Zinc has a vital role in cell growth, development, and is required to make Ribonucleic Acid (RNA) and Deoxy Ribonucleic Acid (DNA) for meiosis [2,3]. Thus, severe zinc deficiency affects the central nervous system that causes behavioural problems, decreased activity [4], decreased intelligence and impaired short-term memory and learning [5]. Acute zinc deficiency in human causes severe abnormalities in the sensory and behavioural performance of brain [6].
During pregnancy, serum copper concentrations increase with increasing gestational age, due to ceruloplasmin rise related to high oestrogen levels, which ensures high serum copper levels for both mother and baby [7,8]. Copper deficiency impairs the central nervous system and heart function with development. In some cases, even with replacement therapy, central nervous system complications such as hearing loss and decreased motor function may not be completely resolved [7].
Consequently, since zinc and copper are necessary in cell growth and having enough storage of these elements is of high importance in preterm or LBW neonates. The present study was designed to survey serum zinc and copper levels in the preterm neonates who have been admitted to the Neonatal Intensive Care Unit (NICU) and their relationship with type of nutrition, birth weight, and gestational age.
Materials and Methods
This cross-sectional study assessed 107 premature neonates with BWT <2500 gram that were hospitalised in neonatal intensive care unit of the affiliated hospital (tertiary service) to Shiraz and Jahrom University of Medical Sciences, Shiraz, Iran, from January 2014 to March 2016. The sample size estimation was based on a study by Abass RM et al., where the zinc level decreased from, 96% in the control group to 62% in the preterm neonate [7]. Considering α=0.05, Power=95%, P1=0.9, and P2=0.6, the sample size was calculated to be at least 104 patients.
The Ethics Committees of Shiraz and Jahrom University of Medical Sciences approved this study. The procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional or regional) and with the Helsinki Declaration of 1975 that was revised in 2000. All neonates were considered to be of appropriate birth weight for gestational age [9] The post-conceptional age was determined from the last menstrual period and confirmed by Dubowitz method [10].
Inclusion criteria were neonates with Gestational Age (GA) less than 37 weeks, BWT<2500 gram, and duration of hospitalisation more than 10 days. Neonates with positive inflammatory markers (C-reactive protein and Procalcitonin) and sign of infection were excluded from study. Since serum copper levels increase in inflammation, neonates with signs of inflammation or fever were excluded from the study. Furthermore, as serum levels of copper and zinc are affected by age, babies with age more than 10 days were enrolled in the study [11,12].
Exclusion criteria were the third-trimester supplementation with zinc and copper, supplementation with zinc and copper before or during hospitalisation, the infants with significant congenital anomaly or inborn error of metabolism, febrile infants, and infants of diabetic mother.
For estimation of zinc and copper level about 2-3 mL of venous blood was drawn from each neonate by an expert nurse and sent to the laboratory in disposable polypropylene tubes and after centrifuge, the serum stored in -40 degrees Centigrade, until use. Zinc and copper levels were measured using Flame-Atomic Absorption Spectrophotometry. All samples were examined in two replications.
Serum zinc and copper levels were compared with Very Low Birth Weight (VLBW) - BWT≤1500g - and LBW- BWT 1500-2500 g- neonates, also the levels were compared according to the type of feeding (breastfeed or formula-fed baby) and gestational age.
Before entering the study, informed consent was read and signed by the patients’ guardians.
Statistical Analysis
SPSS software (SPSS Inc., Version 17.0. Chicago: SPSS Inc.) was used to analyse the data of this study. The data were described by mean and standard deviation. Data analysis using a multiple linear regression analysis was used to estimate the association between independent variables. Pearson’s correlation coefficient (r) test was done for the correlation of parameters. The p-value less than 0.05 was considered statistically significant.
Results
This study involved 107 hospitalised neonates in the NICU who fulfilled the inclusion criteria; there were 63 (58.9%) males and 44 (41.1%) females.
The mean±SD of BWT, Age, and GA were 1914.8±361.2 grams, 14.2±3.1 days, and 32±1.6 week, respectively.
The mean±SD of GA in LBW (n=25) group and VLBW (n=82) group was 32.7±1.6 grams and 29.9±0.73 grams, respectively (p-value <0.001), and also 14.3±3.4 days and 13.9±2.1 days were the mean of age in mentioned groups respectively (p-value =0.57).
The mean±SD of plasma zinc level in LBW and VLBW groups were 83.9±17.1 μg/dL and 48.2±10.4 μg/dL, respectively (p-value <0.001). The mean±SD of plasma copper level in LBW and VLBW groups was 70.48±15.4 μg/dL and 82.7±12.03 μg/dL respectively (p<0.001).
The mean±SD of plasma zinc level in breastfed group (n=69) and formula-fed group (n=38) were 76.3±23.2 μg/dL and 74.2±19.4 μg/dL respectively (p-value=0.63). The mean±SD of plasma copper level in breastfed and formula-fed groups were 75.7±13.5 μg/dL and 74.9±15.9 μg/dL respectively (p-value=0.77).
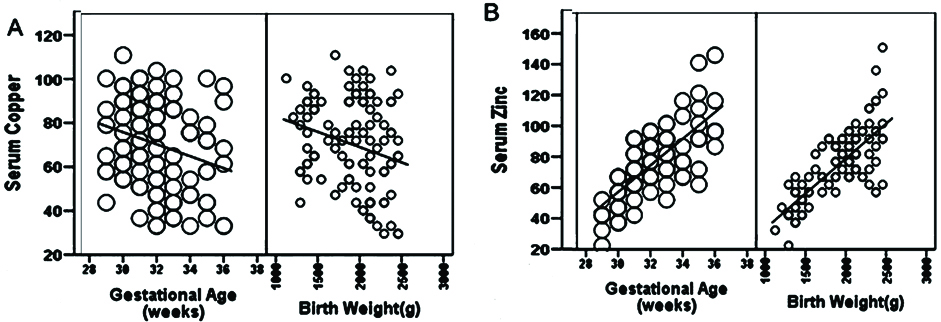
According to Pearson’s correlation test, serum copper had a significant negative correlation with neonatal BWT (r=-0.525, p-value <0.001) and GA (r=-0.572, p-value <0.001).
In addition, serum zinc showed a significant positive correlation with neonatal BWT (r=0.758, P=0.001) and GA (r=0.741, p-value=0.001). The regression variables of covariate distributions are shown in [Table/Fig-1a,b].
Regression variables of covariate distributions (GA and BWT) with serum copper (A) and zinc levels (B).
A multiple linear regression model was performed considering serum copper and zinc levels as dependent variables, and BWT groups (≤1500 and >1500), feeding type (breast fed, formula fed), and sex as independent variables. In this model, only BWT was determined as an independent influencing factor on serum zinc levels (R2=0.479, 95% confidence interval: 28.48-42.88, p=0.001) and serum copper level (R2=0.112, 95% confidence interval: -18.8 to -5.5, p=0.001) [Table/Fig-2].
Multiple linear regressions of covariates associated with serum copper and zinc levels.
| Parameters | R Square | df, F | Beta | B | 95% confidence interval | p-value |
|---|
| Serum copper | | | | | lower | upper | |
| BWT group | 0.112 | 1, 13.2 | -0.335 | 94.9 | -18.8 | -5.5 | 0.001 |
| Feeding type | 0.001 | 1, 0.079 | -0.027 | -0.821 | -6.61 | 4.94 | 0.779 |
| Sex | 0.001 | 1, 0.018 | -0.013 | -1.93 | - 6.02 | 5.25 | 0.893 |
| Serum zinc | | | | | | | |
| BWT group | 0.479 | 1, 96.57 | 0.692 | 35.68 | 28.48 | 42.88 | 0.001 |
| Feeding type | 0.002 | 1, 0.23 | -0.047 | -2.13 | -10.94 | 6.67 | 0.632 |
| Sex | 0.001 | 1, 0.053 | -0.023 | -1.0 | -9.57 | 7.57 | 0.818 |
BWT: Birth weight
Discussion
Zinc and copper are essential trace elements in preterm neonates [13]. Zinc is present in the foetus during the initial periods of intrauterine growth, and the relative concentration of zinc is constant during the development of the foetus. Almost 60% of the total embryonic zinc is obtained during the third trimester, while the embryonic weight is increased three times [12].
There were no statistically significant differences between LBW and VLBW group with respect to sex and age (p-value >0.05). However, there was a significant difference in respect to GA in both groups (p-value <0.05). This difference was expected because, in the studied patients, the gestational age was proportional to birth weight. The mean serum zinc levels in VLBW neonate were significantly lower than LBW (p-value <0.001). Therefore, it seems that the serum zinc level directly correlate with BWT in preterm neonate. As a result, low BWT (especially less than 1500 grams) is a risk factor for zinc deficiency. The mean serum copper level in VLBW neonate was higher than LBW but the differences statically were not significant (p-value =0.056). In the study of Kojima C, et al., the serum zinc and copper levels inversely correlated with GA and BWT [12]. They measured the serum level on the first day of life but in the present study, the serum levels of copper and zinc of neonate were estimated from the 10th day. The results are in contrast to the present study.
In this study, there was no significant relationship between feeding type (breast or formula) with zinc or copper serum level (p-value >0.05). The study by Mahmood T et al., showed that serum zinc level in breastfed neonate was lower than formula-fed neonate and determined that the low breast milk zinc levels achieved succeeding the first pregnancy may have been owing to immaturity of the milk [14]. Hemalatha P et al., observed that breastfed infants have a higher level of zinc compared to formula-fed infants because the colostrum of human breast-milk has higher zinc content [15].
Our study results revealed a negative correlation of serum copper level with neonatal BWT and GA (p-value<0.05), and positive correlation of serum zinc level with neonatal BWT and GA (p- value <0.05). Schneider JM et al., in a similar study did not find any significant difference between preterm and full-term neonates copper level [16]. Schulpis KH et al., presented that the copper levels in premature neonates were significantly lower than term neonates [17].
Regression variables of covariate distributions (GA and BWT) with serum copper and zinc levels showed that serum copper level was associated inversely with GA and BWT with statistically significant (p<0.05). Zinc level was associated directly with GA and BWT (p<0.05) [Table/Fig-2].
In the present study, the negative correlation of copper level with GA and LBW may be due to increased levels of estrogen in mother, subsequently increased ceruloplasmin, and finally cause increased copper level in neonate and mother as mentioned in the studies of Abass RM et al., and Uriu-Adams JY et al., [7,8].
Jyotsna S et al., confirmed that the mean serum zinc level was significantly lower in premature and LBW neonates [18].
Further studies may be needed to establish the guideline for zinc supplementations in normal and complicated pregnancy and in developed vs developing countries. It was found that there are differences between zinc level in complicated pregnancy and normal and developing vs developed countries [19,20].
Limitation
In the present study, it would have been better to correlate mothers’ serum zinc and copper level with their neonates, but it was not possible since our working centers were referral ones and there was no availability.
Conclusion
There was no association between feeding type (breast or formula) with neonatal zinc or copper serum level. Furthermore, serum zinc was found to be directly related to GA and LBW, but serum copper inversely correlated with GA and LBW with statistically significant difference.
BWT: Birth weight