Among the contraceptive methods available, IUCD’s seems to be the most acceptable, effective, extensively used long-acting reversible and the best cost-effective method of contraception [1]. With the increased use and availability of IUCD’s, the number of related problems is also increasing. It is associated with certain problems like irregular vaginal bleeding, menorrhagia, lower abdominal pain, pelvic inflammatory disease, ectopic pregnancy and very rarely some dangerous problems like uterine perforation and transmigration of IUCD to near by organs [2,3].
The most common problem reported is missing thread and that can be the indication of the potential problems like accidentally expelled IUCD, torn-off or retracted IUCD, malpositioned IUCD (abnormal location within the uterus and partially/completely embedded in the uterine myometrium) [4] or transmigrated IUCD (extrauterine location) [1]. The incidence of misplaced IUCD due to uterine perforation varies and is approximately 0.3-2.6/1000 insertions [5-7]. Transmigration of IUCD to the pouch of Douglas, mesentry, bladder, colon, omentum, rectum and ureter has been reported in the literature [8-13].
Its incidence is affected by multiple factors like parity, the timing of IUCD insertion, the position of the uterus, previous history of abortions, lower segment cesarean section or other cervical surgeries, type of IUCD and provider experience [14]. Chances of perforation of uterus are maximum at the time of insertion of IUCD [15]. The mechanism of transmigration was explained by multiple theories and which importantly includes faulty insertion technique and chronic inflammatory process due to the copper content of the IUCD which leads to the erosion of the wall of the uterus and resultant transmigrated IUCD [16]. The Copper content of the copper containing IUCD lying in the abdominal cavity causes massive tissue response and leads to further complications [17].
The Minimally invasive surgery appears to be the diagnostic as well as a therapeutic technique for the safe removal of dislocated IUCD’s. This study was designed to find out the incidence of dislocated IUCD requiring operative intervention and to study common clinical presentation, investigations required and the preferred surgical method for its retrieval.
Materials and Methods
This was a retrospective study, conducted in the Department of Obstetrics and Gynaecology in a medical college over a period of two years from June’ 2016 to June’ 2018. Total 20 patients with dislocated IUCD in whom surgical intervention was required for the retrieval of IUCD were recruited. Case records from the Medical Record Department and Family Planning Unit of the institution were analysed.
Data were entered in a pre-designed performa which included detailed demographic profile, clinical presentation, type of IUCD, time of insertion, duration of IUCD in situ examination findings, investigations required to localise the IUCD, surgical procedure required and intraoperative findings. Data were also reviewed on the use of pelvic ultrasonography and/or abdominal X-ray to diagnose the condition and to find out the exact position of IUCD.
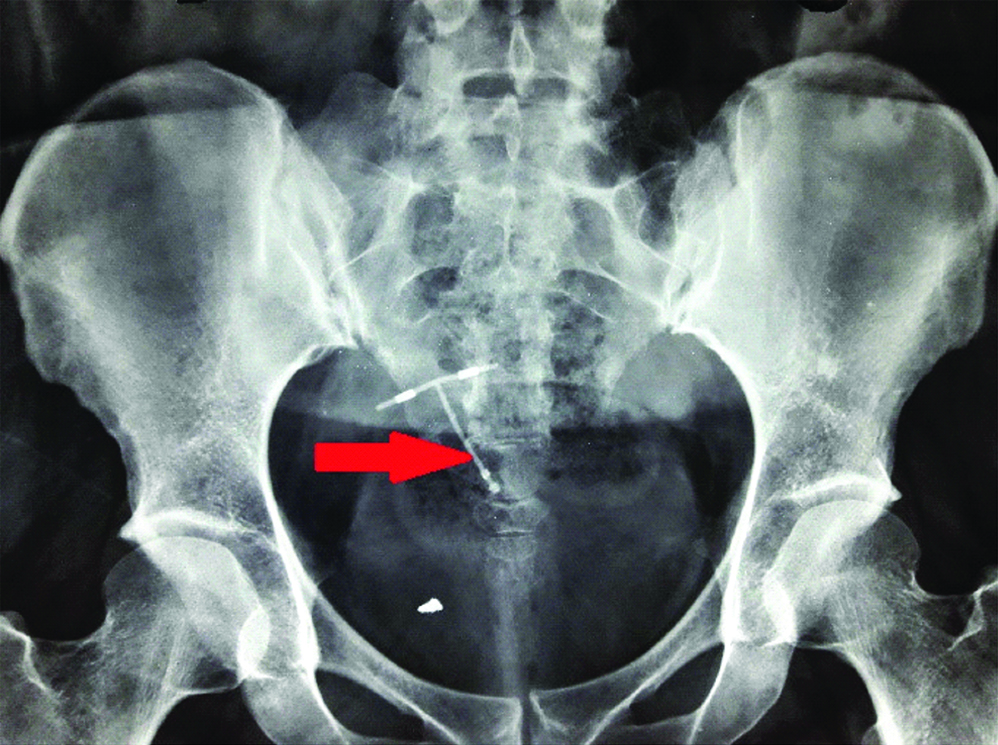
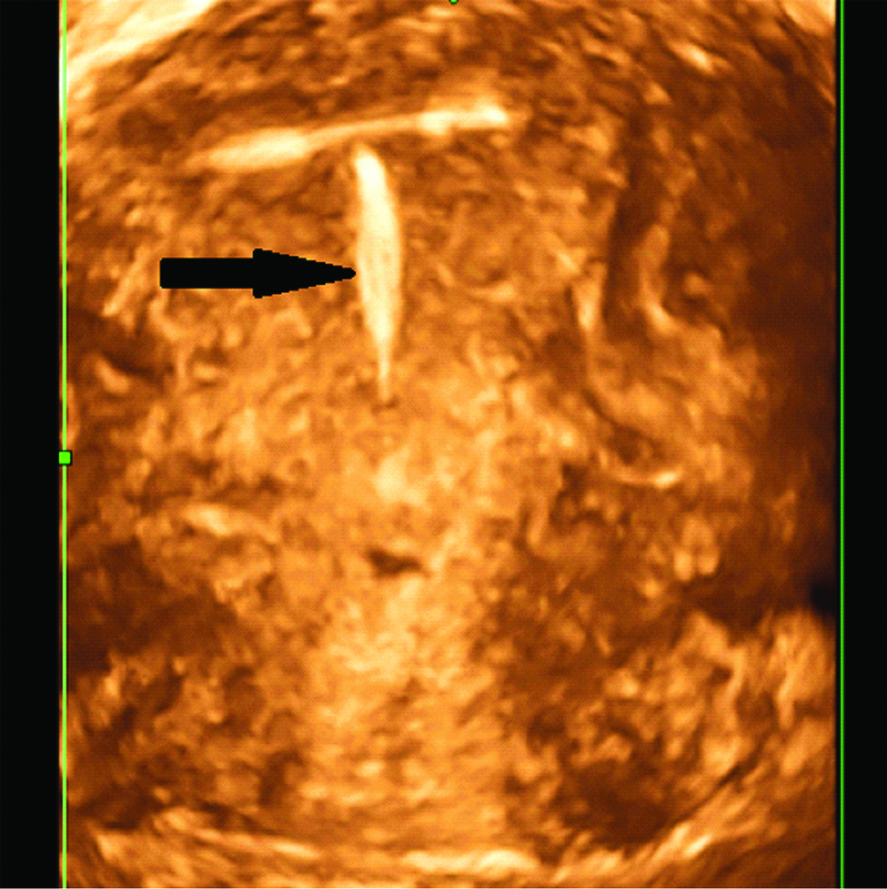
In general, patients were subjected to ultrasonography pelvis (2D/3D) and plain X-ray abdomen/pelvis (If required) to confirm the presence and to localise the IUCD, before planning the surgical procedure (hysteroscopy or laparoscopy/laparotomy) [Table/Fig-1,2].
Plain X-ray Abdomen showing IUCD in the pelvic region (oblique position).
A 3D USG showing IUCD within the uterine cavity.
Statistical Analysis
Data entry and statistical analysis were done using the Statistical Package for the Social Sciences (SPSS) version 17.0. The analysis was done in the form of percentages and proportions and represented as tables wherever necessary.
Results
Total 20 patients were included in the study. Mean age was 27.5 (22-35) years and parity ranged from 1-3. Patients were comparable with regards to age and parity. An 85% (17/20) patients had CuT 380 A and 15% (3/20) had multiload type of IUCD. An 80% (16/20) IUCD were inserted in postpartum phase and 20% (4/20) as an interval IUCD. Among postpartum IUCD (16/20), 10 were inserted immediately post-placental after normal vaginal delivery and 6 were inserted at the time of cesarean section. X-ray abdomen was done only in 3 cases with misplaced/transmigrated IUCD and ultrasonography pelvis was done in remaining 17 cases. Four patients with malpositioned IUCD (4/17) already got X-ray abdomen done before they came to this institute.
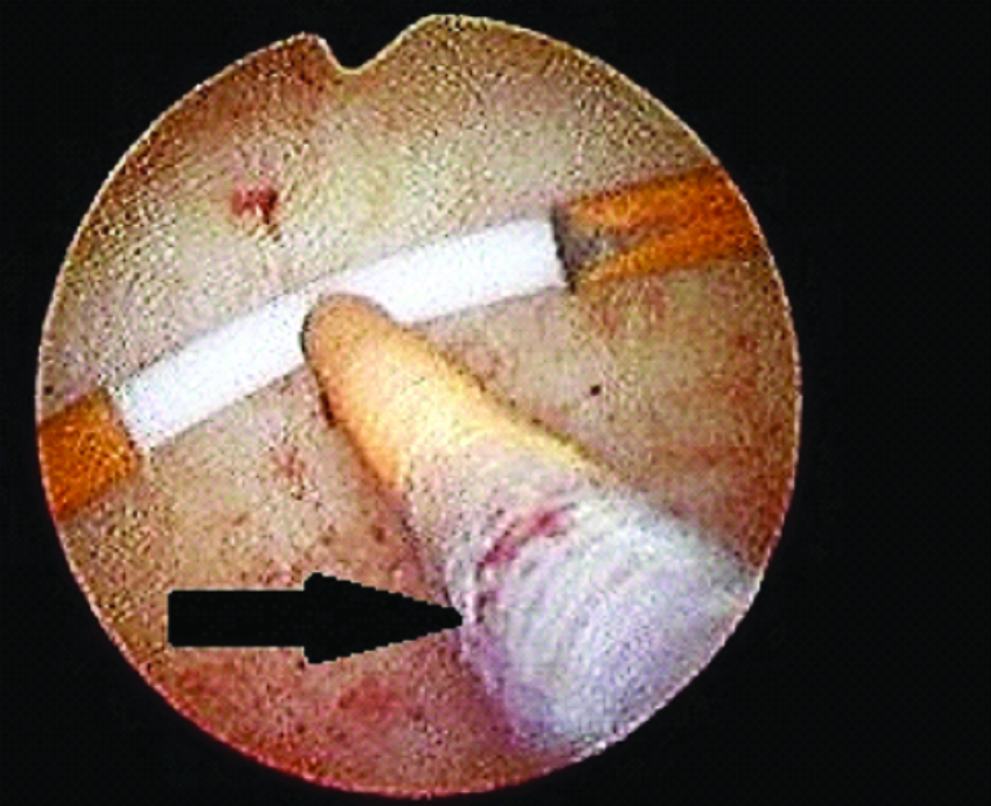
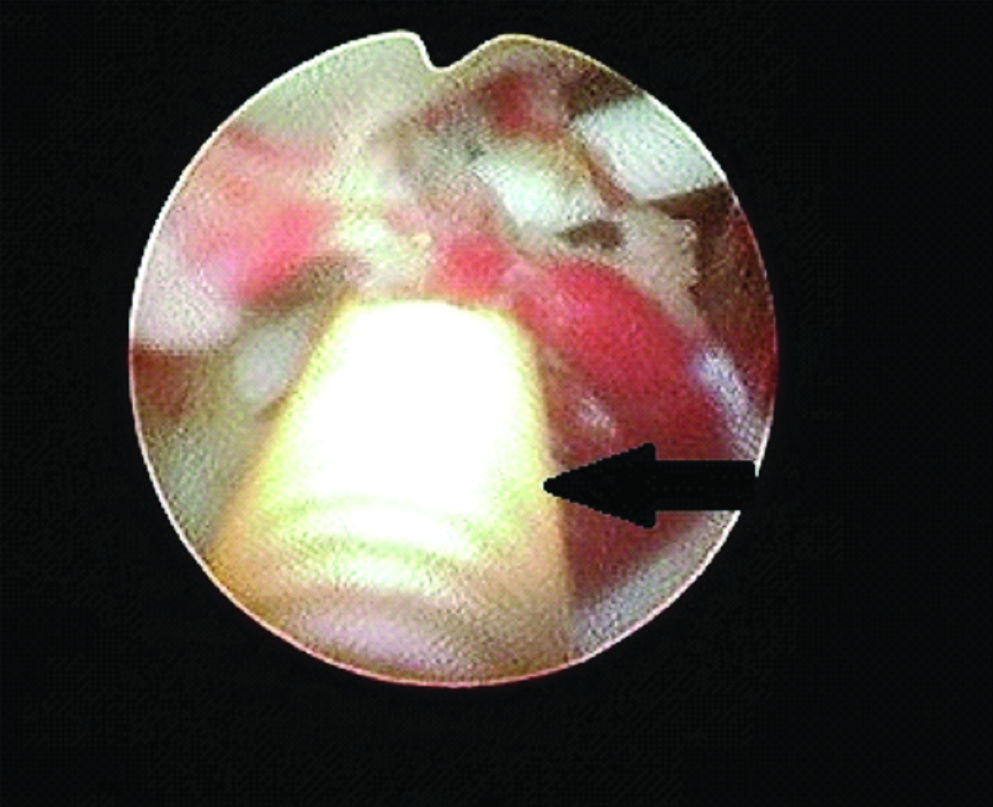
Total number of IUCD inserted during this period in our institute was 482. Surgical intervention was required in only 4.1% (20/482), out of which in 3.52% patients (17/482) IUCD was lying within the uterus (free/embedded in uterine wall) [Table/Fig-3,4] and in 0.6% patients (3/482) IUCD was lying in the peritoneal cavity after complete uterine perforation requiring laparoscopy [Table/Fig-5].
Hysteroscopic image of IUCD lying free in the uterine cavity at the fundus.
IUCD lying embedded in the lateral wall of the uterus (Hysteroscopic image).
Distribution of patients according to the surgical method for removal.
| Surgical procedure | No. of patients (N=20) | Percentage (%) |
|---|
| Malpositioned IUCD (Intra-uterine) | 17 | 85 |
| Removed under anaesthesia using long artery forceps | 4 | 23.53 |
| Hysteroscopic removal | 13 | 76.47 |
| Misplaced IUCD (Extra-uterine) | 3 | 15 |
| Laparoscopic removal | 3 | 100 |
| Laparotomy | 0 | 0 |
Majority of patients, 65% (13/20) were presented with missing thread as the most common complaint in the OPD. Other clinical features were pain abdomen and irregular vaginal bleeding [Table/Fig-6].
Distribution of patients according to the clinical complaints.
| Clinical features | No. of patients (n=20) | Percentage (%) |
|---|
| Missing thread | 13 | 65 |
| Pain abdomen | 2 | 10 |
| Irregular vaginal bleeding | 5 | 25 |
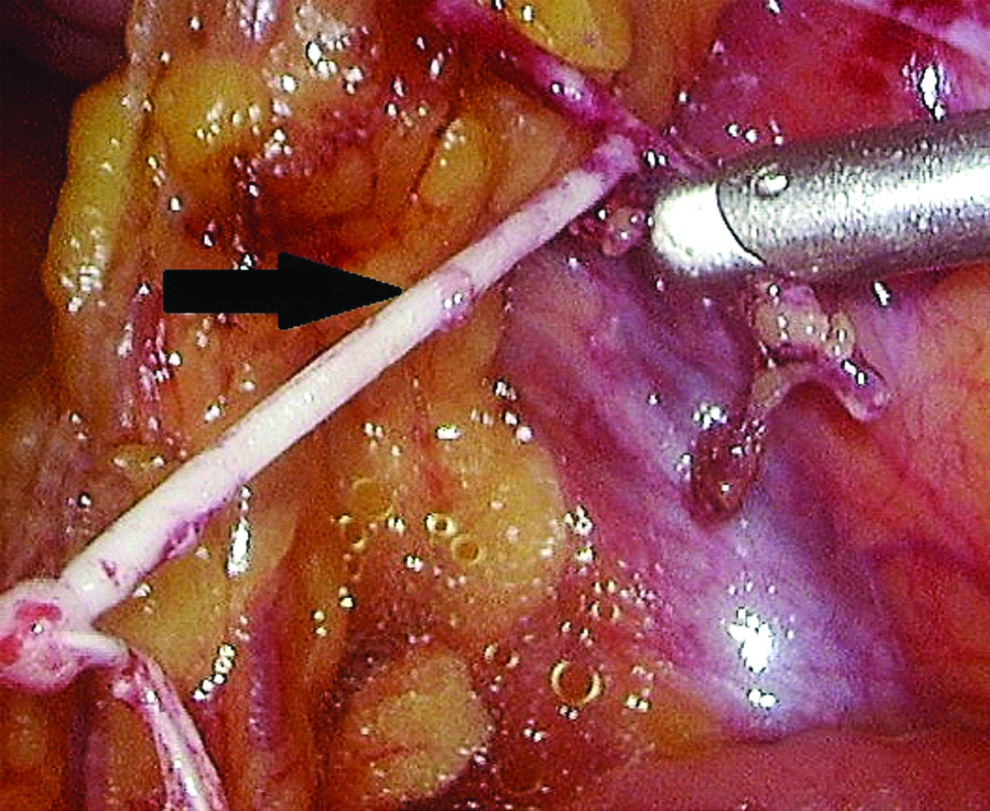
In 85% (17/20) of patients, IUCD were lying in the uterine cavity and in 15% (3/20), in the peritoneal cavity [Table/Fig-7,8]. A 64.70% (11/17) IUCD were lying free and 35.29% (6/17) were lying embedded in the uterine cavity. [Table/Fig-9]. All misplaced/transmigrated IUCD’s were removed by operative laparoscopy (100%) and none required laparotomy [Table/Fig-10].
Laparoscopic image of IUCD embedded within omentum.
Distribution of patients according to the location of IUCD.
| Location of IUCD | No. of patients n=20 (%) |
|---|
| Extra-uterine (Misplaced IUCD) | 3 (15%) |
| Omental adhesions | 2 (10%) |
| POD (buried under adhesions) | 1 (5%) |
| Intra-uterine (Malpositioned) | 17 (85%) |
| Fundus | 8 (47.05%) |
| Mid-cavity | 4 (23.52%) |
| Cervical canal | 5 (29.41%) |
Distribution of patients with malpositioned IUCD (Intra-uterine) according to the position on hysteroscopy/USG.
| Location | No. of patients (n=17) | Percentage (%) |
|---|
| Lying free in the uterine cavity | 11 | 64.70 |
| Straight | 8 | 72.72 |
| Oblique | 2 | 18.18 |
| Inverted | 1 | 9.09 |
| Lying embedded in the uterine cavity | 6 | 35.29 |
| Anterior wall | 2 | 33.33 |
| Fundus | 1 | 16.66 |
| Lateral wall | 2 | 33.33 |
| Previous Lower segment caesarean section scar site | 1 | 16.66 |
Details of patients with misplaced/Transmigrated IUCD.
| Patients | Type of IUCD | Time of insertion | Symptoms | Location of IUCD | Operative time | Complications/Duration of stay |
|---|
| First patient | CuT 380A | Interval | Missing thread | Omental adhesions | 30 min | Nil/48 hrs |
| Second patient | CuT 380A | Postpartum | Pain abdomen | POD (buried under adhesion) | 20 min | Nil/36 hrs |
| Third patient | CuT 380A | Interval | Pain abdomen | Omental adhesions | 40 min | Nil/48 hrs |
Discussion
Although a very small number of dislocated IUCD patients presented with acute symptoms requiring urgent surgery, mostly patients had no symptoms, and therefore had planned surgery. Despite of this, the current guidelines recommends that all dislocated IUCD’s should be removed surgically [18]. In the present study, the incidence of dislocated IUCD’s requiring operative interventions was 4.1% and the results are similar to the retrospective study conducted by Marchi NM et al., over 19 years duration, that showed incidence of 4.96% [19]. Sharma R and Suneja A, conducted a similar retrospective study in 2018 over five years duration in a tertiary care centre and showed incidence of 1.9% which is much lower than the current study [20]. This shows that the incidence of these complications is very rare and this should not be the reason to defer IUCD insertion. Proper counseling regarding benefits and complications is necessary before IUCD insertion. In this study, IUCD was intra-uterine (malpositioned) in location in 85% (17/20) patients. According to Gupta M and Jain G, Sun X et al., Marchi NM et al., Barsaul M et al., and Lawal SO et al., 90.6%, 70.40%, 98%, 79.93% and 63.48% patients respectively, had an IUCD inside the uterine cavity [1,7,19,21,22].
In this study, 65% (13/20) patients required hysteroscopic guided removal, in 20% (4/20) IUCD it was removed using long artery forceps under anaesthesia, 15% had laparoscopic removal and none required laparotomy. Similarly, Gupta M and Jain G, showed hysteroscopic guided removal in 68.75% patients (22/32), long artery forceps guided removal in 21.8% (7/32), laparoscopic removal in 6.25% (2/32) patients and laparotomy was done in 3.12% (1/32) patients [1]. Trivedi SS et al., conducted a study over 38 patients with missing thread and showed that in 92.1% (35/38) patients hysteroscopic guided removal was done and in only one patient (2.8%) laparotomy was done [23]. Sun X et al., has done a retrospective observational study over a period of eight years and included 98 patients [7], showed that among transmigrated IUCD, 75.9% had laparoscopy, 17.2% laparoscopy with hysteroscopy, 3.4% laparotomy and in 3.4% cystoscopy for the retrieval of IUCD and hysteroscopy was done for all who had an IUCD within the uterine cavity.
Frances R et al., done a systematic review (1997-2010) and identified 129 cases of transmigrated IUCD (within peritoneal cavity) in 30 studies, showing that 72.09% patients had laparoscopic removal and 27.9% had laparotomy for IUCD retrieval [18]. In 27 patients laparoscopies were converted to laparotomy due to the complexity of the procedure. In the present study, 15% (3/20) patients had complete uterine perforation and resultant transmigrated IUCD. Gupta M and Jain G, Varun N et al., Sun X et al., Marchi NM et al., and Elahi N and Koukab H, reported 9.37%, 5.56%, 29.95%, 0.6%, and 28.57% respectively of cases of IUCD migration to the peritoneal cavity [1,5,7,19,24]. This showed that there is a large variation in the incidence of transmigrated/misplaced IUCD.
Symptomatology of dislocated IUCD varies and it includes unwanted pregnancy [25], missing thread, pain lower abdomen, irregular vaginal bleeding and symptoms specific to organ perforated in case of transmigrated IUCD like chronic pelvic pain, lower urinary tract symptoms [26], peritonitis and fistula. In the current study missing thread was the most common complaint (65%). Results were similar to a study conducted by Mosley FR et al., where almost half of patients (48.1%) had missing thread as the most common complaint followed by (28.7%) presented with unwanted pregnancy, (17.8%) with pain, (4.7%) with irregular vaginal bleeding, and (0.8%) presented with chronic pelvic inflammatory disease [18]. Sun X et al., showed that (42.85%) patients were asymptomatic and most common clinical complaint was lower abdominal pain (25.51%). Missing thread was the presenting complaint in only (8.16%) patients which is much lower than the current study [7].
Ultrasonography and plain X-ray abdomen/pelvis are the main modalities for the diagnosis of dislocated IUCD. Ultrasonography is the initial investigation and plain X-ray abdomen/pelvis is indicated only if IUCD is not localised on USG or in case of non-availability of ultrasonography [3]. Abdominal Computed Tomography scan/Magnetic Resonance imaging may be required very rarely in cases of transmigrated/misplaced IUCD [14]. Accurate localisation of IUCD is essential before planning a surgical procedure as it affects the type of surgical procedure, success of procedure, complications encountered, need of additional intraoperative procedures like proctoscopy/cystoscopy, ensuring necessary equipments and specialist required and consent required preoperatively. WHO has recommended the removal of misplaced IUCD, irrespective of place and position, as early as possible, even in asymptomatic patients [27,28]. This is to prevent the future fibrosis and adhesion formation and in few cases may result in transmigration/penetration into adjacent pelvic/abdominal organs including the urinary bladder, small bowel, sigmoid colon and appendix. Minimally invasive surgeries are the diagnostic and therapeutic choice for the dislocated IUCD’s now-a-days. They impart high success rate in the retrieval of dislocated IUCD’s [9]. A literature review of surgical methods for the removal of IUCD showed that 93% cases were done laparoscopically but cases of organ perforations had laparotomies in 57.1% of cases [29].
Limitation
The main limitation in our study was the smaller number of patients. The data is from the single institute and results would be better if it’s a multi-centric study.
Conclusion
Most common presenting complaint of misplaced/malpositioned IUCD is missing thread followed by pain lower abdomen. Dislocated IUCD requiring operative interventions is very rare and this should not be the reason to defer IUCD insertion or use. Minimally invasive surgery is the treatment of choice. Awareness of people about this safe, effective, long-acting and reversible method of contraception is required in developing countries like India. Every effort should be made to lower down its complications and failure rates, so that more people can be counseled about this method. Proper counseling and follow-up needs to be ensured.