Traumatic Fat Necrosis Complicated with a High Platelet Count and Anaemia in a Nigerian Neonate
Victor Idowu Joel-Medewase1, Risikat Opeyemi Qlaiya2, Olubukola Oluwayemisi Olusola-Adokayo3, Waheed Akanni Oluogun4
1 Consultant Paediatrician, Department of Paediatrics and Child Health, Ladoke Akintola University of Technology Teaching Hospitals, Ogbomoso, Oyo State, Nigeria.
2 Registrar, Department of Paediatrics and Child Health, Ladoke Akintola University of Technology Teaching Hospitals, Osogbo, Osun State, Nigeria.
3 Registrar, Department of Paediatrics and Child Health, Ladoke Akintola University of Technology Teaching Hospitals, Osogbo, Osun State, Nigeria.
4 Consultant Pathologist, Department of Pathology, Ladoke Akintola University of Technology Teaching Hospitals, Osogbo, Osun State, Nigeria.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Victor Idowu Joel-Medewase, Consultant Paediatrician, Department of Paediatrics and Child Health, Ladoke Akintola University of Technology Teaching Hospitals, Ogbomoso, Oyo State, Nigeria.
E-mail: vicmedjoel@yahoo.com
Traumatic fat necrosis is a rare, temporary and self-limiting condition. It is believed to be caused by panniculitis, or inflammatory change in fat tissues following trauma, cold or ischaemic insult. We report the case of a baby who presented with firm nodular bean seed sized swellings on both sides of the cheek and back, noticed 26 days after a difficult vaginal delivery. A platelet count of 461,000 cell/mm3 was recorded in the patient. The traumatic and haematological aberrations resolved spontaneously, after few weeks. We report the case to increase the awareness of health providers on the occurrence of such complications and to emphasise the need to promptly detect and manage them.
Neonatal, Panniculitis, Thrombocytosis
Case Report
A 26-day-old female baby, at the infant welfare clinic, reported with complaints of an insidious but progressive swelling of both cheeks noticed 5 days before presentation. The swellings had increased slowly and progressively from the size of a bean seed (about 0.5 cm) to almost double this size over five days. The swellings were not painful and the one on the left cheek was bigger in comparison to that on right. No redness was noticed around the swellings. The baby was well and fed well. She was neither febrile nor irritable. The mother was worried because the swellings had not resolved in 5 days [Table/Fig-1].
Showing raised indurated traumatic fat necrosis lesion on the right cheek.

Baby was born to a 27-year-old unbooked para 4 woman who was referred from a general hospital for caesarean section at 38 weeks +5 days on account of failed induction of labour, foetal distress and prolonged rupture of membranes. At delivery the baby had birth weight of 3.5 kg and she had moderate caput succedaneum with features of perinatal asphyxia. The Apgar scores were 21 35 710. The temperature was 37.0°C at admission to the neonatal unit and remained stable throughout her admission. The patient also had two episodes of hypoglycaemia which were corrected with 4 mls/kg of 10% dextrose in water administered as a bolus followed by maintenance dextrose infusion.
On further assessment, baby had features suggestive of hypoxic ischaemic encephalopathy (stage 2). This was managed according to hospital protocol. Baby had features suggestive of neonatal sepsis hence septic screen was done and started on intravenous Cefotaxime and Gentamycin. The results of the investigations done on day three are shown in [Table/Fig-2]. Platelet count was normal. The blood culture was negative after incubation for 72 hours. The electrolytes and urinalysis investigations, done during hospitalisation, were also normal. The baby was discharged to the neonatal clinic for follow up after 11 days of Hospital stay, following resolution of signs of perinatal asphyxia and neonatal sepsis. There was no sign of haemorrhage or thrombosis during stay of following discharge. However, the mother brought the baby back with complaints of localised facial swelling at age 26 days. Examination of the baby at 26 days of life revealed a well looking baby except for the nodular swellings on the malar area of the cheek and upper central portion of the trunk, posteriorly. A non-tender nodular mobile mass over both malar areas of the cheeks and a similar indurated mobile mass on the upper half of the posterior trunk were detected [Table/Fig-3].
| Day 3 | Day 26 | Day 42 | Reference values |
|---|
| PCV (%) | 42 | 20 | 23 | 42-65 |
| WBC (cells/mm3) | 27,000 | - | - | 9,000-30,000 |
| Neutrophil differential (%) | 24 | - | 32 | 66-78 |
| Lymphocyte differential (%) | 76 | - | 64 | 25-33 |
| Platelets (cell/mm3) | - | 461,000 | 148,000 | 150,000-350,000 |
| Calcium (mg/dL) | - | 9.6 | 8.2 | 8.4-10.4 |
| Phosphate (mmol/L) | - | - | 32 | 28-32 |
| Parathhormone (pg/mL) | - | - | 110 | 10-70 |
| Vitamin D3 (pmol/L) | - | - | 147 | 43-167 |
| Alkaline phosphatase (IU/L) | - | - | 390 | 124-341 IU/L |
| Urea (mmol/L) | - | 0.9 | 0.6 | 1.1-4.3 |
| Creatinine (umol/L) | - | 50 | 38 | 27-88 |
Showing raised indurated Traumatic fat Necrosis lesion on the back.

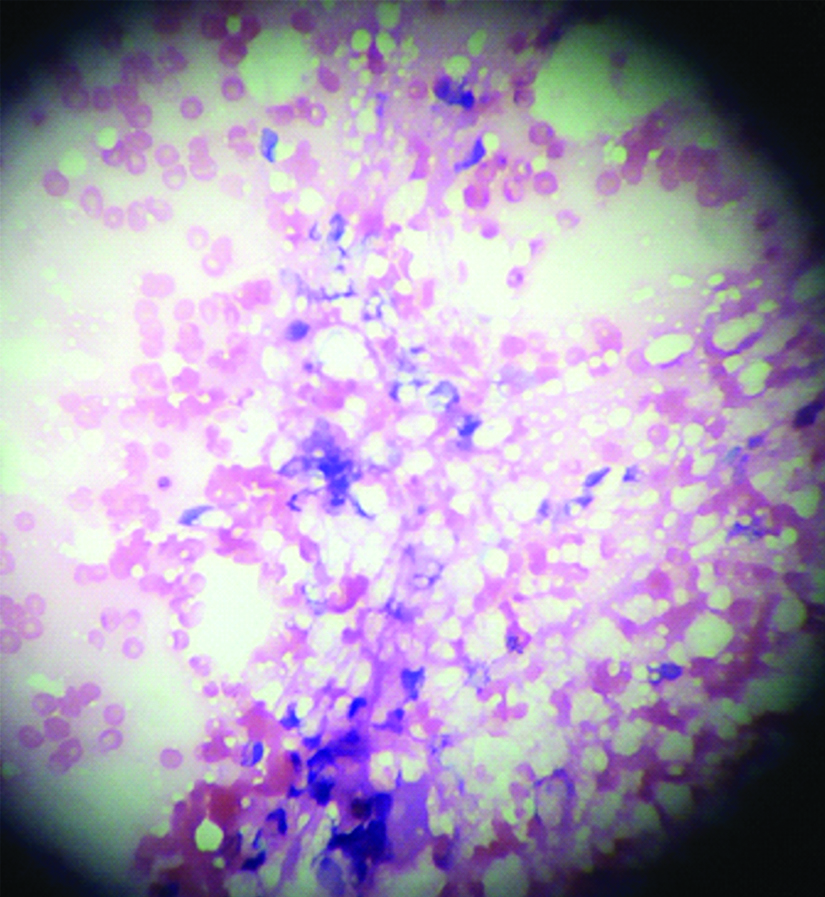
A fine needle aspiration and cytological examination of the aspirated tissue in the cheek revealed changes consistent with Traumatic Fat Necrosis (TFN). Microscopy showed lobules of adipocytes with eccentric nuclei and abundant clear cytoplasm. Admixed with the adipocytes were inflammatory cells mostly lymphocytes, neutrophils and histiocytes. Some clefts were located between the adipocytes and the background was haemorrhagic. The micrograph of the aspirated tissue is shown in [Table/Fig-4].
Photomicrograph of Fine Needle Aspiration Cytology (FNAC) of Traumatic Fat Necrosis (Haematoxylin and Eosin stain x40).
Black Arrow indicates Lobules of Matured adipocytes with eccentric nuclei and abundant clear cytoplasm
Blue Arrow shows Lymphocytes as part of the chronic inflammatory cells
Laboratory investigations for the electrolytes, hormone and haemtological indices assayed on day 42 of life at follow-up are shown in [Table/Fig-2].
The mother refused further blood investigations on the baby, despite counselling that child would need admission, close monitoring and a possible exchange transfusion to correct anaemia and thrombocytosis. She however consented to follow-up of the patient on out-patient basis. Currently, the infant is being followed up fortnightly and the TFN lesions have resolved.
Discussion
Necrosis of traumatised adipose tissue occurring around the period of birth is a temporary and self-limiting condition. In current case, the occurrence of lesions in the anatomical locations of the body with fat pads such as cheeks, buttocks and back are consistent with those of previous studies, which state that TFN occurs in term neonates with background histories of ischaemia, trauma and hypothermia; in similar anatomical locations [1-5]. Although the exact aetiology of TFN is unknown, it is speculated that our patient possibly suffered ischaemic and traumatic injury at birth judging from the low apgar scores and caput succedaneum. It is re-assuring that TFN can be prevented once the underlying risk factors are prevented. Hypothermia was not recorded in this neonate at presentation or during the peri-natal period.
The high prevalence of TFN predisposing factors, especially birth asphyxia and hypothermia, in the developing countries, makes it reasonable to presume that TFN may not be an uncommon condition in clinical practice in developing countries [2,6,7]. Short term problems associated with perinatal asphyxia and trauma includes seizures, hypoglycaemia and cerebral oedema, brachial plexus palsy and bleeding into tissues within and outside the skull [8]. Hypothermia on the other hand may lead to hypoglycaemia, acidosis and fatal illness outcome [9]. Other serious complications associated with TFN are hypercalcaemia, thrombocytopenia and anaemia [3-5,10,11].
Prevalence estimates of 20.8% and 2.7% have been documented for birth asphyxia and hypothermia respectively in a previous Nigerian report [12]. The paucity of reports on TFN in Nigeria may partly be due to missed cases or the under reporting associated with resource constrained areas. There are many location where birth asphyxia and hypothermia are still prevalent and at the same time, lack of health facilities or trained health workers. The babies born in such settings may not have the privilege of care by trained health workers proficient and competent enough to prevent the development of asphyxia or hypothermia, diagnose TFN and to report the same in medical literature.
Other aids necessary for prompt and accurate diagnosis of TFN include a high index of suspicion, knowledge of TFN, and anticipation of possibilities of developing TFN where risk factors such as perinatal asphyxia and foetal trauma at delivery exist [1-5]. The caput succedaneum is evidence of trauma to the skull, while the 3.5 kg weight of the child in relation to the size of the birth canal could put the baby at the risk of mechanical trauma while transiting the birth canal at delivery. Despite the fact that the baby was managed at a tertiary hospital and had two risk factors for TFN namely perinatal asphyxia and possible trauma resulting in marked caput succedaneum, the possibility of the baby developing TFN as a complication was not anticipated at or after birth. Even the mother was not informed of these developments. It was the mother who on noticing the tissue changes due to the TFN became worried and came to complain about them to the health providers.
Appropriate diagnosis and management are important, considering the fact that associated complications like hypercalcaemia and thrombocytopenia when present may prolong morbidity or lead to mortality [1-5]. The appropriate diagnosis of TFN in the present case put the maternal anxiety to rest and prevented further complications.
As a differential, erythema toxicum (urticarial of the newborn) can present with a rash which commonly appears in term babies between the ages of 2 and 10 days, much earlier than in the present case. They may look alarming and can be shown to contain platelet aggregates. They usually disappear spontaneously within a few days.
Thrombocytosis is a very rare complication of TFN and to our knowledge there is only one documented case of thrombocytosis with TFN [13]. A platelet count of 461,000 cell/mm3 was recorded in the case reported. Normal platelet count values range between 150,000-450,000 cell/mm3 while thrombocytosis is defined as a platelet count of 500,000 cell/mm3 and above [14]. It is therefore difficult to categorise the 461,000 platelet count in present report as normal or thrombocytosis. What is not controversial is that the platelet count is above the normal reference values.
It is worthy of note that the patient in the present report did not develop any of the feared complications of thrombocytosis (thrombosis and or haemorrhage). Reactive thrombocytosis is the most common cause of high platelet counts. The thrombocytosis is more likely to be due to TFN rather than neonatal sepsis considering that the patient had been treated for and recovered from the neonatal sepsis. The raised platelet count was therefore likely to be due to the TFN that she had sustained. A previous report has suggested that thrombocytosis could play a part in the pathogenesis of adipose tissue necrosis by causing lower blood perfusion in the presence of a background of relative hypoxaemia and hypothermia [13].
To examine for TFN in neonates or infants with risk factors for its development should be seen as wise action. Additional studies to determine the prevalence of TFN should be undertaken by way of deliberately examining the skin of newborns at birth and after birth at home by the mother.
[1]. Savic DM, Stojanovic ND, Stankovik VD, Stojkovic AK, Canovic DS, Ninkovik SM, Subcutaneous fat necrosis in NewbornsMed Glas (Zenica) 2012 9(2):429-31. [Google Scholar]
[2]. Chikaodinaka AA, Jude AC, Subcutaneous fat necrosis of the newborn: A case report of a term infant presenting with malaise and fever at age of 9 weeksCase Reports in Pediatrics 2015 2015:638962Available at http://dx.org/10.1155/2015/63896210.1155/2015/63896226635987 [Google Scholar] [CrossRef] [PubMed]
[3]. Feng Z, Guo B, Zhang Z, Subcutaneous fat necrosis of the newborn associated with hypercalcaemia after therapeutic hypothermiaJ La State Med Soc 2014 166(3):97-99. [Google Scholar]
[4]. Oliveira AC, Selores M, Pereira O, Fat necrosis of the newborn-A report of two casesAn Bras Dermatol 2011 86(4 Suppl 1):S114-17.10.1590/S0365-0596201100070003022068788 [Google Scholar] [CrossRef] [PubMed]
[5]. Verma SA, Bailey SM, Malley PV, Wachel EV, Subcutaneous fat necrosis and hypercalcaemia after therapeutic hypothermia in patients with hypoxic ischemic encephalopathy: A case seriesCureus 2018 10(7):e307410.7759/cureus.3074 [Google Scholar] [CrossRef]
[6]. Ekwochi U, Ndu IK, Nwokoye IC, Ezenwosu OU, Amadi OF, Osuorah D, Pattern of morbidity and mortality of new-born’s admitted into the sick and special care baby unit of Enugu State University Teaching Hospital, EnuguState: A five year reviewNig Q J Hosp Med 2011 25:255-61. [Google Scholar]
[7]. Olamijulo JA, Olaleye O, Perinatal mortality in Lagos University Teaching hospital: A five year reviewNig Q J Hosp Med 2011 21(4):255-61.Doi: 10.4013/1119-3077.130238 [Google Scholar]
[8]. Carlo WA, Nervous system disorders in Kliegman RM, Stanton BF, St. Geme JW, SchorNF, Behrman REIn Nelson’s Textbook of Pediatrics19th EdnPhiladelphia, U.SW.B Saunders Company:569-73. [Google Scholar]
[9]. Carlo WA, Neonatal Cold Injury in Kliegman RM, Stanton BF, St. Geme JW, Schor NF, Behrman REIn Nelson’s Textbook of Pediatrics19th EdnPhiladelphia, USW.B Saunders Company:622 [Google Scholar]
[10]. Lewis A, Cowen P, Rodda C, Dyall-Smith D, Subcutaneous fat necrosis of the newborn complicated by hypercalcaemia and thrombocytopeniaAustralas J Dermatol 1992 33(3):141-44.10.1111/j.1440-0960.1992.tb00102.x1303074 [Google Scholar] [CrossRef] [PubMed]
[11]. Varan B, Gurakan B, Ozbek N, Emir S, Subcutaneous fat necrosis of the newborn associated with anemiaPediatr dermatol 1999 16(5):381-83.10.1046/j.1525-1470.1999.00100.x10571839 [Google Scholar] [CrossRef] [PubMed]
[12]. Adebami OJ, Joel-Medewase VI, Oyedeji OA, Oyedeji GA, A review of neonatal admissions in Osogbo, Southwestern NigeriaNig Hosp Pract 2010 5(3):36-41.10.4314/nhp.v5i3-4.57848 [Google Scholar] [CrossRef]
[13]. Turba F, Bianchi C, Cella D, Rondanini GF, Thrombocytosis and neonatal subcutaneous adiponecrosisMinerva Pediatr 1994 46(7-8):343-46. [Google Scholar]
[14]. Weidmeier SE, Henry E, Burnett J, Anderson T, Christensen RD, Thrombocytosis in neonates and young infants: A report of 25 patients with platelet counts of or >1000000 micro(-l)J Perinatol 2010 30:222-26.Epub 2009 Oct 110.1038/jp.2009.14619798040 [Google Scholar] [CrossRef] [PubMed]