Introduction
Pyridoxine or vitamin B6 is a water soluble vitamin of the B-complex group. In human body, the coenzyme form of this vitamin occupies a centre stage in amino acid metabolism in cells. The amino acid catabolism includes catabolism of two components-the carbon skeleton and the amino group. Pyridoxine, in its coenzyme form, is indispensable for both metabolism (transamination and deamination of the amino group, decarboxylation of the carbon skeleton). The coenzyme also plays a major role in glycogen breakdown, neurotransmitter metabolism and hormone metabolism. Beside the dietary and biochemical essentiality, it is also therapeutically important in gynecology. Pyridoxine is believed to be effective in suppression of lactation, however other studies reports similar results to placebo [1-3]. Supplementation of 100 mg vitamin B6/day have shown to relieved depression and normalised glucose tolerance in women taking contraceptives [4]. Vitamin B6 administration has also been shown to prevent etretinate induced development of fetal abnormalities [5].
About 70-80% pregnant women experiences nausea and vomiting, while most pregnant women experience it only in the first trimester, a small percentage of women show a prolonged course of symptoms extending until delivery. A combination of pyridoxine (vitamin B6) (pregnancy category A) and doxylamine (category B), previously known as Bendectin commercially, is the only Food and Drug Administration (FDA) approved medication for treatment of NVP [6]. Alternatively, pyridoxine can be taken on its own in NVP. A vitamin B6 supplementation of 1.9 mg per day has been recommended by The American College of Obstetrics and Gynecology recommend for hyperemesis gravidarum [7]. Improvement in nausea scores were obtained in patients with severe nausea who took pyridoxine and a reduction was seen in the vomiting episodes when compared to women taking placebo [8,9].
Biochemistry and Pharmacochemistry of Pyridoxine
Requirements and dosage: Vitamin B6 requirements in the diet are related to protein intake and not to calorie intake. Deficiency of the vitamin precipitates as neurological, dermatological and hematological manifestations. It is considered that 15 μg/g dietary protein is an adequate intake to meet the requirement of most of the population and that 11 μg/g dietary protein is the minimum safe limit. Current Recommended Dietary Allowances (RDAs) range between 1.5-2.2 mg/day. During pregnancy and lactation, the requirement is increased to 2.5 mg/day. Requirement is known to increase in the elderly as well, and the requirement in infants remains undetermined [10]. Vitamin B6 is naturally obtainable from dried yeast, rice polishings, wheat germs, cereals, legumes, oil seeds, egg, milk, meat, fish and green leafy vegetables. The vitamin supplements are also available for use in times of increased demand by the body. However, doses over 100 mg may lead to imbalance, numbness, muscle weakness and nerve damage and extremely high intakes of 500 mg/day leads to neurological damage [10,11]. [Table/Fig-1] shows the limits on the amounts of pyridoxine that can be given nutritionally or for pharmaceutical purposes, as proposed by the UK department of Health Committee on toxicity in June 1997 [12].
Recommended doses of B6 (UK department of health committee on toxicity, 1997).
| Reference nutrient intake | 1.2-1.5 mg/d |
|---|
| Freely sold as nutritional supplement | Upto 10 mg/d |
| Sold in pharmacy on professional advice | 10-50 mg/d |
| Provided on prescription | >50 mg/d |
Deficiency and toxicity: Vitamin B6 deficiency has been reported to cause seizures in children and rashes; normocytic anemia, cheilitis with scaly lip skin and cracks in the corner of the mouth, non-specific pruritic rash and glossitis in adults. In severe deficiency, it leads to mental status changes or even depression.
More recent studies have implicated the role of B6 deficiency in heart disease, cancer and cognitive decline. Studies also indicate a reduction of symptoms in the premenstrual syndrome (moodiness, irritability, forgetfulness) following B6 supplementation [7,13]. More than 250 mg per day of pyridoxine on a chronic basis, may result in toxic effects on skin, gastro-intestinal, and neurological system [7].
Chemistry: Pyridoxine is one of the three vitamers of the B6 family along with pyridoxal and pyridoxamine. Humans obtain vitamin B6 from diet and from the bacterial microflora of the large intestine [14]. Dietary B6 compounds exist in the free and phosphorylated form that undergoes dephosphorylation to the free form prior to absorption [15-17].
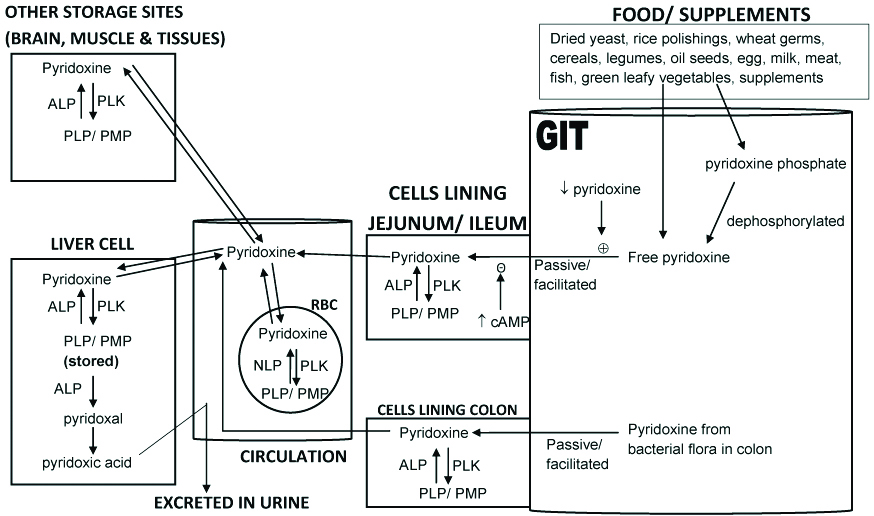
Absorption, metabolism, excretion: The summary of pyridoxine kinetics in the human body is illustrated in [Table/Fig-2]. Pyridoxine is mainly absorbed by passive diffusion in the jejunum. Small amounts are also absorbed in the ileum. Some studies suggests that the intestinal B6 absorbed by a non-saturable mechanism, whole other reports a specific acidic pH (but not Na+)-dependent carrier-mediated mechanism [15,18-21]. Intestinal absorption is regulated by extracellular as well as intracellular factors. A low vitamin level influences the extracellular regulatory factor causing a transcriptionally mediated up-regulation of intestinal pyridoxine absorption [20]. A Protein Kinase A (PKA) mediated pathway acts as the intracellular regulatory factor; where an increase in intracellular cAMP level leads to a significant decrease in the activity (and/or the number), but not affinity, of pyridoxine uptake [21]. In addition to the absorption of dietary B6 in jejunum and ileum, humans also absorb pyridoxine from the bacterial flora through an efficient mechanism for vitamin B6 uptake in the large intestine [19]. The vitamin is freely transported in the blood, primarily stored in the liver and lesser amounts are also stored in the muscle and brain [22]. In mammalian tissues, the Pyridoxal Kinase (PLK) enzyme catalyzes the phosphorylation of pyridoxine to its major coenzyme forms of vitamin B6, viz. Pyridoxal Phosphate (PLP) and Pyridoxamine 5’-Phosphate (PMP) (note that Pyridoxine Phosphate (PNP) produced from pyridoxine, is immediately converted to PLP). The vitamers of B6 readily diffuse across membranes, phosphorylation to PLP and PMP renders them poorly diffusible and essentially trapped in the cell, since their transport out of the cell requires dephosphorylation by enzymatic hydrolysis. Thus, PLK and the dephosphorylating enzymes of PLP are major factors that control the intracellular PLP concentrations [23,24]. Several nonspecific neutral or Alkaline Phosphatases (ALP) catalyse the dephosphorylation of the phosphorylated forms of vitamin B6 [24-26]. APL catalyses the conversion of PLP to pyridoxal in most tissues [27,28]. Alkaline phosphatase found in plasma metabolises a small fraction of plasma PLP [28,29]. In human erythrocytes, a neutral phosphatase, appears to be the enzyme primarily responsible for hydrolysing PLP [23]. B6 is metabolised in the liver to the metabolite 4-pyridoxic acid and excreted mostly as 4-pyridoxic acid in the urine. The t ½ of pyridoxine is 15 to 20 days [22].
Summary of pyridoxine metabolism in the human body.
↑ cAMP: increase in intracellular cyclic AMP; ↓ pyridoxine: decrease in extracellular pyridoxine; ⊕: activates; Θ: inhibits; PLP: pyridoxal phosphate; PMP: pyridoxamine phosphate; PLK: pyridoxal kinase; ALP: Alkaline phosphatase; NLP: Neutral phosphatase
Biochemical functions: The functions of PLP have been summarised in [Table/Fig-3]. The active functional group in pyridoxine is an alcoholic group. Pyridoxal phosphate, the coenzyme form is synthesised from pyridoxine by the enzyme pyridoxal kinase utilising Adenosine Triphosphate (ATP). About 70-80% of PLP is associated with glycogen phosphorylase activity and has a slow turnover; 20-30% is associated with amino acid metabolism and steroid hormone action, and has a rapid turnover [30]. PLP is believed to act as a phosphate buffer at the active site of glycogen phosphorylase [31]. It acts as a coenzyme for various enzymes associated with amino acid metabolism (transaminases, decarboxylases, serine hydroxymethyl transferase), heme synthesis (amino levulinic acid synthase or ALA synthase), niacin synthesis (kynureninase), and also in the formation of ceramide and sphingolipids. In all these reactions, the aldehyde group of PLP forms a Schiff base with the epsilon amino group of lysine residue of the apoenzyme [11].
Biochemical and signaling functions of pyridoxine.
PLP: Pyridoxal phosphate; PLK: Pyridoxal kinase; ALA synthase: Amino levulinic acid synthase
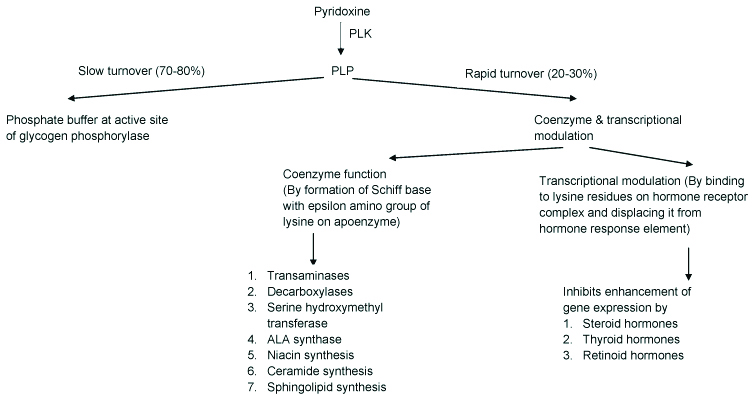
PLP inhibits enhanced gene expression by steroid hormones, vitamins A and D and thyroid hormones by binding to a lysine residue in the hormone receptor complex and displacing it from the hormone response element [12]. These findings were supported by Symes EK et al., Bowden JF et al., and Bender DA et al., studies in the years 1984, 1986 and 1987 respectively which have reported that B6 deficiency leads to accumulation of steroid hormones in the nucleus of target tissues [32-35]. Also, experimentally induced acute B6 depletion was found to produce two-fold increase in rate of expression of genes and addition of pyridoxal led to a decrease in gene expression [35-37].
Pyridoxine Levels in Pregnancy
In the recent years, there is a growing consensus that most pregnant women have some level of vitamin B6 deficiency compared to age matched non-pregnant women [38].
During pregnancy, plasma and erythrocyte pyridoxal 5’-phosphate (PLP) concentrations are altered in humans and laboratory animals [39-41]. In a study by Contractor SF and Shane B in the year 1970, both pyridoxal phosphate and pyridoxamine phosphate levels were found to be significantly lower in the blood of pregnant women as compared to non pregnant women. The pyridoxamine values were also lowered in both mother and fetus when compared with those in non pregnant women or men, but there was no difference in 4-pyridoxic acid or in pyridoxal values. Two hours after an oral load of pyridoxine hydrochloride, the values of pyridoxal 5’-phosphate in blood were lower in pregnant women in comparison to non-pregnant women. Higher levels of PLP were found in the cord blood than mother’s blood 3.5-10 hours after a pyridoxine hydrochloride load at delivery. The recovery of pyridoxal, pyridoxine and 4-pyridoxic acid (the main metabolite) following the oral load was similar in men, non pregnant women and pregnant women. Therefore it was concluded that the intestinal absorption was unimpaired during pregnancy and the relative deficiency of pyridoxal 5-phosphate was mainly because of the large fetal uptake and not due to metabolic changes in pyridoxine metabolism [42].
Neuroendocrine and Hormonal Factors Contributing to NVP/HG
Nausea and vomiting has been reported in about 50-90% of pregnancies [43]. In a study involving more than 360 pregnant women, nausea limited to the mornings was seen in 2% whereas 80% complained that nausea persisted throughout the day. The condition is usually self-limiting and the symptoms peaks at around 9 weeks of gestation and ceasing at 20 weeks. However, in about 20% cases, both the nausea and vomiting may continue until delivery and this condition is known as nausea and vomiting of pregnancy (NVP) or emesis gravidarum. As long as the affected female leads a normal life, this condition is not pathological [43,44]. In some females, however, it can take a more severe form called Hyperemesis Gravidarum (HG).
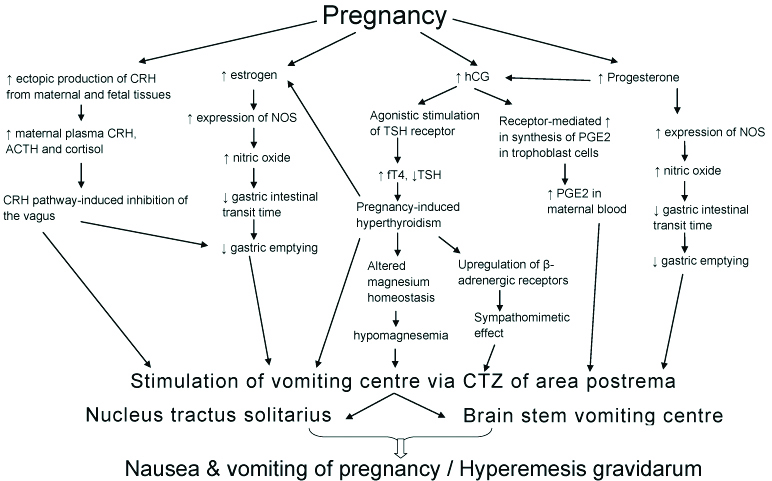
Although several factors are believed to contribute to NVP and hyperemesis in pregnancy the present review paper focuses only on the endocrine and hormonal factors [6]. The mechanism of action of pyridoxine as a therapeutic in NVP and pyridoxine is known to inhibit the enhancement of gene expression by steroid hormones. Among the hormonal factors, Human Chorionic Gonadotropin (hCG), progesterone, estrogen, Adrenocorticotropic Hormone (ACTH), cortisol, growth hormone and prolactin have been especially implicated in NVP [45]. These hormones are now well established in the list of circulating chemical agents that stimulate cells of the Chemoreceptor Trigger Zone (CTZ) of area postrema in the medulla oblongata, to initiate vomiting.
Based on the observation that the incidence of hyperemesis is maximum during the peak of pregnancy-induced increase of hCG (around 9 weeks gestation), hCG is considered to be the most likely endocrine factor for the development of HG [46]. The fact that some pregnant women do not experience nausea and vomiting despite elevated hCG-levels, can be explaned on the account of varying biological activity of different isoforms of hCG. An individuals’ sensitivity for emetogenic stimuli and hormone receptor interactions modify the effects of hCG leading to hyperemesis in some cases but not in others [47]. The different isoforms of hCG, isoforms without carboxy-terminal portion are short-acting but powerful stimulants of TSH and hyperglycosylated hCG isoforms are long-acting with respect to TSH receptor. Genetic and epigenetic factors attributes to different isoforms of hCG which explains the differences in HG incidence found in different populations and the variability in relationship between hCG and NVP [48,49]. Although the mechanism of emesis by elevated hCG is not well understood, Gadsby and Barnie-Adshead reported that the increased hCG levels causes a receptor mediated increase in PGE2 synthesis, resulting in elevated levels in maternal blood [50]. These findings suggest the role of PGE2 as the causative factor in NVP. Elevated, lowered as well as unaltered progesterone levels have been reported in patients with hyperemesis [51-54]. Increased plasma progesterone in hyperemesis-affected pregnant women is believed to cause a potentially emetogenic elevation of HCG [52]. Progesterone-induced reduced gastrointestinal motility and gastric dysrhythmias (tachygastria, bradygastria) during pregnancy are additional factors contributing to the observed hyperemesis [55,56].
Increased levels of estrogen and estradiol are known to cause nausea and vomiting in pregnancy The observation that oestrogen treatment can cause nausea supports its role in NVP. Conversely, women with hyperemesis seem to be more sensitive to oestrogen effects than asymptomatic pregnant women [52]. Walsh et al., reported that estrogen causes HG by inducing nitric oxide synthase that increasing the production of nitric oxide, that leads to smooth muscle relaxation, which slowes down gastric intestinal transit period and gastric emptying. The study also suggested that progesterone in combination with estrogen may also have a role in NVP since both hormones cause delayed gastric emptying to emetogenic levels [56].
Biochemical hyperthyroidism is prevalent in pregnancy especially in pregnant women with NVP or HG. Goodwin study reports a relationship between hCG and Transient Hyperthyroidism of Hyperemesis Gravidarum (THHG) [48]. Different mechanisms have revealed how hyperthyroidism can trigger vomiting. The first states that the thyroid hormones upregulates β-adrenergic receptors and causes an increase in β-adrenergic activity [57]. Thus, the vomiting in hyperthyroidism may be attributed to sympathomimetic effects of thyroid hormones. Second, it has been speculated that increased thyroid hormones per se can cause emesis by stimulating the CTZ [58]. Third, thyroid hormones alter magnesium homeostasis and the resulting hypomagnesemia affect smooth muscle directly or autonomic innervations of the upper GI smooth muscle [59, 60]. Fourth, since estrogen is increased in patients of both sexes with thyrotoxicosis the raised estrogen could explain the NVP in susceptible patients [58,61,62].
Maternal plasma CRH increases in pregnancy due to its ectopic origin from fetal as well as maternal tissues during pregnancy and a consequential and/or independent increase in plasma ACTH as well as plasma cortisol has also been reported [63]. This peripheral CRF pathway activation has been shown to stimulate inhibitory motor nerves in the dorsal motor nucleus of the vagus, thereby delaying gastric emptying and triggering emesis [64]. The same signal is also seen to trigger area postrema (AP) which is implicated in nausea and vomiting responses) suggesting that elevated peripheral CRF levels modulates the vomiting pathway [65, 66]. The roles of these hormones as causative factors in NVP are summarised in [Table/Fig-4,5].
Role of neuroendocrine and hormonal factors in etiogenesis of NVP/HG.
Maternal pyridoxine levels and pyridoxine administration in nausea and vomiting of pregnancy.
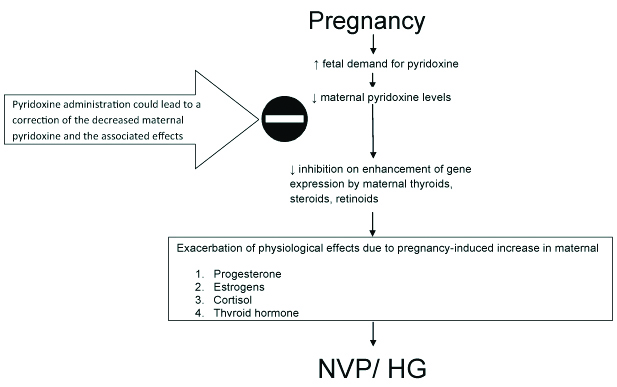
Pyridoxine-Mechanism of Action in NVP
Currently, the preventive/therapeutic role of pyridoxine in NVP is well accepted. In their review, Nuangchamnong and Niebyl described how NVP is often undertreated partly due to the fear of teratogenic effects of medications on the fetus during early pregnancy. They also gave historical review of the doxylamine-pyridoxine combination drug that obtained FDA approval as a delayed-release combination pill called Diclegis for the treatment of NVP and at present is the only FDA-approved medication for the indication of NVP. The re-introduction of Diclegis in American market filled up the therapeutic gap created due to removal of Bendectin used for the management of NVP. Based on extensive research, the authors proposed that this combination drug should be first-tier in the hierarchical approach to pharmacological treatment of NVP. Apart from the combination, pyridoxine alone can also be used in NVP [67].
Conclusion
Pyridoxine or vitamin B6, the water soluble vitamin of the B-complex group is therapeutically important in gynecology-in suppression of lactation, relieving depression and normalising glucose tolerance in women taking contraceptives, prevent etretinate induced development of fetal abnormalities and in relieving the symptoms of nausea and vomiting of pregnancy induced by increased fetal demand.
[1]. Marcus RG, Suppression of lactation with high doses of pyridoxineS Afr Med J 1975 49(52):2155-56. [Google Scholar]
[2]. Gupta T, Sharma R, An antilactogenic effect of pyridoxineJ Indian Med Assoc 1990 88(12):336-37. [Google Scholar]
[3]. Macdonald HN, Collins YD, Tobin MJ, Wijayarathne DN, The failure of pyridoxine in suppression of puerperal lactationBr J Obstet Gynaecol 1976 83(1):54-55.10.1111/j.1471-0528.1976.tb00730.x766822 [Google Scholar] [CrossRef] [PubMed]
[4]. Benninck HJ, Schreurs WH, Improvement of Oral Glucose Tolerance in Gestational Diabetes by PyridoxineBMJ 1975 (3):13-15.10.1136/bmj.3.5974.131131652 [Google Scholar] [CrossRef] [PubMed]
[5]. Jacobsson C, Granstrom G, Prevention of etretinate induced craniofacial malformations by vitamin B 6 in the ratEuropean Journal of Oral Science 1960 104(5-6):583-88.10.1111/j.1600-0722.1996.tb00145.x9021329 [Google Scholar] [CrossRef] [PubMed]
[6]. Noel ML, Saha S, Nausea and vomiting of pregnancyGastroenterol Clin North Am 2011 40(2):309-vii10.1016/j.gtc.2011.03.00921601782 [Google Scholar] [CrossRef] [PubMed]
[7]. Brown MJ, Beier K, Vitamin B6 deficiency (Pyridoxine)Statpearls (Internet) 2019 https://www.ncbi.nlm.nih.gov/books/NBK470579/ [Google Scholar]
[8]. Sahakian V, Rouse D, Sipes S, Rose N, Niebyl J, Vitamin B6 is effective therapy for nausea and vomiting of pregnancy: a randomized, double-blind placebo-controlled studyObstet Gynecol 1991 78(1):33-36. [Google Scholar]
[9]. Niebyl JR, Briggs GG, The pharmacologic management of nausea and vomiting of pregnancySupplement to the Journal of Family Practice 2014 63(2):S31-7. [Google Scholar]
[10]. Bender DA, Vitamin B6 requirements and recommendationsEur J Clin Nutr 1989 43(5):289-09. [Google Scholar]
[11]. Vasudevan DM, Vaidyanathan K, Sreekumari S, Textbook of biochemistry for medical students 2017 8th editionJaypee Brothers Medical Publishers (P) LtdISBN: 9789385999741 [Google Scholar]
[12]. Bender DA, Non nutritional uses of vitamin B6British Journal of Nutrition 1999 81(1):7-20.10.1017/S000711459900008210341670 [Google Scholar] [CrossRef] [PubMed]
[13]. Rollón N, Fernández-Jiménez MC, Moreno-Carralero MI, Murga-Fernández MJ, Morán-Jiménez MJ, Microcytic anemia in a pregnant woman: beyond iron deficiencyInt. J. Hematol 2015 101(5):514-19.10.1007/s12185-014-1723-725547425 [Google Scholar] [CrossRef] [PubMed]
[14]. Wrong OM, Edmonds CJ, Chadwick VS, The Large Intestine: its Role in Mammalian Nutrition and Homeostasis 1981 67(2)New YorkWiley and Sons:361-62. [Google Scholar]
[15]. Hamm MW, Hehansho H, Henderson LM, Transport and metabolism of pyridoxamine and pyridoxamine phosphate in the small intestineJ. Nutr 1979 109:1552-59.10.1093/jn/109.9.1552479950 [Google Scholar] [CrossRef] [PubMed]
[16]. Middleton HM, Intestinal absorption of pyridoxal-5′ phosphate disappearance from perfused segments of rat jejunum in vivoJ. Nutr 1979 109(6):975-81.10.1093/jn/109.6.975448455 [Google Scholar] [CrossRef] [PubMed]
[17]. Middleton HM, Uptake of pyridoxine by in vivo perfused segments of rat small intestine: a possible role for intracellular vitamin metabolismJ. Nutr 1985 115(8):1079-88.10.1093/jn/115.8.10794020487 [Google Scholar] [CrossRef] [PubMed]
[18]. Yoshida S, Hayashi K, Kawasaki T, Pyridoxine transport in brush border membrane vesicles of guinea pig jejunumJ. Nutr. Sci. Vitaminol 1981 27(4):311-17.10.3177/jnsv.27.3117328440 [Google Scholar] [CrossRef] [PubMed]
[19]. Said HM, Intestinal absorption of water soluble vitamins in health and diseaseBiochem J 2011 437(3):357-72.10.1042/BJ2011032621749321 [Google Scholar] [CrossRef] [PubMed]
[20]. Said ZM, Subramanian VS, Vaziri ND, Said HM, Pyridoxine uptake by colonocytes: a specific and regulated carrier-mediated processAm. J. Physiol. Cell Physiol 2008 294(5):C1192-97.10.1152/ajpcell.00015.200818353902 [Google Scholar] [CrossRef] [PubMed]
[21]. Said HM, Ortiz A, Ma TY, A carrier-mediated mechanism for pyridoxine uptake by human intestinal epithelial Caco-2 cells: regulation by a PKA-mediated pathwayAm. J. Physiol. Cell Physiol 2003 285(5):C1219-25.10.1152/ajpcell.00204.200312867360 [Google Scholar] [CrossRef] [PubMed]
[22]. Pyridoxine. Available from: http://www.drugs.com/ppa/pyridoxine-hydrochloride-b6.html (Accessed on 27/2/2015) [Google Scholar]
[23]. Lumeng L, Li TK, Vitamin B-6 metabolism in chronic alcohol abuseClin. Invest 1974 53(3):693-04. [Google Scholar]
[24]. Ebadi M, Catabolic pathways of pyridoxal phosphate and derivatives. In: Vitamin B-6. Pyridoxal PhosphateChemical, Biochemical, and Medical Aspects. Part B. (Dolphin, D., Poulson, R. & Avramovic, O., eds.) 1986 New YorkJohn Wiley & Sons:449-476.10.1172/JCI1076074359937 [Google Scholar] [CrossRef] [PubMed]
[25]. Lumeng L, Li TK, Characterization of the pyridoxal 5’-phosphate and pyridoxamine 5’-phosphate hydrolase activity in rat liverBiol. Chem 1975 250(20):8126-31. [Google Scholar]
[26]. Dorald T, Bachhawat BK, Purification and properties of brain alkaline phosphataseNeurochem 1977 29:503-512.10.1111/j.1471-4159.1977.tb10699.x19566 [Google Scholar] [CrossRef] [PubMed]
[27]. Anderson BB, O’Brien R, Grihfn GE, Mollin DL, Hydrolysis of pyridoxal 5’-phosphate in plasma in conditions with raised alkaline phosphataseGui 198 21(3):192-94.10.1136/gut.21.3.1927399318 [Google Scholar] [CrossRef] [PubMed]
[28]. Lumeng L, Schenker S, Li TK, Brashea RE, Compton MC, Clearance and metabolism of plasma pyridoxal 5’-phosphate in the dogLab. Clin. Med 1984 103(1):59-69. [Google Scholar]
[29]. Whyte MP, Mcalister WH, Patton LS, Magill HL, Falla N, Lorenz WB, Herrod HG, Enzyme replacement therapy for infantile hypophosphatasia attempted by intravenous infusion of alkaline phosphatase-rich Paget plasmaJ Pediatr 1984 105(6):926-33.10.1016/S0022-3476(84)80079-7 [Google Scholar] [CrossRef]
[30]. Coburn SP, Modeling vitamin B 6 metabolismAdv Food Nutr Res 1996 40:107-32.10.1016/S1043-4526(08)60023-6 [Google Scholar] [CrossRef]
[31]. Palm D, Klein HW, Schinzel R, Beuhner M, Helmreich EJ, The role of pyridoxal 59-phosphate in glycogen phosphorylase catalysisBiochemistry 1990 29(5):1099-07.10.1021/bi00457a0012182117 [Google Scholar] [CrossRef] [PubMed]
[32]. Symes EK, Bender DA, Bowden JF, Coulson WF, Increased target tissue uptake of, and sensitivity to, testosterone in the vitamin B 6 deficient ratJournal of Steroid Biochemistry 1984 20(5):1089-93.10.1016/0022-4731(84)90348-0 [Google Scholar] [CrossRef]
[33]. Bowden JF, Bender DA, Coulson WF, Symes EK, Increased uterine uptake and nuclear retention of [3H] oestradiol through the oestrous cycle and enhanced end-organ sensitivity to oestrogen stimulation in vitamin B 6 deficient ratesJournal of Steroid Biochemistry 1986 25(3):359-65.10.1016/0022-4731(86)90248-7 [Google Scholar] [CrossRef]
[34]. Bender DA, Oestrogens and vitamin B 6-actions and interactionsWorld Review of Nutrition and Dietetics 1987 51:140-88.10.1159/000414645 [Google Scholar] [CrossRef]
[35]. Allgood VE, Powell Oliver FE, Cidlowski JA, Vitamin B 6 influences glucocorticoid receptor-dependent gene expressionJournal of Biological Chemistry 1990 265:12424-33. [Google Scholar]
[36]. Allgood VE, Cidlowski JA, Vitamin B6 modulates transcriptional activation by multiple members of the steroid hormone receptor superfamilyJournal of Biological Chemistry 1992 267(6):3819-24. [Google Scholar]
[37]. Tully DB, Allgood VE, Cidlowski JA, Modulation of steroid receptor-mediated gene expression by vitamin B6FASEB J 1994 8(3):343-49.10.1096/fasebj.8.3.81439408143940 [Google Scholar] [CrossRef] [PubMed]
[38]. Raiten DJ, In: Vitamin B6 metabolism in pregnancy, lactation and infancy 1995 LondonCRC Press [Google Scholar]
[39]. Cleary RE, Lumeng L, Li TK, Maternal and fetal plasma levels of pyridoxal phosphate at term. Adequacy of vitamin B-6 supplementation during pregnancyAm J Obstet. Gynecol 1975 121(1):25-28.10.1016/0002-9378(75)90968-0 [Google Scholar] [CrossRef]
[40]. Lumeng L, Cleary RE, Wagner R, Yu PL, Li TK, Adequacy of vitamin B5 supplementation during pregnancy: A prospective studyAm J Clin Nutr 1976 29(12):1376-83.10.1093/ajcn/29.12.1376998549 [Google Scholar] [CrossRef] [PubMed]
[41]. Shane B, Contractor SF, Assessment of vitamin B6 status. Studies on pregnant women and oral contraceptive usersAm J Clin Nutr 1975 28(7):739-47.10.1093/ajcn/28.7.7391146727 [Google Scholar] [CrossRef] [PubMed]
[42]. Contractor SF, Shane B, Blood and urine levels of vitamin B6 in the mother and fetus before and after loading of the mother with vitamin B6American Journal of Obstetrics and Gynecology 1970 107(4):635-40.10.1016/S0002-9378(16)33952-7 [Google Scholar] [CrossRef]
[43]. Gadsby R, Barnie-Adshead AM, Jagger C, A prospective study of nausea and vomiting during pregnancyBr J Gen Pract 1993 43(371):245-48. [Google Scholar]
[44]. Mylonas I, Gingelmaier A, Kainer F, Nausea and vomiting in pregnancyDtsch Arztebl 2007 104(25):A-182. [Google Scholar]
[45]. Jueckstock JK, Kaestner R, Mylonas I, Managing hyperemesis gravidarum: a multimodal challengeBMC Medicine 2010 8:4610.1186/1741-7015-8-4620633258 [Google Scholar] [CrossRef] [PubMed]
[46]. Sheehan P, Hyperemesis gravidarum-assessment and managementAust Fam Physician 2007 36(9):698-01. [Google Scholar]
[47]. ACOG (American College of Obstetrics and Gynecology)Practice bulletin: nausea and vomiting of pregnancyObstet Gynecol 2004 103(4):803-14.10.1097/00006250-200404000-0004515051578 [Google Scholar] [CrossRef] [PubMed]
[48]. Goodwin TM, Hyperemesis gravidarumObstet Gynecol Clin Am 2008 35(3):401-17.10.1016/j.ogc.2008.04.00218760227 [Google Scholar] [CrossRef] [PubMed]
[49]. Jordan V, Grebe SKG, Cooke PR, Acidic isoforms of chorionic gonadotropin in European and Samoan women are associated with hyperemesis gravidarum and may be thyrotrophicClin Endocrinol 1999 50:619-27.10.1046/j.1365-2265.1999.00702.x10468928 [Google Scholar] [CrossRef] [PubMed]
[50]. Gadsby R, Barnie-Adshead AM, What causes the nausea and vomiting of pregnancy and hyperemesis gravidarum 2014 Semantic Scholarhttps://pdfs.semanticscholar.org/af12/2a6d0b46babccd0a97da17d8841f1745c2cc.pdf [Google Scholar]
[51]. Yoneyama Y, Suzuki S, Sawa R, Yoneyama K, Doi D, Otsubo Y, Araki T, The T-helper 1/T-helper 2 balance in peripheral blood of women with hyperemesis gravidarumAm J Obstet Gynecol 2002 187(6):1631-35.10.1067/mob.2002.12737312501075 [Google Scholar] [CrossRef] [PubMed]
[52]. Jarnfelt-Samsioe A, Nausea and vomiting in pregnancy: a reviewObstet Gynecol Surv 1987 42(7):422-27.10.1097/00006254-198707000-00003 [Google Scholar] [CrossRef]
[53]. Masson GM, Anthony F, Chau E, Serum chorionic gonadotrophin (hCG), schwangerschaftsprotein 1 (SP1), progesterone and oestradiol levels in patients with nausea and vomiting in early pregnancyBr J Obstet Gynaecol 1985 92(3):211-15.10.1111/j.1471-0528.1985.tb01084.x3872132 [Google Scholar] [CrossRef] [PubMed]
[54]. Lagiou P, Tamimi R, Mucci LA, Trichopoulos D, Adami HO, Hsieh CC, Nausea and vomiting in pregnancy in relation to prolactin, estrogens and progesterone: a prospective studyObstet Gynecol 2003 101(4):639-44.10.1097/00006250-200304000-0000612681864 [Google Scholar] [CrossRef] [PubMed]
[55]. Koch KL, Frissora CL, Nausea and vomiting during pregnancyGastroenterol Clin North Am 2003 32(1):201-34.10.1016/S0889-8553(02)00070-5 [Google Scholar] [CrossRef]
[56]. Walsh JW, Hasler WL, Nugent CE, Owyang C, Progesterone and estrogen are potential mediators of gastric slow-wave dysrhythmias in nausea of pregnancyAm J Physiol 1996 270:G506-14.10.1152/ajpgi.1996.270.3.G5068638718 [Google Scholar] [CrossRef] [PubMed]
[57]. Bilezikian JP, Loeb JN, The influence of hyperthyroidism and hypothyroidism on α- and β-adrenergic receptor systems and adrenergic responsivenessEndocr Rev 1983 4:378-88.10.1210/edrv-4-4-3786317368 [Google Scholar] [CrossRef] [PubMed]
[58]. Rosenthal FD, Jones C, Lewis SI, Thyrotoxic vomitingBr Med J 1976 2:209-211.10.1136/bmj.2.6029.209974494 [Google Scholar] [CrossRef] [PubMed]
[59]. Parkin AJ, Nisbet AP, Bishop N, Vomiting due to gastric stasis as the presenting feature in thyrotoxicosisPostgrad Med J 1981 57(668):40510.1136/pgmj.57.668.4057301693 [Google Scholar] [CrossRef] [PubMed]
[60]. Ballard B, Torres LM, Romani A, Effect of thyroid hormone on Mg(2+) homeostasis and extrusion in cardiac cellsMol Cell Biochem 2008 318(1-2):117-27.10.1007/s11010-008-9863-918604605 [Google Scholar] [CrossRef] [PubMed]
[61]. Wang KW, Mui KS, Thyrotoxic hyperemesis: a case reportSingapore Med J 1989 30:493-94. [Google Scholar]
[62]. Chopra IJ, Abraham GE, Chopra U, Solomon DH, Odell WD, Alterations in circulating estradiol-17 in male patients with Graves’s diseaseN Engl J Med 1972 286:124-29.10.1056/NEJM1972012028603035066598 [Google Scholar] [CrossRef] [PubMed]
[63]. Mastorakos G, Ilias I, Maternal and fetal hypothalamic-pituitary-adrenal axes during pregnancy and postpartumAnn N Y Acad Sci 2003 997:136-49.10.1196/annals.1290.01614644820 [Google Scholar] [CrossRef] [PubMed]
[64]. Taché Y, Martinez V, Million M, Wang L, Stress and the gastro intestinal tract III Stress-related alterations of gut motor function: role of brain corticotropin-releasing factor receptorsAm. J. Physiol. Gastrointest. Liver Physiol 2001 280(2):G173-G77.10.1152/ajpgi.2001.280.2.G17311208537 [Google Scholar] [CrossRef] [PubMed]
[65]. Maillot C, Wang L, Million M, Tache Y, Intraperitoneal corticotropin-releasing factor and urocortin induce Fos expression in brain and spinal autonomic nuclei and long lasting stimulation of colonic motility in ratsBrain Res 2003 974(1-2):70-81.10.1016/S0006-8993(03)02553-8 [Google Scholar] [CrossRef]
[66]. Wang L, Martinez V, Vale W, Tache Y, Fos induction in selective hypothalamic neuroendocrine and medullary nuclei by intravenous injection of urocortin and corticotropin-releasing factor in ratsBrain Res 2003 855(1):47-57.10.1016/S0006-8993(99)02200-3 [Google Scholar] [CrossRef]
[67]. Nuangchamnong N, Niebyl J, Doxylamine succinate-pyridoxine hydrochloride (Diclegis) for the management of nausea and vomiting in pregnancy: an overviewInt J Womens Health 2014 6:401-09.10.2147/IJWH.S4665324748822 [Google Scholar] [CrossRef] [PubMed]