by periventricular haemorrhage, hypoxic/anoxic encephalopathy [Table/Fig-11]. The study population showed significant correlation between Gestational age (both as per LMP and USG), birth weight, APGAR at five minutes and CPR values. All the values were statistically significant (p<0.001) [Table/Fig-12].
Association between NICU Admission and CPR.
| NICU admission | CPR |
|---|
| Abnormal (n=63) n (%) | Normal (n=65) n (%) |
|---|
| Yes | 44 | 35 |
| No | 19 | 30 |
Chi-square test; p-value=0.063; Not Significant
Correlation between CPR and various other parameters.
| Parameter | Correlation coefficient | p-value |
|---|
| GA | 0.315 | <0.001 |
| USG GA | 0.432 | <0.001 |
| Birth weight | 0.565 | <0.001 |
| APGAR at 5 min | 0.659 | <0.001 |
Discussion
CPR represents the interaction of alterations in blood flow to the brain and is manifested by increased diastolic flow. It is due to the cerebrovascular dilatation resulting from hypoxia and increased placental resistance causing decreased diastolic flow of the umbilical artery [18]. Increase in diastolic flow with decreased pulsatility index shows the brain sparing taking place in compromised fetuses [19-21]. Cerebral placental ratio is constant during pregnancy especially after 30 weeks and 1 is used as the cut off value; all values <1 are considered abnormal [22]. In this present study, it was shown that the Middle Cerebral Artery Pulsatility Index (MCA PI) had a mean value of 1.22 (range 0 to 1.96). The Umbilical Artery (UA) pulsatility index had mean value of 1.34 (range 0-2.6). The CPR was calculated and showed a mean value of 0.92, ranging between 0 to 1.63, the value below 1.0 was considered as abnormal, and value above 1.0 was considered as normal.
There was significant association between the Ultrasonographic gestational age and CPR of study population. Patients who were >32 weeks of gestation as per USG study, showed abnormal CPR (value <1), significantly higher when compared to patients of less than 32 weeks of gestation. It was also found that CPR did not vary with maternal age, inferring that there was no influence of maternal age on CPR. There is statistically significant association between the birth weight of babies and the CPR values, with babies weighing low, had significantly lower (abnormal) CPR values compared to the ones who had higher birth weight. This is consistent with the results obtained by Adiga P et al., who studied the value of CP ratio in prediction of neonatal outcomes that had good negative predictive value in predicting adverse neonatal outcome [23].
Fetal outcome was measured in terms of following parameters. There is statistically significant perinatal morbidity in terms of still birth and neonatal death in the study population who showed abnormal CPR values. Overall this study showed statistically significant association between fetal outcome, in terms of live birth/still birth and CPR value. Lower APGAR score at 5th minute was associated with abnormal CPR values, especially with the babies having APGAR score of ≤7 at five minutes. There is statistically significant association between APGAR score at five minutes and CPR values, with lower scores having abnormal CPR and higher scores having normal CPR. Although abnormal CPR babies were admitted in NICU, more than the normal CPR babies, it was not statistically significant to contribute for NICU care.
The study population showed significant correlation between Gestational age (both as per LMP and USG), birth weight, APGAR at 5 minutes and Cerebro Placental Ratio values. All the values were statistically significant (p<0.01). On the other hand Eser A et al., in their cross-sectional study that included 185 women, that studied the predictive value of CP ratio in prediction of neonatal outcomes in preeclampsia [24] showed no significant positive correlation between abnormal CP ratio and poor Apgar score, as p-value=0.1, showed no significant positive correlation between abnormal CP ratio and poor APGAR score, as p-value=0.1. Redistribution of blood flow occurs at an early stage in fetal adaptation to hypoxemia (brain-sparing reflex), wherein there will be an increased end diastolic flow resulting in decrease in Middle Cerebral Artery PI and RI. Present study showed similar findings of decrease in the MCA Doppler indices with an elevated umbilical artery resistance. Low index of pulsatility in the MCA associated fetal compromise has been described by many authors.
The study conducted by Gaikwad PR et al., showed the Cerebro-placental ratio showed highest specificity (98.55%), PPV (94.44%) and diagnostic accuracy (80.19%) in predicting adverse perinatal outcome and it is better than MCA PI and UA PI alone. The findings of this study echo similar features [25]. In a study conducted by El Guindy AE et al., they demonstrated Cerebro-uterine ratio and cerebro-placental ratio were complementary to each other in predicting the adverse neonatal outcomes than any of the ratios alone [26]. This study shows that CPR alone also can be used as a reliable predictor of neonatal outcome. MCA/UA Pulsatility index ratio or the Cerebro-placental ratio is potentially more advantageous in predicting perinatal outcome as it not only incorporates data on the placental status but also on fetal response.
Limitation
The limitation of this study was it was a hospital-based study and hence it cannot be generalised to the whole population.
Conclusion
Hypertensive disorders of pregnancy do have a significant impact on perinatal outcome. CPR assesses parameters on the placental side and also the fetal response. Doppler of the fetal circulation plays a crucial role in monitoring the redistribution of blood to the fetus and would help to determine the optimal time for delivery and predicting outcome. Present study shows that abnormal CPR is valuable in predicting the outcome of hypertensive disorders in pregnancy. Perinatal outcomes namely, preterm delivery, caesarean section and fetal compromise like low birth weight, lower APGAR at 5 minutes, requirement of NICU care can be predicted with lower CPR.
Chi-square test; p-value=0.047; Significant
Chi-Square Test; p-value <0.001; Significant
Chi-square test; p-value=0.001; Significant
Chi-square test, p-value=0.002, Significant
Chi-square test; p-value=0.063; Not Significant