Blood Pressure (BP) measurement is a vital part of clinical practice and it is a commonly done physical examination. It is usually measured in one arm only and the readings thus obtained are used for various diagnostic and prognostic purposes. However, the practice of recording BP from both the arms is gaining attention especially with the current guidelines for the management of hypertension which recommend that since patients may have large difference (>10 mmHg) between arms, BP should be measured in both the arms and the arm with the higher value should be used for subsequent measurements [1]. Raised inter-arm BP difference has been associated with cardiovascular mortality and any difference ≥20/10 mmHg has been recommended to be taken seriously and referred to specialists [2,3]. Raised inter-arm systolic blood pressure is also associated with peripheral arterial disease [4].
PAD includes those disorders which result in the obstruction of blood flow in the arteries except in cerebral and coronary circulation [5]. It affects 12% of the general population and its incidence increases with age [6]. The all-cause mortality in patients with PAD is 4.8% which is higher than the all-cause mortality of patients without PAD which is 1.6% [7]. Cardiovascular mortality rate is almost five times higher in subjects with PAD when compared to subjects without PAD [8-10].
Most of the studies which assessed the relation between raised inter-arm BP difference and cardiovascular disease have been done in subjects with increased risk for cardiovascular disorder like people with hypertension and diabetes mellitus [4,11]. The difference in inter-arm BP has also been observed in general population but the studies to analyse its relation with PAD in general population without the presence of cardiovascular risk factors are scarce and so are the studies which related IAD with the presence and absence of symptoms for PAD. Such studies conducted in Indian population are little to none despite the increase in incidence. With this lacuna, we assessed the prevalence of inter-arm difference in SBP in people without any cardiovascular risk factor and related the inter-arm BP difference with both symptomatic and asymptomatic peripheral arterial disease.
Materials and Methods
Subject Selection
The study was conducted in the Department of Radiology and Physiology of a Private Medical College in Tamil Nadu, India. It was a comparative study with simple random sampling method. Study included 300 subjects of both the gender in the age group of 40-70 years who attended the out-patient department. The study was approved {06/mmchri/2016(A)} by Institute Ethical Committee and study was done during June 2016-May 17.
A detailed medical history was collected from all the subjects followed by thorough general examination. The medical history also included patient’s history of smoking, alcohol consumption and tobacco use. The symptoms of Peripheral arterial diseases like intermittent claudication, numbness of leg, non-healing wounds in the leg or foot were asked for and noted in the medical history. Subjects with any known history of diabetes mellitus, hypertension, chronic kidney disease or any endocrine disorder were excluded and a total of 260 participants were selected as participants. The purpose of the study was explained clearly in the local language (Tamil) and consent was obtained.
Blood Pressure Measurement
Blood pressure was measured for all the subjects after five minutes rest using OMRON digital BP monitors {Omron Healthcare Manufacturing Vietnam Company, Singapore}. BP was measured in both the arms consecutively with a minimum interval between the two readings of less than two minutes. Two readings were taken and the average of such reading was taken. Care was taken that the subjects were seated comfortably and neither the subject nor the observer talks during the measurement. The difference in SBP between the right arm and left arm measurements were calculated and the subjects were divided into the following groups based on their IAD SBP.
Group I (No IAD): IAD in SBP <10 mmHg
Group II: IAD in SBP >10 mmHg
Group II with significant IAD in SBP was further divided into three groups based on the level of IAD as follows: Group IIA, IIB and IIC with IAD SBP 10-15 mmHg, 15-20 mmHg, and >20 mmHg respectively. (Decided by authors)
Diagnosis of PAD
Non-invasive doppler scan was performed in all the subjects using ACUSON X300 (Siemens Medical Solutions, USA) for the diagnosis of peripheral arterial disease. All the subjects were enquired about the presence of symptoms of PAD like leg cramps, pain during ambulation, coldness in lower extremities, non-healing sores in toes, foot and legs and loss of hair in legs.
Statistical Analysis
All data were entered in MS Excel 2010 spreadsheet and analysis was done using SPSS software (version 21.0) and Sigmaplot software (version 6.01). Chi-square test was done to find the relation between IAD in SBP and PAD and odds ratio was calculated. Paired t-test was done to compare the mean difference in inter-arm SBP and independent sample t-test was done to compare the IAD in SBP between normal and PAD patients and for the comparison of IAD between PAD patients with and without symptoms. p-value of <0.05 was taken to be statistically significant.
Results
The average age of the participants was 50.6 years and out of the 260 subjects, 174 subjects (66.92%) had IAD in SBP below 10 mmHg and 86 subjects (33.08%) belonged to Group II with IAD in SBP above 10 mmHg. In Group II, 22, 45 and 19 subjects belonged to Group IIA, IIB and IIC respectively [Table/Fig-1].
Distribution of subjects based on IAD in SBP and diagnosis of PAD.
| Group | No. of subjects | PAD | No PAD |
|---|
| Group I | 174 | 12 | 162 |
| Group IIA (10-15 mmHg) | 22 | 15 | 7 |
| Group IIB (15-20 mmHg) | 45 | 42 | 3 |
| Group IIC (>20 mmHg) | 19 | 19 | 0 |
PAD: Peripheral arterial disease
Group I versus group II (IAD vs no IAD)
In Group I, i.e., subjects with IAD difference <10 mmHg, only 6.9 % (12 out of 172) had PAD. However, in Group II, i.e., subjects with IAD difference >10 mmHg 88.4% (76 out of 86) of patients with IAD had PAD [Table/Fig-1].
The odds ratio of patients with IAD to have PAD was 102.6 times higher than patients without IAD to have PAD {OR=102.6 (42.46– 247.94)} [Table/Fig-2].
Comparison of the risk of developing PAD with and without IAD in SBP.
| Odds ratio | 95% CI |
|---|
| Group I vs Group II (no IAD vs IAD) | 102.6 | 42.46–247.94 |
| Group IIA vs Group IIB (10-15 IAD vs 15-20 IAD) | 6.53 | 1.49–28.57 |
| Group IIB vs Group I (15-20 IAD vs no IAD) | 189 | 51–700.38 |
IAD: Inter-arm difference in systolic blood pressure; CI: Confidence interval
Group IIA vs Group IIB (10-15 IAD vs 15-20 IAD])
In Group IIA subjects, i.e., with IAD between 10-15 mmHg, 68.2% (15 out of 22) had PAD and in Group IIB, i.e., with IAD between 15-20 mmHg, 93.3% (42 out of 45) had PAD. The odds of group to had PAD was 6.53 times higher than patients with IAD10-15 to have PAD {OR=6.53 (1.49–28.57)} [Table/Fig-2].
Group IIC vs Group IIB (>20 IAD vs 15-20 IAD)
All the patients (100%) with IAD >20 mmHg had PAD. Since the number of subjects in Group IIC to not have PAD was zero, odds ratio was not calculated for this comparison.
Group IIB vs Group I (15-20 IAD vs no IAD)
The odds of patients with IAD15-20 mmHg to have PAD is 189 times higher than patients without IAD to have PAD {OR=189 (51–700.38)} [Table/Fig-2].
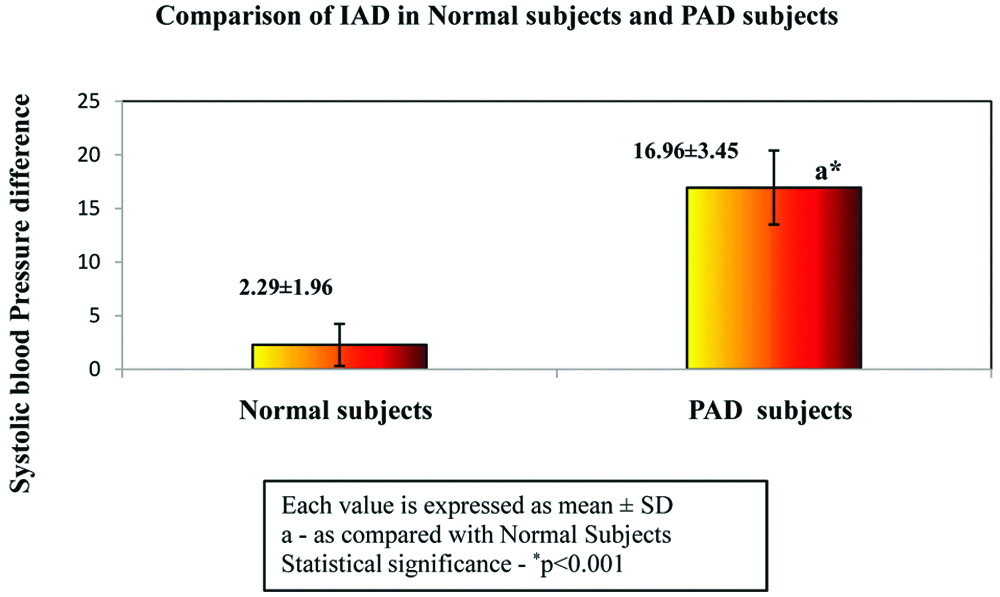
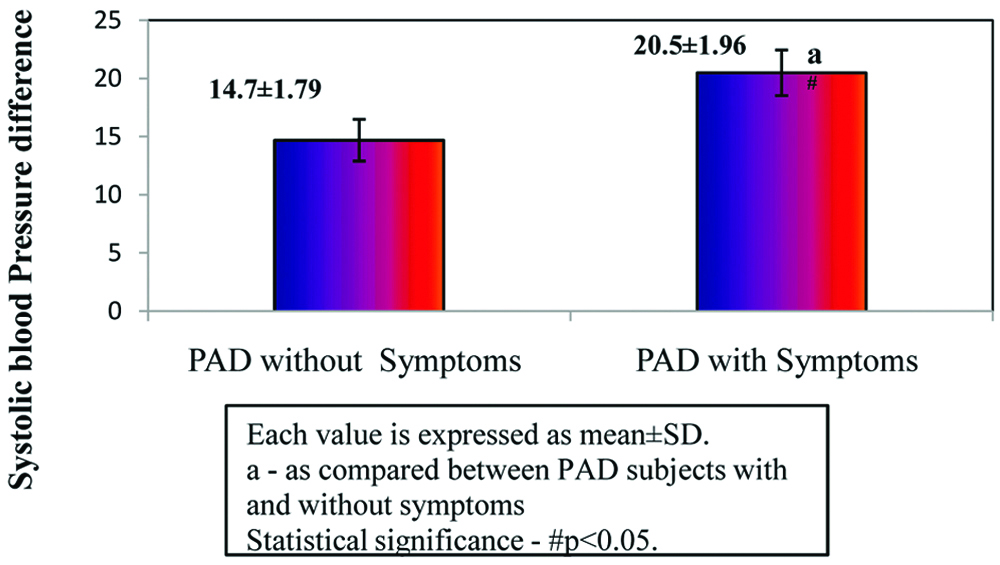
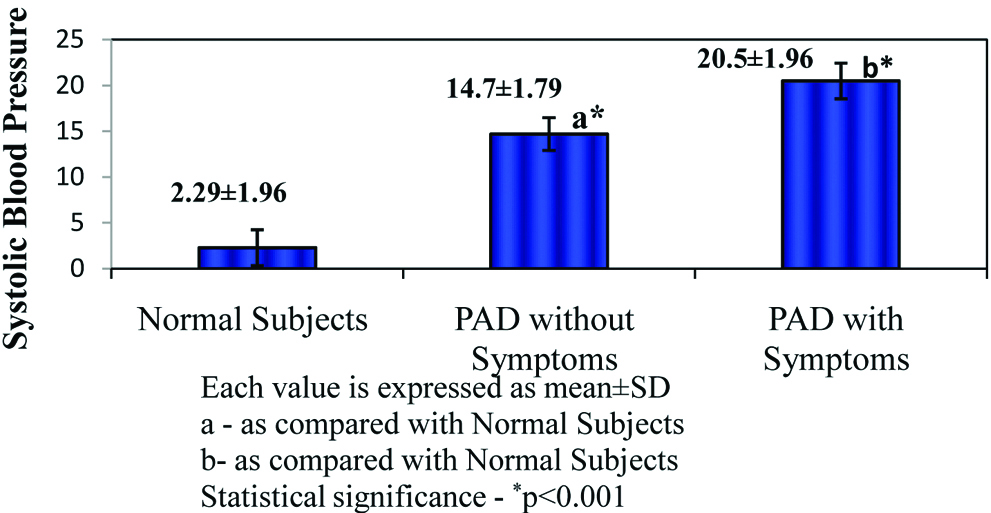
Comparison of IAD in normal subjects (n=12) and patients with PAD with and without symptoms (n=76).
The mean IAD in SBP was significantly higher in PAD patients when compared to normal subjects with a p<0.001 [Table/Fig-3]. Out of 76 PAD patients in Group II, 30 PAD patients were with symptoms and 46 patients were PAD without symptoms (39.48% and 60.52%, respectively) [Table/Fig-4]. The PAD patients with symptoms had significantly higher IAD in SBP when compared to PAD patients without symptoms (p-value<0.05) [Table/Fig-5]. The IAD in SBP was significantly higher in PAD patients with symptoms when compared with subjects without PAD (p-value<0.001) [Table/Fig-6].
Comparison of IAD in SBP in Normal subjects and PAD subjects.
PAD: Peripheral arterial disease; IAD: Inter-arm difference in systolic blood pressure
Distributions of patients with PAD presented with and without symptoms.
| Number of patients | Percentage |
|---|
| PAD with symptoms | 30 | 39.48% |
| PAD without symptoms | 46 | 60.52% |
| Total | 76 | 100.00% |
Comparison of IAD in SBP in PAD subjects with symptoms and without symptoms.
PAD: Peripheral arterial disease; IAD: Inter arm difference in systolic blood pressure
Comparison of IAD in SBP in Normal subjects, PAD subjects without symptoms and PAD subjects with symptoms.
PAD: Peripheral arterial disease; IAD: Inter-arm difference in systolic blood pressure
Discussion
An inter-arm difference in SBP >10 mmHg is defined as high IAD [12]. In the present study, with 50.6 years as the average age of the subjects, it was found that 33.08% (76) of the subjects had inter-arm SBP difference above 10 mmHg. Similar study by Harrison EG et al., found that high IAD in SBP was found in 5% of the subjects with the average age of 48 years [13]. Authors also found that out of the 76 subjects with high IAD, 88.4% were diagnosed with PAD. The risk of the patients with high IAD to have PAD in the present study was drastically higher than patients without IAD and so was the risk of patients with IAD between 15-20 mmHg to have PAD when compared to that of the patients without IAD. This is concomitant with the results of other studies which showed a positive relation between high IAD and incidence of PAD [2,14].
There are several risk factors for PAD including smoking, hypertension, diabetes mellitus and advanced age. In the present study, the subjects recruited were without a known history of hypertension and diabetes mellitus but despite that authors got high prevalence of PAD with 88 (33.85%) subjects out of which, 76 (29.23%) had high IAD and 12 (4.62%) had IAD less than <10 mmHg. This high prevalence could be attributed to the older age of the subjects in the present study with 50.6 years average. Similar findings have been shown by other studies which showed that the incidence of PAD increased with age [6,15].
Asymptomatic PAD is frequently present in the population and one of the alarming finding in the present study was that the 4.62% of the sample with no significant IAD who did not present with any symptoms of PAD were diagnosed with PAD in Doppler scan. The same happened to 60.52% of patients with high IAD who did not present with any PAD symptoms. Due to the lack of awareness about PAD, most of the frequent symptoms of PAD like leg cramps and pain during ambulation are neglected by the patients as they ascribe them to old age or physical exertion. The patient then tries to avoid exertion to prevent them from having those symptoms and they miss to report them to their physician [10]. Even in the present study, out of the 30 PAD patients who had symptoms, 20 patients failed to mention the PAD symptoms without prompting from the examiner. This can be prevented by increasing the awareness regarding PAD among the population which would help in earlier diagnosis and better management of the condition.
The IAD in SBP was significantly higher in PAD patients with symptoms when compared to PAD patients without symptoms and normal subjects. The studies which assessed the relation between inter-arm blood pressure difference and PAD did not include its relation with the absence of symptoms and little to none of such study has been conducted in Indian population. Since PAD can also be asymptomatic, this overlook is not desirable.
The diagnosis of PAD is aided by a non-invasive test which is ankle brachial pressure index but it is time consuming and is not a routinely followed physical examination procedure unlike BP measurement [16]. With the symptoms of PAD being commonly over looked by the patients, if BP measurement is done bilaterally in both the arms routinely in clinical practice, earlier diagnosis and management of PAD becomes possible. Unfortunately, this simple procedure is not done by the majority of the practitioners. A survey by Mc Kay CW et al., found that only 23% of the physicians recorded blood pressure in both the arms [17]. Awareness should be created that a simple procedure of bilateral BP measurement may save lives.
Limitation
The limitation of the study is that, the relationship between smoking history and the onset of peripheral arterial disease was considered. The BP measurement was done one time and continuous beat to beat. BP Measurement and its interarm difference over a time has to be considered in the larger population for better study implications.
Conclusion
The inter-arm systolic blood pressure difference is strongly related to peripheral arterial disease in the subjects of age group 40-70 years is high. Though, Inter-Arm Difference (IAD) was significantly more in Peripheral Arterial Disease (PAD) patients with symptoms than those without symptoms and normal subjects, a considerable amount of the PAD patients also presented without any symptoms. We urge the healthcare system to increase the awareness regarding the symptoms of PAD among the general population and also appraise the employment of blood pressure measurement in both the arms as a routine physical examination. An appreciation of the potential IAD in general population by the practitioners would be drastically beneficial for the patients and is also critical for accurate diagnosis and management of peripheral arterial disease.
PAD: Peripheral arterial disease