Focal liver lesions are best assessed and characterised by multiphasic CT. It is an effective aid in determining the number, location, and nature of such lesions and monitoring their size over time. In patients with cancer, the accurate detection of metastatic disease at the time of diagnosis or during the course of treatment remains crucial to management of the disease.
Multidetector Computed Tomography (MDCT) represents an advance in CT technology that involves the use of a multiple-row detector array instead of the traditional single-row detector array used in spiral CT. This innovation allows scanning four to eight times faster than scanning with spiral CT [1]. A triphasic spiral CT technique images the entire liver in arterial, portal, and equilibrium phases [2,3].
Multiple modalities in radiological imaging along with histopathological characteristics and clinical assessment are used to attain a correct diagnosis [10].
In the available literature, especially in India there are fewer comprehensive studies about the role of multiphasic MDCT scan in characterising liver lesions under benign or malignant category and were conducted with a very small sample size. With the above background, this study was undertaken as an effort to assess the role of MDCT in detection and characterisation of focal liver lesions with a larger sample size and help in deciding further course of management.
Materials and Methods
This cross-sectional study was conducted in the Department of Radiodiagnosis in Era’s Lucknow Medical college and Hospital for a period of 18 months from January 2017 to June 2018 and total of 84 patients were included in the study.
Sample size was calculated on the basis of specification and Positive Predictive Value of MDCT [11] using the formula:
Where, Zα=1.96 (95% CI), P=Prevalence=5% (on the basis of Tertiary Care Hospital- Era’s Lucknow Medical College and Hospital) and C=Margin of error=5%
Loss=10%=8 Then sample size came out to be=84
Adult patients of age group 20-60 years with focal hepatic lesions on abdominal imaging (USG), all patients presenting with deranged liver function or known cases of liver mass lesions and the subjects who were willing to participate in the study and gave their written consent for the same were included in the study. Patients with traumatic liver lesions and patients with deranged blood clotting profile were excluded.
After obtaining approval from the institutional ethical committee (ELMC/R_ cell/EC/2017/11) and written and informed consent from all the patients, they were subjected to a USG scan followed with Quadri-phasic CECT scan and biopsy. Obtained samples were sent for histopathology and biochemical analysis. All the values for the arterial phase, venous phase, portal phase and delayed phase were recorded and all the patients were followed up till histopathological and biochemical report confirmation was done.
Statistical Analysis
Data so obtained were subjected to statistical analysis. Results were evaluated for the best modality through which benign and malignant lesions can be differentiated. Data analysis was done by SPSS software® version 16.0. Descriptive statistical analysis, which included frequency and percentages, was used to characterise the data. Association with the factors was tested for significance using chi-square test and p <0.05 was considered statistically significant.
Results
Out of 84 patients, maximum number of patients was from age group 20-29 years as shown in [Table/Fig-1]. Other demographic details and lifestyle habits are shown in [Table/Fig-2,3].
Age distribution of subjects.
| Age group | No. | % |
|---|
| 20-29 year | 26 | 31.0 |
| 30-39 year | 20 | 23.8 |
| 40-49 year | 18 | 21.4 |
| 50 year and above | 20 | 23.8 |
| Total | 84 | 100.0 |
| Mean | 38.92±11.75 (20-60 year) |
Gender distribution of subjects.
| Gender | No. | % |
|---|
| Male | 44 | 52.4 |
| Female | 40 | 47.6 |
| Total | 84 | 100.0 |
Distribution of subjects according to addictions.
| Addictions | No. | % |
|---|
| Smoking | 29 | 34.5 |
| Alcohol | 22 | 26.2 |
| Tobacco | 24 | 28.6 |
Among the cases, most of them had complaints of abdominal discomfort as shown in [Table/Fig-4].
Distribution of subjects according to complaints.
| Complaints | No. | % |
|---|
| Acute abdomen | 59 | 70.2 |
| Abdominal discomfort | 82 | 97.6 |
| Palpable mass | 57 | 67.9 |
| Abdominal mass | 48 | 57.1 |
| Anorexia | 68 | 81.0 |
| Fever | 34 | 40.5 |
| Weight loss | 62 | 73.8 |
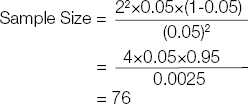
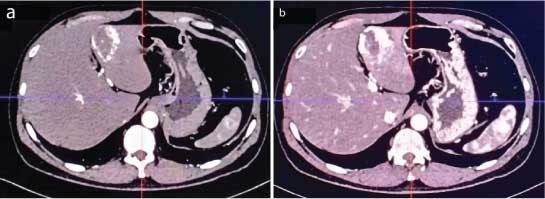
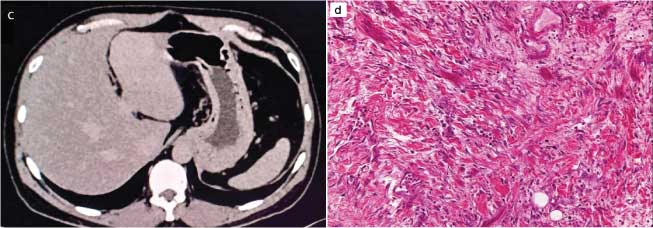
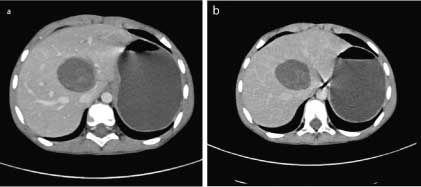
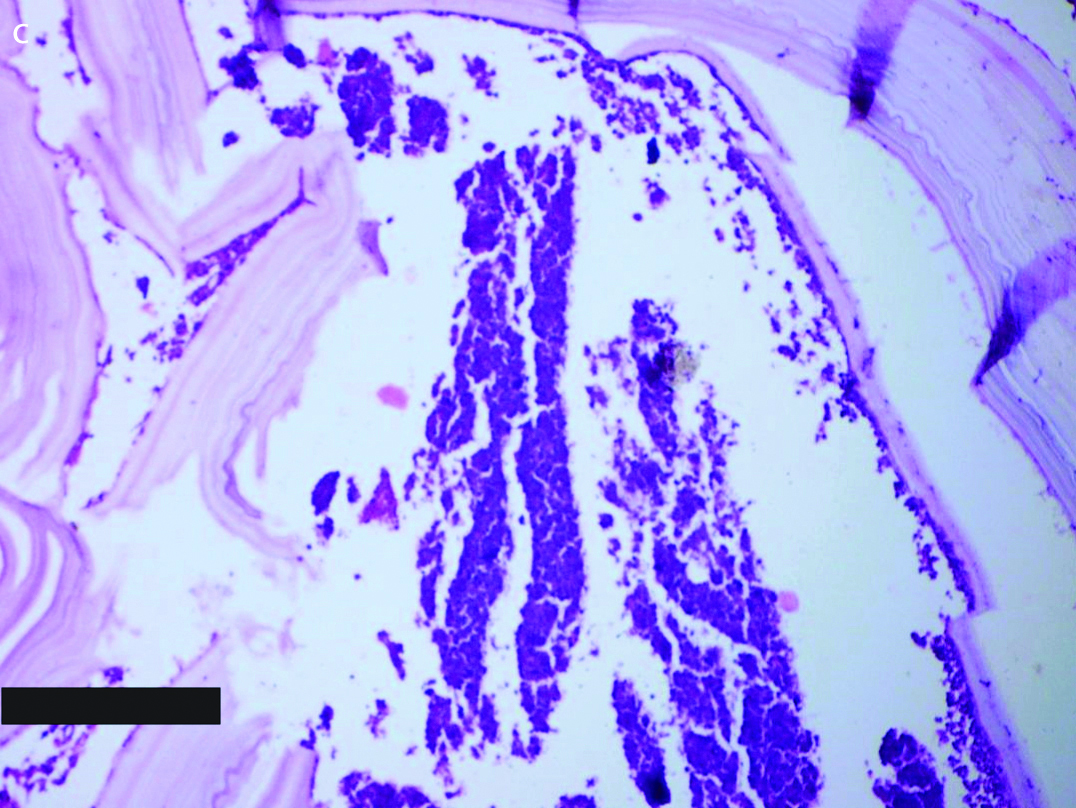
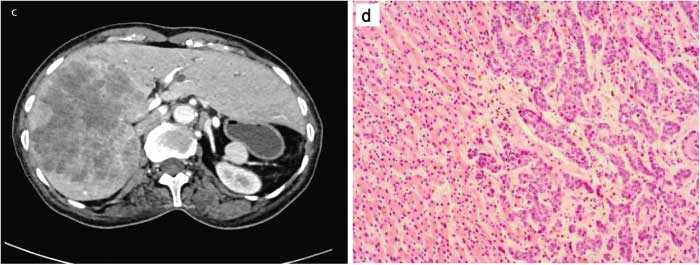
As detected by MDCT, benign and malignant focal liver lesions were seen in 84 patients. Out of 84, benign focal liver lesions were 72 (85.7%) and malignant lesions were 12 (14.3%). Among the benign lesions, maximum cases were of abscess [Table/Fig-5a,b]. Others were Cyst, Haemangioma [Table/Fig-6a,b,c,d], Hydatid cyst [Table/Fig-7a,b,c] and Hepatic Granuloma. Among the malignant lesions MDCT finding was of Hepatocellular carcinoma [Table/Fig-8a,b,8c,d,9].
a) CECT arterial phase image of a liver abscess shows central low density hypoattenuating lesion with peripheral enhancement; b) CECT portal venous phase image of a liver abscess shows peripherally enhancing, centrally hypo-attenuating lesion with persistence of inner ring enhancement.
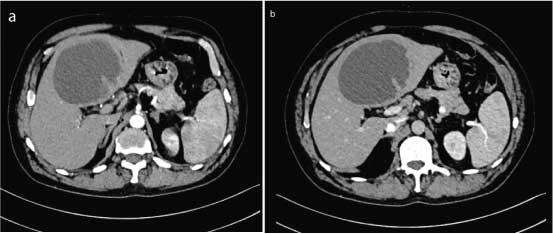
a) CECT arterial phase image of a hepatic haemangioma shows central low-density hypo-attenuating lesion with peripheral enhancement; b) CECT portal venous phase image of a hepatic haemangioma shows peripherally enhancing, centrally hypo-attenuating lesion with persistence of inner ring enhancement.
c) CECT 10 minutes delayed phase axial image of a hepatic haemangioma shows further fill-in and hence lesion appears iso-hyper-attenuating to liver parenchyma; d) Haematoxylin and Eosin stained tissue section (100x magnification) of hepatic haemangioma shows variably sized vascular channels lined by flattened endothelial cells. The vascular channels are separated by fibrous stroma.
a) CECT arterial phase image of a hydatid cyst shows a well-defined fluid density hypo-dense lesion with few enhancing septae within; b) CECT delayed phase image of a hydatid cyst shows a well-defined fluid density hypo-dense lesion with few enhancing septae within.
Haematoxylin and Eosin stained tissue section (40x magnification) of hydatid scolex surrounded by laminated membrane lining the hydatid cyst.
a) CECT arterial phase axial image of hepatocellular carcinoma shows an enhancing mass lesion in right lobe of liver; b) CECT portal phase axial image of hepatocellular carcinoma shows a heterogeneously enhancing mass lesion in right lobe of liver.
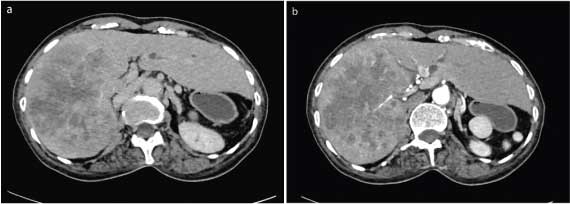
c) CECT delayed phase axial image of hepatocellular carcinoma at 5 minutes shows rapid washout of the contrast from the lesion typical of hepatocellular carcinoma; d) Haematoxylin and Eosin stained tissue section (10x magnification) from the liver tissue shows that malignant cells on the right side are well differentiated and interdigitate with normal hepatocytes arranged in regular cords on the left side.
Prevalence of various lesion types as detected by MDCT.
| Lesion category | Lesion type | MDCT finding | 95% Confidence interval |
|---|
| No. | % | Lower | Upper |
|---|
| Benign | Abscess | 39 | 46.4 | 35.8 | 57.1 |
| Benign | Cyst | 10 | 11.9 | 5.0 | 18.8 |
| Benign | Haemangioma | 13 | 15.5 | 7.7 | 23.2 |
| Malignant | Hepatocellular carcinoma | 12 | 14.3 | 6.8 | 21.8 |
| Benign | Hydatid cyst | 8 | 9.5 | 3.2 | 15.8 |
| Benign | Hepatic Granuloma | 2 | 2.4 | 0.0 | 5.6 |
| Total | 84 | 100.0 | 100.0 | 100.0 |
For detecting various types of lesions, the results of MDCT matched with biopsy in 90.5% cases while in 9.5% cases the results didn’t match. So the diagnostic accuracy (efficiency) of MDCT was found to be 90.5% with predicted value (95% CI: 84.20-96.75%) [Table/Fig-10]. The agreement of MDCT with biopsy findings in liver lesions is shown in [Table/Fig-11]. The overall agreement between MDCT and Biopsy was found to be highly significant (Kappa=0.806, p<0.001).
Correlation of MDCT with biopsy to detect various type of lesions.
| Result | No. | % | Diagnostic accuracy |
|---|
| Unmatched | 8 | 9.5 | 90.5%(95% CI: 84.20-96.75%) |
| Matched | 76 | 90.5 |
| Total | 84 | 100.0 |
Agreement of MDCT with biopsy findings in liver lesions.
| Biopsy diagnosis | MDCT diagnosis | Total |
|---|
| Abscess | Cyst | Haemangioma | Hepatocellular carcinoma | Hydatid cyst | Hepatic granuloma |
|---|
| No. | % | No. | % | No. | % | No. | % | No. | % | No. | % |
|---|
| Abscess | 38 | 100 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 38 |
| Cyst | 0 | 0.0 | 9 | 75.0 | 0 | 0.0 | 0 | 0.0 | 1 | 14.3 | 0 | 0.0 | 10 |
| Haemangioma | 0 | 0.0 | 0 | 0.0 | 13 | 86.7 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 13 |
| Hepatocellular carcinoma | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 7 | 70.0 | 0 | 0.0 | 0 | 0.0 | 7 |
| Hydatid cyst | 0 | 0.0 | 1 | 8.3 | 0 | 0.0 | 0 | 0.0 | 5 | 71.4 | 0 | 0.0 | 6 |
| Biliary Hamartoma | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 1 | 14.3 | 0 | 0.0 | 1 |
| Cystic metastasis | 0 | 0.0 | 2 | 16.7 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 2 |
| focal nodular hyperplasia | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 2 | 20.0 | 0 | 0.0 | 0 | 0.0 | 2 |
| Hepatic adenoma | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 1 | 10.0 | 0 | 0.0 | 0 | 0.0 | 1 |
| Hepatic metastasis | 0 | 0.0 | 0 | | 2 | 13.3 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 2 |
| Hepatic Grannuloma | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 2 | 100.0 | 2 |
| Total | 38 | 100 | 12 | 100 | 15 | 100.0 | 10 | 100.0 | 7 | 100.0 | 2 | 100.0 | 84 |
| Agreement | Kappa = 0.806, p <0.001 |
Among the benign cases detected by MDCT, 97.2% confirmed as benign cases by biopsy. On the other hand, among the malignant cases detected by MDCT only 83.3% cases confirmed as malignant by biopsy [Table/Fig-12]. Highly significant association (chi-sq=54.51, p<0.001) and agreement (Kappa=0.806, p<0.001) was found between MDCT and biopsy techniques. The overall sensitivity, specificity, PPV, NPV and diagnostic accuracy for malignant lesions was found to be 83.3%, 97.2%, 83.3%, 97.2% and 95.2% respectively.
Validity and reliability of MDCT with respect to biopsy for detecting malignancy in liver lesions.
| MDCT | Biopsy | Total |
|---|
| Benign | Malignant |
|---|
| No. | % | No. | % |
|---|
| Benign | 70 | 97.2 | 2 | 2.8 | 72 |
| Malignant | 2 | 16.7 | 10 | 83.3 | 12 |
| Total | 72 | 85.7 | 12 | 14.3 | 84 |
Discussion
In the available literature there are few Indian comprehensive studies about the role of Multiphasic MDCT scan in improving the diagnostic accuracy of characterising the malignant liver lesions.
Risk factors and complaints of the study subjects: Habits like smoking, alcohol consumption and tobacco chewing that are considered as risk factors for malignant liver lesions were present in majority of subjects in our study. Such habits were also proven by Simonetti RG et al., to be risk factors for malignant liver lesions [11].
Validity and reliability for detecting malignant liver lesions: In present study, the overall sensitivity and specificity of MDCT with respect to biopsy, for establishing their validity and reliability in detecting malignancy in liver lesions, was found to be 83.3% and 97.2%, respectively.
In addition, in a meta-analysis of hepatic metastases from cancers of the gastrointestinal tract, Kinkel K et al., reported a mean sensitivity of 72% for CT, based on 25 publications that included 1747 patients [12]. In a study by Khalid M et al., the diagnostic accuracy of metastatic focal hepatic lesions by MRI was 55% as compared with 17% for CT [13]. In this study, more recent comparisons of non-invasive imaging modalities, primarily MDCT and USG, have shown equally accurate if not better lesion detection by MDCT. However, in the present study, cases of abscess show highly significant agreement between MDCT and biopsy techniques. The overall sensitivity and specificity of MDCT was found to be 99.3% and 97.1% respectively. For the cases of cyst, highly significant agreement was found between MDCT and biopsy techniques. The overall sensitivity, specificity, PPV, NPV and diagnostic accuracy of MDCT was found to be 97.9%, 96.6%, 87.9%, 97.9% and 96.7% respectively. Ahirwar CP et al., added that with sensitivity of 91.3%, specificity 97.8%, PPV 91.3% and NPV 97.8% (p-value<0.001, kappa value 0.847), Triple phase CT is excellent diagnostic modality for characterisation and better evaluation of hepatic masses [14]. In diagnosing malignant hepatic lesions, triphasic CT has accuracy of 93%, sensitivity and specificity of 93.3% and 92.5% respectively and with PPV and NPV of 94.9% and 90.2%, respectively. Similarly, in present study, the overall sensitivity and specificity for the cases of haemangioma was found to be 92.3%, 98.6%, respectively.
The hydatid cyst and hepatocellular carcinoma cases showed overall sensitivity and specificity of 97.4%, 96.1%, and 96.9%, 90.4%, respectively. In contrast Hassan and their colleagues had sensitivity and specificity of haemangiomas to be 76.9%, 88.4% and for MRI 85.2% and 91.2%, whereas, in hepatocellular carcinoma, the sensitivity and specificity of CT were 62% and 83.3% and for MRI were 90.3% and 87.5% in metastases, sensitivity and specificity of CT were 60% and 84% and for MRI were 76.2% and 87.8% [15]. These results are somewhat like in previous studies, as mentioned [16,17]. In the study conducted with 64 MDCT and MRI [16], the difference between the detection sensitivity of MRI and MDCT were insignificant. Also, the numbers of false positive MRI findings were the same as or relatively low compared with those for MDCT. Eighty percent of the false-positive MRI results and 67% of the false-positive CT results were primarily attributed to arterio-portal shunt. Furthermore, cirrhosis-related benign nodules may exhibit predominant hypo-attenuation on contrast-enhanced portal or delayed phase CT image [18] and might not be differentiated from hypo-vascular HCC. In another study 33%, of false-positive findings on MDCT were attributed to prominent cirrhosis-related nodules. In a study by Matilde NM et al., 92% of the 100 lesions demonstrate arterial enhancement [19].
Positive predictive values of 82% or greater and specificity of 80% or greater were seen with patterns of abnormal or variegated internal vessels (hepatocellular carcinoma), peripheral puddles (haemangioma) and complete ring (metastasis) [16]. In our study, all the abscesses detected by MDCT confirmed to be abscesses on biopsy also. Cysts seen by MDCT correlated with biopsy findings in 75.0% cases, hydatid cyst in 8.3% cases and cystic metastasis in 16.7% cases. Haemangioma diagnosed by MDCT was confirmed by biopsy in 88.2% cases along with hepatic metastasis which were confirmed in 11.8% cases. Cases of hepatocellular carcinoma detected by MDCT were diagnosed such in 70.0% cases, focal nodular hyperplasia in 20.0% cases and hepatic adenoma in one case (10.0%) by biopsy. Hydatid cyst was also confirmed in 71.4% cases, cyst in 14.3% cases and biliary hamartoma in 14.3% cases by biopsy. Haemangiomas characteristically have discrete well-defined peripheral globules that are iso-attenuating with vascular structures [20]. When all lesions with circumferential ring enhancement were considered, malignancy was predicted with 86.8% specificity for metastasis. As found in this study and others [19], benign and malignant lesions may overlap in appearances, for example, homogeneous pattern can be exhibited by HCC, haemangiomas and FNH. We also found overlap between enhancement of metastasis and peripheral puddles pattern of haemangiomas. Lesions with similar arterial phase enhancement may be differentiated by correlation with portal venous phase images. Few haemangiomas and hyper-vascular metastases were included in present study, but further work was necessary to fully examine their enhancement patterns.
In addition, according to Pattanayak SK et al., the conspicuity of a liver lesion depends on the attenuation difference between the lesion and the normal liver [21]. Due to low contrast in non-enhanced CT scans between tumor tissue and surrounding liver parenchyma, tumors become invisible. As the surrounding liver parenchyma begins to enhance in the portal venous phase, these hyper-vascular lesions may become concealed. The enhancement should have same density as the blood pool in all phases and should be peripheral and nodular. If it is neither a cyst nor a haemangioma, then the lesion should be further studied. Based on the enhancement patterns, we divide the masses into hyper-vascular and hypo-vascular lesions. Usually, a combination of different features like enhancement pattern, pathological features like presence of fat, blood, calcifications, cystic or fibrotic component in the liver lesions along with clinical history is used to frame the differentials. Gupta K et al., also added a significant finding about the role of CT in evaluation of parenchymal focal lesions of liver and concluded that MDCT is a highly sensitive non-invasive tool for detection and characterisation of focal hepatic lesions [22].
Limitation
There are certain limitations of our study like the entire spectrum of focal liver lesions were not covered. Further studies can be conducted to include secondary focal liver lesions such as metastases, biliary hamartomas, etc.
Conclusion
The results of this study prove MDCT to be highly sensitive in sorting the hepatic lesions into clinically relevant categories which helps in achieving correct diagnosis and evaluation of lesion. This study opens new possibilities of prevention of liver disease with early detection and consequent management of hepatic lesions.