Impact of Periodontal Therapy in Patients with Sturge-Weber Syndrome
Iasminy Soares De Oliveira1, Teresa Cristina Esteves2, André Caroli Rocha3, Maria Das Graças Afonso Miranda Chaves4, Gisele Maria Campos Fabri5
1 DDS, Master, Department of Dentistry School, Federal University of Juiz de Fora, Juiz de Fora, Minas Gerais, Brazil.
2 MD, Master, Department of Medicine School, Federal University of Juiz de Fora, Juiz de Fora, Minas Gerais, Brazil.
3 DDS, PhD, Dental Division of Medical School, University of São Paulo, São Paulo, Brazil.
4 DDS, PhD, Department of Dentistry School, Federal University of Juiz de Fora, Juiz de Fora, Minas Gerais, Brazil.
5 DDS, PhD, Department of Dentistry School, Federal University of Juiz de Fora, Juiz de Fora, Brazil.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Gisele Maria Campos Fabri, Rua José Lourenço Kelmer s/n- São Pedro, Juiz de Fora– MGCEP- 36036-900, Juiz de Fora, Brazil.
E-mail: gisele.fabri@ufjf.edu.br
A 19 years old female patient, presented with the chief complaint of pain and swelling on her face. At physical examination, facial asymmetry and “port wine” spots on the left face were seen. Clinical examination: dental biofilm presence and dental calculus, spontaneous gingival bleeding, gingival hyperplasia, contour alteration and gingival tissue staining. Radiographic examination revealed radiolucent images and widening of the periodontal ligament space in the posterior region. This case emphasises the importance of dental follow-up of patients with Sturge-Weber Syndrome (SWS), demonstrating that careful periodontal treatment and orientation of oral hygiene care are fundamental to maintain the health and quality of life.
Angiomatosis, Gingival hyperplasia, Oral hygiene, Periodontal diseases
Case Report
A 19-year-old female patient, reported with the chief complaint of throbbing pain in her mouth and face. The pain was so intense prevented her from getting up in the morning and as consequence failed to attend her school regularly. When pain comes, she stays quiet in bed, takes some medicines, a determined episode. It was necessary to take morphine to relieve pain. She denied using anticonvulsants. The patient consulted so many (numbers of consulted dentists not reported) dentists who recommended oral antibiotics and oral hygiene techniques, but none of treatment relieved the pain. On taking medical history, her mother revealed that when she was child, she had recurrent seizures despite the fact that there were no alterations in imaging tests and subsequently was diagnosed with SWS.
On clinical examination, vascular malformation characterised by persistent macular erythema called port wine maculae, since she was born. Thus, oedema was noted on left side of her face which provoked facial asymmetry and labial angioma. The affected area was region of trigeminal innervation [Table/Fig-1]. Clinicians observed ocular prosthesis and they questioned the mother about this, according to her patient had the optic nerve affected by the syndrome as a child and use of the prosthesis was necessary. Intraoral examination revealed gingival overgrowth both palatally and labially in anterior and left posterior areas. The gingival condition was presented with reddish-purple colour, irregular and edematous contour with soft consistency. Furthermore, spontaneous gingival bleeding and presence of pockets in all vascular malformation intraoral area, dental calculus and abundant dental biofilm were observed [Table/Fig-2,3,4 and 5]. After examination, provisional diagnosis was established as chronic periodontal disease associated with vascular malformation.
Appearance in the first appointment presenting nevus flammeus and edema on left side of the face.

Intraoral view shows gingival edema, dental calculus and abundant dental biofilm on the affected side.

Intraoral view showing gingival edema, dental calculus and abundant dental biofilm on the unaffected side.

Occlusal view showing difference in the gingival volume of the affected side to the normal side.

Occlusal view showing gingival tissue covering the coronary portion of the involved teeth.

The treatment was administered during biweekly appointments and treatment plan consisted of the removal of dental calculus through conventional periodontal therapy, paying attention to the vascular behaviour of site that was normal during the procedures. A protocol of oral hygiene was instituted, and clinical periodontal therapy was planned. Supra and subgingival root scaling and teeth polishing were performed, using ultrasonic scalers (Profit III Bios, Dabi Atlant) and hand instruments. All treatment were administered under local anaesthesia. In addition, laser therapy (Photon Lase III- PL7336, DMC) was applied at a 90° angle to a gingival and non-tissue contact surface (660 nm, 50 mW, 4 J/cm 2, 90 seconds) in all appointment.
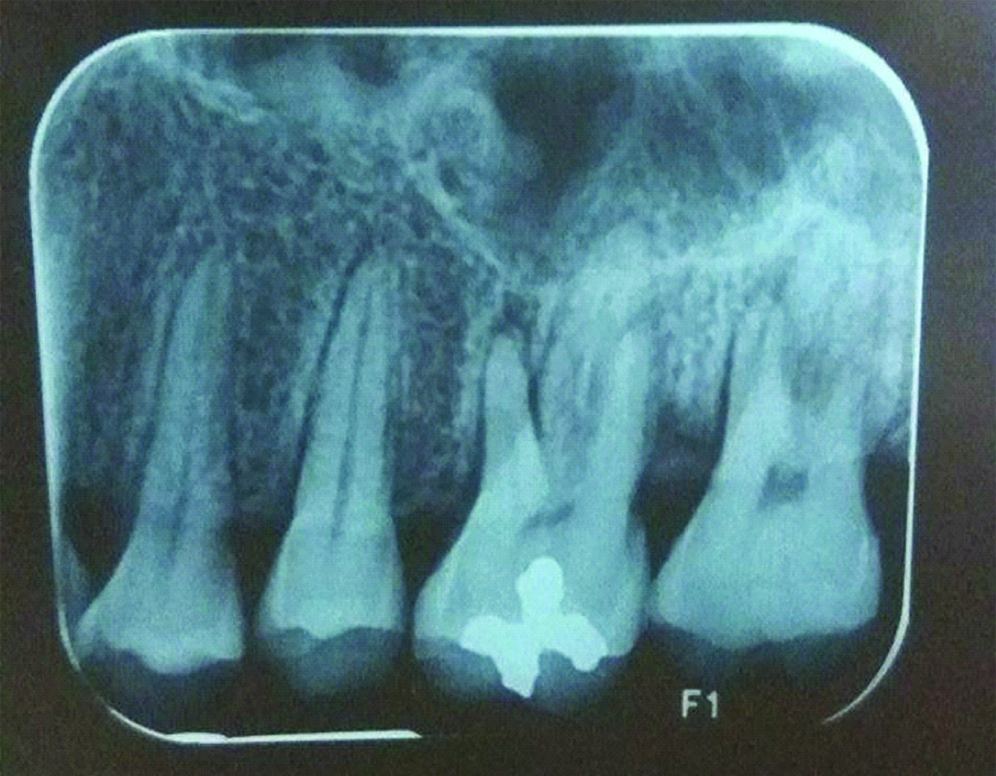
Radiographic examination showed loss of periodontal attachment, widening of periodontal ligament space and changes in bone density in the posterior region of the affected maxilla [Table/Fig-6].
Periapical radiograph of the area affected by vascular malformation.
The patient was reevaluated one month after the periodontal treatment period and achieved complete pain relief. There was reduction in swelling and the colour of the gingival tissue was normalised [Table/Fig-7,8]. So, patient made periodic follow-up visits for every three months.
Buccal aspect after periodontal treatment after one month follow-up.

Labial view after periodontal treatment after one month follow-up.

Discussion
Sturge-Weber Syndrome (SWS) is part of the vast group of diseases classified as phacomatoses or hamartomatosis defined by the established triad: meningeal, cutaneous and visual hemangiomas [1]. Notwithstanding its typical presentation, incomplete forms are common [1]. The most common alterations are: intracranial calcifications, affecting cortical parieto-occipital areas, angioma reinforcement after contrast administration and atrophy [2]. Although it is congenital, no pattern of heredity has been established and there is no predilection for race or sex [3,4]. It has an incidence of 1 /50,000-1/230,000 live births [5,6]. Medical treatment in patients with SWS includes anticonvulsants, symptomatic and prophylactic treatment for the headache, glaucoma treatment to reduce intraocular pressure and laser therapy for la Mancha vinho do porto [7]. Other similar cases showed patients with oral complications and chief complaints of swollen, bleeding gums and dental calculus on the teeth. On extraoral examination of these cases, as the present case, port wine stains on side of the face and facial asymmetry were observed [8,9].
The present case of SWS demonstrated significant aspects of dental professional knowledge and approach. The patient showed serious dental complaint which compromised her daily activities. On clinical examination, authors observed increasingly exacerbated gingival volume, intense accumulation of dental calculus, proliferation of blood vessels throughout the left maxilla and cheek on the same side. She presented the port-wine stain affecting the middle and lower thirds of her right cheek, which can increase in size with age and does not usually regress spontaneously [10]. It has already been described that oral manifestations are presented in approximately 40% of the cases and the most common feature is an angiomatous gingival lesion, usually restricted to the ipsilateral side of the jaw, floor of the mouth, lips, palate, tongue, and buccal mucosa ending abruptly at the midline [11-13]. This overgrowth not only causes discomfort and deformity but leads to poor hygiene and greater susceptibility to oral and systemic infections [12,14]. Plaque control is imperative to maintain oral health and to minimise adverse factors related to periodontal tissues [12].
The radiographic examination showed loss of periodontal insertion, periodontal ligament enlargement and changes in bone density in the posterior region of the affected maxilla. This condition may lead to loss of the elements involved [14], more specifically the molars that already had bone loss, when associated with poor oral hygiene. Confronted with this possibility and the difficulty of rehabilitation of this area, it is essential to maintain these elements. Patients with SWS may have difficulty in performing oral hygiene and in chewing due to vascular changes caused by the syndrome. This condition may predispose the patient to local and systemic infections [12,14].
In the first assessment, it was observed increasingly exacerbated gingival volume, colour change, alteration in contour and texture of gingival tissue with intense accumulation of dental calculus. Immediate prophylaxis with ultrasound (Profi III Bios, Dabi Atlant) and instructions about oral hygiene. A dental education on oral hygiene practices and as a preventive strategy should be notified, as was done in this case [8]. Plaque control is imperative to maintain oral health and to minimise adverse factors related to oral hygiene in periodontal tissues [12].
Clinical periodontal treatment was administered during biweekly appointments. Case follow-up resulted in an improvement of periodontal health. The results showed a reduction in gingival volume that generated relief in pain and improved quality of life. However, continuous periodontal treatment is required to reduce gingival inflammation and avoid the need for invasive surgical techniques [15].
In this case report, the laser therapy was associated with a periodontal therapy aiming to speed up the process of healing. Studies have shown that laser therapy is an effective treatment for relieving post-operative pain and reducing oedema by accelerating healing and ensuring the quality of life for post-treatment patients [16].
Conclusion
To conclude, this case emphasises the need for adequate and planned intervention in this patient profile, due to the associated gingival vascular characteristics and complicated manifestations. Periodic oral assessments and maintenance of good oral hygiene help to prevent any complications of oral changes and ensure the quality of life for patients with Sturge-Weber syndrome.
[1]. Aylett S, Sturge-Weber syndromeAnnals of Indian Academy of Neurology 2007 10:55-58.10.4103/0972-2327.31489 [Google Scholar] [CrossRef]
[2]. Rastogi S, Lee C, Salamon N, Neuroimaging in pediatric epilepsy: a multimodality approachRadiographics 2008 28(4):1079-95.10.1148/rg.28407511418635630 [Google Scholar] [CrossRef] [PubMed]
[3]. Evans AL, Widjaja E, Connolly DJ, Griffiths PD, Cerebral perfusion abnormalities in children with Sturge-Weber syndrome shown by dynamic contrast bolus magnetic resonance perfusion imagingPediatrics 2006 117(6):2119-25.10.1542/peds.2005-181516740855 [Google Scholar] [CrossRef] [PubMed]
[4]. Patrianakos TD, Nagao K, Walton DS, Surgical management of glaucoma with the Sturge Weber syndromeInt Ophthalmol Clin 2008 48(2):63-78.10.1097/IIO.0b013e318169358218427262 [Google Scholar] [CrossRef] [PubMed]
[5]. Maraña Pérez AI, Ruiz-Falcó Rojas ML, Puertas Martín V, Domínguez Carral J, Carreras Sáez I, Duat Rodríguez A, Analysis of Sturge-Weber syndrome: A retrospective study of multiple associated variablesNeurologia 2017 32(6):363-70.10.1016/j.nrl.2015.12.01226964511 [Google Scholar] [CrossRef] [PubMed]
[6]. Pascual Castroviejo I, Síndrome de Sturge Weber, En: Pascual Castroviejo I, editor. Diagnóstico clínico-radiológico en neurología infantil 1971 BarcelonaEd. Científico-Médica:81-87. [Google Scholar]
[7]. Higueros E, Roe E, Granell E, Baselga E, Sturge-Weber Syndrome: A ReviewActas Dermosifiliogr 2017 108(5):407-17.10.1016/j.ad.2016.09.02228126187 [Google Scholar] [CrossRef] [PubMed]
[8]. Nidhi C, Anuj C, Sturge Weber Syndrome: An Unusual Case with Multisystem ManifestationsEthiop J Health Sci 2016 26(2):187-92.10.4314/ejhs.v26i2.1327222632 [Google Scholar] [CrossRef] [PubMed]
[9]. Neerupakam M, Reddy PS, Babu BA, Krishna GV, Sturge Weber Syndrome: A Case StudyJ Clin Diagn Res 2017 11(5):ZD12-ZD14.10.7860/JCDR/2017/25593.989128658923 [Google Scholar] [CrossRef] [PubMed]
[10]. Amaral APB, Souza KL, Pereira CM, Síndrome de Sturge-Weber: revisão da literaturaNeurobiologia 2008 71(1-2):53-64. [Google Scholar]
[11]. Manivannan N, Gokulanathan S, Ahathya RS, Gubernath , Daniel R, Shanmugasundaram , Sturge-Weber syndromeJ Pharm Bioallied Sci 2012 4:349-52.10.4103/0975-7406.10030423066288 [Google Scholar] [CrossRef] [PubMed]
[12]. Pagin O, Del Neri NB, Battisti MPL, Capelozza AL, Santos PS, Periodontal manifestations and ambulatorial management in a patient with Sturge Weber syndromeJ Craniofac Surg 2012 23(6):1809-11.10.1097/SCS.0b013e318271016c23147344 [Google Scholar] [CrossRef] [PubMed]
[13]. Pithon MM, de Andrade AC, de Andrade AP, dos Santos RL, Sturge-Weber syndrome in an orthodontic patientAm J Orthod Dentofacial Orthop 2011 140(3):418-422.10.1016/j.ajodo.2009.10.04921889087 [Google Scholar] [CrossRef] [PubMed]
[14]. Bhansali RS, Yeltiwar RK, Agrawal AA, Periodontal management of gingival enlargement associated with Sturge-Weber syndromeJ Periodontol 2008 79(3):549-555.10.1902/jop.2008.06047818315439 [Google Scholar] [CrossRef] [PubMed]
[15]. Suprabha BS, Baliga M, Total oral rehabilitation in a patient with portwine stainsJ Indian Soc Pedod Prev Dent 2005 23(2):99-102.10.4103/0970-4388.16452 [Google Scholar] [CrossRef]
[16]. Merigo E, Vescovi P, Margalit M, Ricotti E, Stea S, Meleti M, Efficacy of LLLT in swelling and pain control after the extraction of lower impacted third molarsLaser Ther 2015 Mar 31 24(1):39-46.10.5978/islsm.15-OR-0525941424 [Google Scholar] [CrossRef] [PubMed]