Febrile thrombocytopenia is frequently encountered by physicians during peri-monsoon and monsoon periods. Fever is defined as an increase in body temperature above the normal circadian range due to the change in the hypothalamic set point. Morning temperature of >37.2°C (98.9°F) or an evening temperature of >37.7°C (99.9°F) is considered as fever [1]. It is an easily noted and reliable sign of sickness.
Platelets play a central role in normal haemostasis. Thrombocytopenia is defined as platelet count <1,50,000/μL. This can be due to decreased production, increased destruction or increased sequestration in spleen [1]. Infections like dengue, leptospirosis, malaria, rickettsia, septicaemia, typhoid, tuberculosis and HIV are some of the most common causes of fever with thrombocytopenia [2]. In some cases, severe thrombocytopenia often leads to life-threatening complications like intra-abdominal or intra-cerebral bleeding. The creditability of platelet count as a reliable parameter to determine the need for platelet transfusion is still debatable [3].
According to European Directorate’s guide to ‘Preparation, use and quality assurance of blood components’, the decision to transfuse platelets should not be based on platelet counts alone and patient’s clinical condition must be taken into account [4].
Currently, there are no guidelines for platelet transfusion in febrile thrombocytopenia. Irrational blood transfusions may have adverse effects on patients and also overwhelm blood banks, jeopardizing their supply in essential cases.
Therefore, the need of the hour, is to develop a scoring system for febrile thrombocytopenia to predict case mortality, length of hospital stay and need of emergency interventions including platelet transfusions.
Kshirsagar P et al., developed a risk assessment scoring system for febrile thrombocytopenia to aid physicians for designing the course of treatment. This retrospective study was conducted on a smaller sample size, thus sanctioning the need for another study with a larger sample size and due consideration for both aetiology and comorbidities [5].
The present study was designed to validate this clinical scoring system, correlate aetiology, comorbidities and platelet count with clinical score and outcome predicting patients’ with febrile thrombocytopenia.
Materials and Methods
The prospective observational study was conducted on 465 (aged 18-85 years) participants at the Department of General Medicine, R.L. Jalappa Hospital associated with Sri Devaraj Urs Medical College, Kolar, Karnataka.
Patients admitted in medical wards during monsoon and peri-monsoon period (June-December 2017) with fever and thrombocytopenia were recruited. Instituional Ethical Committee approval was taken (registration No: SDUMC/KLR/IEC/72/2017-18). Informed written consent was obtained from all patients.
Patients with history of fever >99.0°F and platelet count <1,50,000/mm3 were selected.
Patients on drugs causing thrombocytopenia or previously diagnosed patients with chronic thrombocytopenia were excluded from the study.
Careful history was recorded. General physical examination and detailed examination of all systems was performed. Clinical examination findings of patients with respect to neurological status, respiratory, renal, hepatic and hematological systems was noted.
CNS complications like encephalopathy, encephalitis, meningitis, seizures were assessed based on history, lumbar puncture, CT or MRI brain whenever necessary. Respiratory complications like pulmonary oedema, ARDS, pulmonary hemorrhage was noted based on ABG, chest X-radiograph. Renal complications like acute renal failure, acute tubular necrosis was noted based on urine output, renal function test and routine urine examination. Hepatic complications like acute hepatitis, fulminant hepatic failure, cholecystitis, cholangitis was noted based on liver function test, USG abdomen and coagulation profile whenever needed. Haematological complications were noted based on history, petechiae, purpura, bleeding from any orifices and other complications like intra-cranial or intra-abdominal bleeding.
Routine investigations such as complete blood count, plasma glucose, blood urea, serum creatinine, serum electrolytes, liver function tests, ECG, Chest X-ray and USG abdomen was done. Dengue serology, peripheral smear for Malarial parasite, Weil Felix test for Leptospira were done. Cause of fever was tabulated accordingly.
Risk score was calculated as shown in [Table/Fig-1]. Patients were assigned a score of 1, 2 or 3 based on the pulse, temperature, respiratory rate, blood pressure, platelet count, central nervous system, respiratory, haematological, hepatic and renal complications. Total score was calculated, and patients were grouped into Low (≤7), Moderate (8-15) and High risk (16-26) groups [5].
Clinical risk scoring system [5].
| Score |
|---|
| Parameters | 1 | 2 | 3 |
| Platelet counts (/mm3) | >1,00,000 | 20,000-1,00,000 | <20,000 |
| Systolic blood pressure (mmHg) | >90 | ≤90 | |
| Pulse (/minute) | <100 | ≥100 | |
| Respiratory rate (/minute) | <20 | ≥20 | |
| Temperature (°F) | <100 | ≥100 | |
| CNS complications | | | Present |
| Respiratory complications | | | Present |
| Haematological | | | Present |
| Hepatic complications | | | Present |
| Renal complications | | | Present |
Data was entered into Microsoft excel data sheet and analysed using Statistical Package for the Social Sciences (SPSS) version 20 software. Non-parametric Chi-square, Unpaired t-test and one way ANOVA were applied in comparative analysis of results between different groups. The p-value <0.05 was considered as statistically significant. Mean values, standard deviation, prevalence was assessed wherever relevant.
Outcome of the patient was assessed in each group. Patients were routinely screened until they were symptom-free and had platelet count >1,00,000/mm3 with increasing trend in platelets. For follow-up, the platelets were re-measured after 7 days post-discharge.
Results
A total of 465 patients, 279 (60%) male and 186 (40%) females fullfilling the inclusion and exclusion criteria were recruited in the study.
The mean age of presentation was 34.6±14.19 years (18-85 years). The patients were classified into 3 groups based on their age (18-30, 30-60 and >60 years). There were 225 patients in the age group 18-30, 217 between 30-60 and 23 patients were >60-years-old.
Average duration of fever before hospitalisation was 4.46±2.86 days, in high risk group it was 3.96 days compared to 4.45 in low and 4.51 in moderate group. This shows that high risk group patients sought help earlier than low and moderate risk.
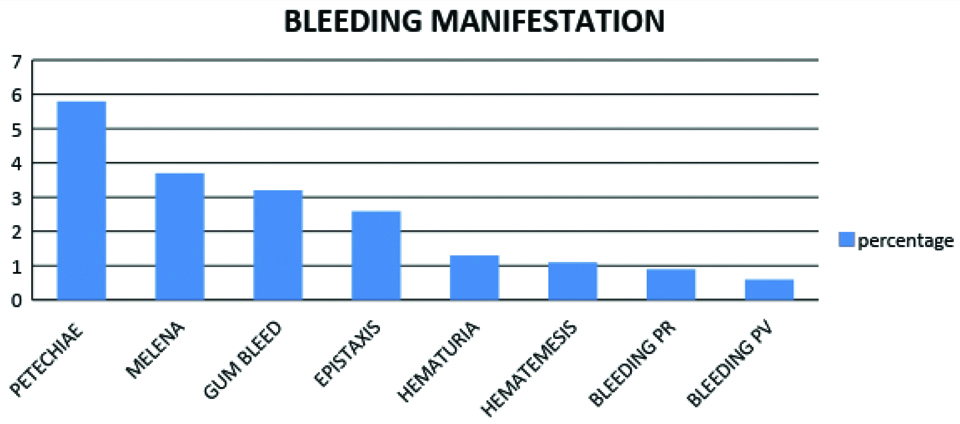
We observed, 81 patients had bleeding manifestations, 27 patients had petechiae followed by melena (17), bleeding gums (15), epistaxis (12), haematuria (6), haematemesis (5) bleeding per rectum (PR) (4) and bleeding per vagina (PV) in 3 patients [Table/Fig-2]. None of the patients had life threatening bleeding manifestation.
Bleeding manifestations of patients under study.
The vital parameters were measured at admission, 36 patients had SBP <90 mmHg, 116 patients had PR >100/min and 4 had PR <60/min, 117 patients had RR >20/min. [Table/Fig-3].
Vital Parameters of patients at admission.
| Temperature (°F) | Respiratory rate/Min | Pulse rate/Min | Systolic BP (mmHg) | Diastolic BP (mmHg) |
|---|
| Mean | 99.61 | 18.23 | 89.75 | 113.63 | 72.02 |
| SD | 0.74 | 4.31 | 14.88 | 15.52 | 12.94 |
The average duration of hospital stay was 5.794±2.25 days. It was the longer in high risk group average being 6.34 days compared to 5.7 in low and moderate group.
The patients were divided into 4 groups according to their day 1 platelet levels [Table/Fig-4]. The average platelet count at admission was 60116/mm3, those who died had 42888/mm3 and the average platelet count of patients receiving transfusion was 26725/mm3 and with hematological complication was 41851/mm3 [Table/Fig-5]. The lowest platelet count with which patient presented to us was 2000/mm3.
Platelet classification of patients under study.
| Group | Platelet Count/mm3 | Frequency | Percentage |
|---|
| 1 | <20000 | 96 | 20.64 |
| 2 | 20000-50000 | 146 | 31.39 |
| 3 | 50000-100000 | 128 | 27.52 |
| 4 | >100000 | 95 | 20.43 |
Average platelet count of patients at admission.
| Patients | Average platelet count at admission (per mm3) |
|---|
| Average platelets | 465 | 60116 |
| Survived | 456 | 60456 |
| Dead | 9 | 42888 |
| Platelet transfused | 135 | 26725 |
| No platelet transfusion | 330 | 73775 |
| Haematological complication | 81 | 41851 |
| No Haematological complications | 384 | 63968 |
Patients were assigned scores according to parameters mentioned in [Table/Fig-1]. In our study the minimum score was 5 and maximum was 24.199 (42.79%) patients fell into low risk, 240 (51.62%) in moderate and 26 (5.59%) in high risk group [Table/Fig-6].
Clinical score and outcome (p-value <0.001).
| Outcome | Total | Percentage |
|---|
| Death | Survived |
|---|
| Risk score | <7 Score (Low risk) | 0 | 199 | 199 | 42.79% |
| 8-15 Score (Moderate risk) | 0 | 240 | 240 | 51.62% |
| >16 Score (High risk) | 9 | 17 | 26 | 5.59% |
| Total | 9 (1.94%) | 456 (98.06%) | 465 | 100 |
There were 9 deaths in our study, which depicts a significant association (p-value <0.001) between score group and death [Table/Fig-6]. The average score of patients who survived was 8.83, and those who died was 19.22.
Significant association was found between age and risk stratification [Table/Fig-7,8]. Elderly individuals had increased risk of poor outcome.
Sex and score correlation.
| Score group | Total |
|---|
| <7 (Low risk) | 8-15 (Moderate risk) | >16 (High risk) |
|---|
| Sex | F | 83 | 93 | 10 | 186 |
| M | 116 | 147 | 16 | 279 |
| Total | 199 | 240 | 26 | 465 |
p-value 0.4239
Age and score (p-value 0.024).
| Score group | Total |
|---|
| <7 (Low risk) | 8-15 (Moderate risk) | >16 (High risk) |
|---|
| Age group | 18-30 years | 100 | 114 | 11 | 225 |
| 30-60 years | 86 | 120 | 11 | 217 |
| >60 years | 13 | 6 | 4 | 23 |
| Total | 199 | 240 | 26 | 465 |
p-value 0.024
The causes for febrile thrombocytopenia were recorded. The most common cause for febrile thrombocytopenia was found to be dengue followed by sepsis, malaria, typhoid, leptospira, rickettsia and HIV. 4 patients had co-infection: 2 patients had dengue with typhoid, 1 patient had HIV and dengue, and other had malaria with dengue which was not statistically significant. In spite of these investigations definitive cause of febrile thrombocytopenia could not be ascertained in 84 patients [Table/Fig-9].
| Score | Low risk (<7) | Moderate (8-15) | High (>16) | Total | Percentage |
|---|
| Dengue | 122 | 145 | 23 | 318 | 68.3 |
| Sepsis | 14 | 19 | 1 | 34 | 7.31 |
| Malaria | 8 | 2 | 0 | 10 | 2.1 |
| Typhoid | 2 | 3 | 0 | 5 | 1.07 |
| Rickettsia | 0 | 4 | 0 | 4 | 0.86 |
| Leptospira | 4 | 2 | 0 | 6 | 1.29 |
| Malaria+Dengue | 1 | 0 | 0 | 1 | 0.21 |
| Typhoid+Dengue | 0 | 2 | 0 | 2 | 0.21 |
| HIV+Dengue | 1 | 0 | 0 | 1 | 0.43 |
| Undetermined | 47 | 35 | 2 | 84 | 18.06 |
| Total | 199 | 240 | 26 | 465 | 100 |
The etiology of febrile thrombocytopenia was found to be associated with risk group [Table/Fig-9]. In the high-risk group, 23 (88.46%) were dengue positive. Risk score with dengue (p-value=0.003), malaria (p-value=0.19), rickettsia (p-value=0.87), leptospira (p-value=0.87), typhoid (p-value=0.58), HIV (p-value=0.62) sepsis (p-value=0.73) and undetermined cause (p-value=0.016) were calculated. Dengue and undetermined febrile thrombocytopenia cases had poor outcome, they needed aggressive management and monitoring compared to other diseases causing febrile thrombocytopenia.
Platelets were transfused to patients with bleeding manifestations or platelets count less than 10000/cumm, 135 patients received platelet transfusion in our study. Total 513 random donor platelet units were transfused and on an average 3.8 RDPs per patient were transfused. Among those who received transfusion, 32 (16%) patients were in low risk group, 85 (35%) in moderate risk and 18 (69%) in high risk group. No association (p-value=0.94) was observed between platelet count and risk score [Table/Fig-10].
Platelet Group and Score.
| Platelet count/mm3 | Total |
|---|
| <20000 | 20000-50000 | 50000-100000 | >100000 |
|---|
| Score | <7 Low risk | 40 | 59 | 54 | 46 | 199 |
| 8-15 Moderate risk | 51 | 78 | 67 | 44 | 240 |
| >16 High risk | 5 | 9 | 7 | 5 | 26 |
| Total | 96 | 146 | 128 | 95 | 465 |
p-value=0.94
Patients who died in our study had a initial platelet presentation between 2,000 to 1,05,000/mm3 (platelet counts were 2000, 5000, 9000, 19000, 40000, 41000, 77000, 88000, 105000/mm3) and their scores were between 17 to 24 with average score of 19.22.
Dengue was diagnosed in 8 patients and cause could not be determined in one patient. Platelets were transfused in 5 patients but platelet transfusion did not have any effect on the mortality of these patients. Among them 2 patients were both diabetic and hypertensive and rest did not have any co-morbidities. All the patients in high risk group needed ICU support and continuous monitoring.
Platelet counts did not have any significant association with outcome of the patient (p-value=0.35) [Table/Fig-11]. Also there was no significant association between co-morbidities and risk score [Table/Fig-12]. Risk score with Type 2 diabetes mellitus (p-value=0.62), hypertension (p-value=0.93), Hypothyroid (p-value=0.57), anaemia (p-value=0.17), seizure (p-value=0.87), CVA (p-value=0.55).
Platelet count and outcome.
| Platelet (mm3) | <20000 | 20000-50000 | 50000-100000 | >100000 | Total |
|---|
| Survived | 92 (95.84%) | 144 (98.63%) | 126 (98.43%) | 94 (98.95%) | 456 |
| Died | 4 (4.16%) | 2 (1.37%) | 2 (1.57%) | 1 (1.05%) | 9 |
| Total | 96 | 146 | 128 | 95 | 465 |
p-value: 0.35
Co-morbidities and score.
| Low (<7) | Moderate (8-15) | High (>16) | Total |
|---|
| T2DM | 21 | 23 | 2 | 46 |
| HTN | 5 | 7 | 3 | 15 |
| Hypothyroid | 4 | 3 | 1 | 8 |
| Anaemia | 1 | 1 | 0 | 2 |
| CVA | 1 | 0 | 0 | 1 |
| Seizure | 2 | 2 | 0 | 4 |
| SLE | 0 | 1 | 0 | 1 |
There was no significant association between platelet count and renal system (p-value=0.507), respiratory (p-value=0.50) or CNS complications (p-value=0.720), however significant association between platelet group and hepatic (p-value <0.001) and hematological complications (p-value <0.001) was observed [Table/Fig-13]. In our study, highest number of organ failure were associated with hepatic complications (28.38%). We tabulated platelet transfusion and organ system complications as in [Table/Fig-14], (53.08%) patients with haematological complications followed by CNS (50%) and hepatic (42.22%), respiratory (40.24%) and renal (25%) complications had platelets transfusion.
Platelet count and organ system complications.
| Complications | <20000 | 20000-50000 | 50000-100000 | >100000 | Total |
|---|
| Respiratory | 24 | 26 | 26 | 6 | 82 (17.63%) |
| Renal | 7 | 8 | 5 | 8 | 28 (6.02%) |
| Hepatic | 42 | 48 | 33 | 9 | 132 (28.38%) |
| Haematological | 30 | 26 | 17 | 8 | 81 (17.41%) |
| CNS | 0 | 2 | 1 | 1 | 4 (0.86%) |
Platelet transfusion and organ system complications.
| Complications | No of patients | Patients receiving platelets | No of platelets transfused | Average no. of platelet transfused |
|---|
| Respiratory | 82 | 33 (40.24%) | 132 | 4 |
| Renal | 28 | 7 (25%) | 28 | 4 |
| Hepatic | 132 | 57 (42.22%) | 233 | 4.08 |
| Haematological | 81 | 43 (53.08%) | 168 | 3.9 |
| CNS | 4 | 2 (50%) | 7 | 3.5 |
Discussion
Febrile thrombocytopenia patients come with varied clinical presentation ranging from self-limiting illness to life-threatening complications which can be fatal, if left untreated. Patients sometimes have multi-organ dysfunction, hence requires intensive care and have significant morbidity and mortality [6,7]. Depending upon the severity of the condition, these patients often require platelet transfusion. However, reliability of platelet count as a sole parameter for determining the need for platelet transfusion is remains debatable [3,7].
In infections, platelet count is reduced both due to decreased platelet production and increased platelet destruction [8]. In severe cases, thrombocytopenia can lead to life-threatening complications like intra-abdominal bleeding and intra-cerebral bleeding. Protect trial demonstrated that adverse effects in medical and surgical ICU had a correlation with the severity of thrombocytopenia but no such study have been done on patients with febrile thrombocytopenia [9].
According to World Health Organisation (WHO), prophylactic transfusion of platelets is not indicated in dengue patient unless the patient has bleeding or a count of less than 10000/mm3 [10].
There is a scoring system in place for many illnesses like stroke, MI and heart failure but there is no system to evaluate patients presenting with febrile thrombocytopenia [11,12]. Kshirsagar P et al., have developed a risk score for febrile thrombocytopenia based on platelet count, vital signs and organ system involvement. Based on these parameters patients were grouped into low, moderate and high-risk groups [5].
In our study, 26 (5.59%) patients were in high-risk group and all 26 needed ICU support, they had increased duration of hospital stay and came early to hospital when compared to others. A total of 23 of them were dengue positive and 11 patients had sepsis. Dengue was found to be most common cause for febrile thrombocytopenia followed by sepsis. Etiology could not be determined in 18.06% patients which was similar to other studies [7-13]. Dengue and undetermined cause patient had a high risk of mortality and morbidity compared to other causes.
In our study, 9 patients died and all of them were in high risk group which showed significant association with mortality (p-value <0.001). Patients who died had a initial platelet presentation between 2,000 to 1,05,000/mm3 with average platelet count of 42888/mm3. Thus indicating that there was no significant relationship between the initial platelet presentation and outcome of the patient.
A significant relationship between age of the patient and risk group (p-value <0.024) was observed. Patients <60 years had a favourable outcome compared to elderly patients.
Similarly no statistically significant association was observed between risk score and co-morbidities. Platelet count and risk group, systemic complications and outcome were analysed. Significant association between platelet count and hepatic and haematological complications was observed but there was no association between platelet count at presentation and outcome of the patient was found.
In our study, 17.41% patients had haematological complications and none of them had any life threatening bleeding manifestation. Some patients had bleeding manifestation with platelets above 100000/mm3 and some had no bleeding manifestation even with platelets less than 5000/mm3. Among the patients that died, four didn’t have any bleeding manifestations. This shows that bleeding manifestations and mortality of patients are not dependent on platelet count alone and platelet count as sole criteria should not be used to gauge the prognosis or for planning further management.
In the study, conducted by Kshirsagar P et al., 3.2% were in high risk group and 2 patients died in their study with score of 17 and 18 with platelet count 20000/mm3 and 100000/mm3 [5]. However, association between aetiology, co-morbidity and patient outcome was reported. They found that there was no significant difference in patient outcome across platelet groups and patients who fall into high risk group have poor prognosis which was similar in our study.
Our study was an observational prospective study and platelets were transfused as per present guidelines i.e., patient with platelets less than 10000/mm3 or in patients with bleeding manifestations. 135 patients underwent platelet transfusion, 32 (16%) patients in low risk group, 85 (35%) in moderate risk and 18 (69%) in high risk group. 16% of platelet transfusion could have been avoided in our study by following the risk score.
With p-value <0.001 there was significant association between risk category and outcome. Patients who fall into high risk category had poor prognosis and required aggressive management. The outcome of the patients was dependent on the risk score and not only on the platelet count at admission. Irrespective of the number of platelets transfused, the prognosis remained poor as the risk score increased.
Based on the scoring system, we recommend that patients with low risk (<7) can be deferred admission with serial monitoring of platelet count where as patients with moderate risk (8-15) should be admitted in wards and the score should be re-analysed every 6-8 hours and judicious transfusion of platelets if clinically necessary. Patients in high risk (>16) group need continuous monitoring with transfusion of platelets in ICU. These recommendations are similar to that of study by Kshirsagar P et al., [5].
The above recommendations, if followed significantly reduces the burden on resource poor-hospitals and blood banks and help in better management of the patients.
Limitation
It was an observational study and no active interventions were done. We recommend similar study in other centers and during different season as there is geographical and seasonal variation in aetiology of febrile thrombocytopenia which may alter the outcome.
Conclusion
This study suggests that Kshirsagar P et al., risk scoring system can intimate the physician about the need for transfusion and to prognosticate patient’s recovery. Patients with dengue and undetermined cause had the poorest outcome. Likewise, patients labelled as high risk and the elderly also proved to have poor outcomes. Bedside versatility, easy reproducibility and it’s cost effective nature prove that this scoring system is one of the foremost tools in guiding physicians in treatment and thus, curtailing the irrational prescription of platelet transfusions.
p-value 0.4239
p-value 0.024
p-value=0.94
p-value: 0.35