Primary Bone Lymphoma of Humerus Culminated to Shoulder Disarticulation- Astray of Diagnosis
Pankaj Kumar Mishra1, Sujeet Mishra2, Deepak Singh Maravi3, Sanjiv Gaur4, Ashish Gohiya5
1 Assistant Professor, Department of Orthopaedics, Gandhi Medical College, Bhopal, Madhya Pradesh, India.
2 Student, Department of Orthopaedics, Gandhi Medical College, Bhopal, Madhya Pradesh, India.
3 Professor, Department of Orthopaedics, Gandhi Medical College, Bhopal, Madhya Pradesh, India.
4 Professor and Head, Department of Orthopaedics, Gandhi Medical College, Bhopal, Madhya Pradesh, India.
5 Professor, Department of Orthopaedics, Gandhi Medical College, Bhopal, Madhya Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sujeet Mishra, Deparment of Orthopaedics, GMC and Hamidia Hospital, Bhopal-462011, Madhya Pradesh, India.
E-mail: drpankajv@yahoo.com
In the horizon of knowledge, there is dearth of documentation depicting the incidence of Primary Bone Lymphoma (PBL) being delayed/misdiagnosed as chronic osteomyelitis, which entails that this case report is of more magnitude. It is a case report of young female, having complaints of pain and swelling in left arm initially which was misdiagnosed as chronic osteomyelitis. Later on, she was diagnosed as PBL. Here, we want to discuss the clinical presentation of PBL, and to make aware from such grave pathology and to consider it in the differential diagnosis of chronic osteomyelitis.
B-cell, Osteomyelitis, Small lymphocytic lymphomas
Case Report
A 25-year-old female presented to our orthopaedic department with pain (three months) and swelling since two months of left arm with inability to use her left upper extremity. Pain was continuous, non-radiating and dull aching in nature. Diffuse swelling appeared over distal part of arm since two months back. On inspection it was pear shaped (approx- 20 cm in circumference and 15 cm in length), skin was shiny and stretched and there was venous engorgement. On palpation, local temperature was normal, with firm to hard consistency, with moderate tenderness and thickening of humerus bone. There was no history of previous trauma, weight loss, fever and night cries. General physical examination was unremarkable and routine haemogram was within normal range.
After history and clinical examination, we suspected for chronic osteomyelitis of left arm. The X-ray (AP and lateral view) of the left arm with elbow prescribed. X-ray revealed the diaphyseal pathological fracture of humerus with periosteal reaction, moth-eaten type lytic lesion and sequestrum [Table/Fig-1]. The clinico-radiological differential diagnosis of chronic osteomyelitis, tubercular osteomyelitis, osteosarcoma and multiple myeloma were installed. Haematological examinations were normal. Incisional biopsy was done and it revealed the features suggestive of chronic inflammation and granuloma. Ultimately, the final diagnosis of tuberculous osteomyelitis of humerus was thought. Arm was supported in U-cast and anti-tubercular treatment started and patient kept for observation and regular follow-up.
Antero-posterior and lateral view radiographs of left arm swelling revealing the moth eaten type lytic lesion (curved arrow), periosteal reaction (head of arrow), sequestrum (straight arrow) with pathological fracture.

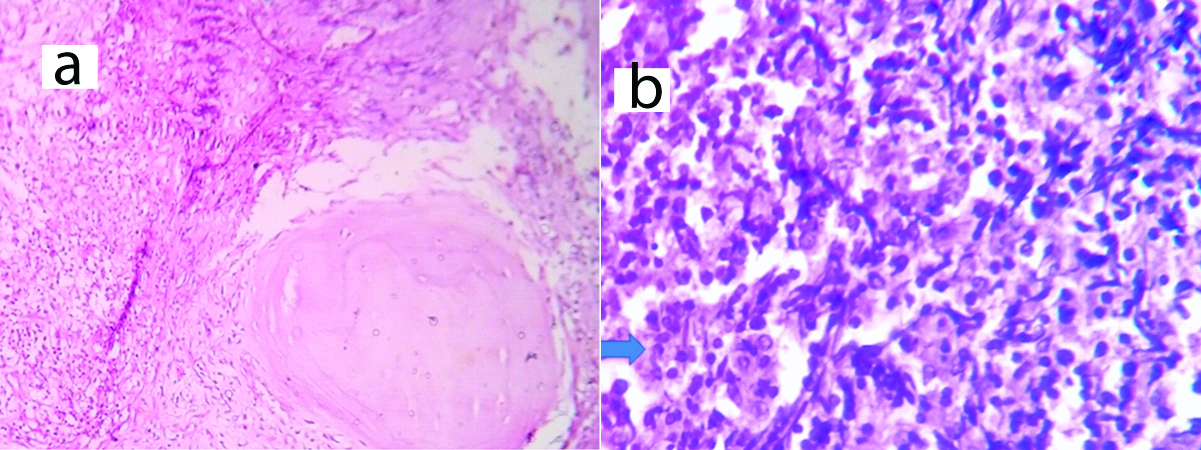
Patients did not turn at called follow-up, and around three months later she entered to OPD with gross swelling of arm, gross abnormal movement, and shiny skin with engorged veins [Table/Fig-2]. Again X–ray was done and now it showed the grossly destructed humerus with soft tissue haziness and lysis of bone with wide zone of transition suggestive of obvious malignant lesion [Table/Fig-3]. The MRI described the osteolytic lesion replaced by soft tissue with infiltrated neurovascular bundle and included the differential diagnosis of Ewing sarcoma and chondrosarcoma [Table/Fig-4]. Now it’s appeared that the previous diagnosis of chronic osteomyelitis was not accurate. The grave nature of pathology explained to the patient and second biopsy was planned. Since the whole of the humerus was involved and it was non-salvageable limb due to neurovascular infiltration so the shoulder disarticulation was planned [Table/Fig-5]. Furthermore, the histopathology revealed the neoplastic infiltrate composed of monomorphous population of small sized lymphocytes with round regular nuclei, increased numbers of mitotic figures, occasional nucleoli; clumped chromatin and absence of bizarre cell were suggestive of Small Lymphocytic Lymphoma [Table/Fig-6]. While the first biopsy slide was also matched with the second biopsy slide, but there were no any anaplastic cells in previous slide. Shoulder disarticulation done with the informed consent. After wound healing, patient underwent the local radiotherapy of 50Gy in 25 fractions. After 2 years of follow-up, she is doing well without any local and systemic recurrence.
Anterior and posterior view of arm showing the gross swelling and engorged veins.

Antero-posterior and lateral radiograph showing gross destruction of almost full length of humerus with wide zone of transition (bracket) and soft tissue haziness (arrow).

Axial T2 weighted (a) and coronal T2 weighted (b) MRI images of left arm depicting the large neoplastic bony mass, replacing the lower two third of humerus with infiltration of neurovascular bundle (arrow).
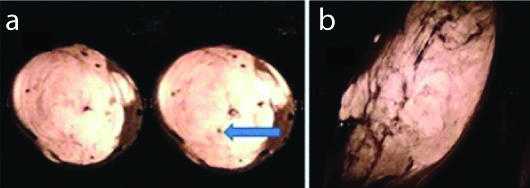
Disarticulated left upper extremity from the shoulder joint.

Haematoxylin and eosin stain: (a) 10X showing (bracket) extensive lymphoid infiltration; and (b) 40X depicting (arrow) pleomorphic (small sized) lymphocytes, regular nuclei, clumped chromatin and occasional nucleoli.
Discussion
Primary Bone Lymphoma (PBL) is an unusual tumour and has referential of origin from lymphoid and myelopoetic tissues [1]. Parker F et al., categorised the PBL as a separate clinical pathology [2]. Incidence of PBL is about 3% of all form of primary malignant bone tumours. PBL is an extra-nodal form of lymphoma and comprises 1% of all lymphoma [3]. It is considerably unintelligible to distinguish the primary from secondary bone lymphoma. Coley suggested the criteria to diagnose the PBL as lymphoma presenting at skeletal site with no evidence of disease at extra-skeletal site for at least six months after the diagnosis [4,5].
There are literatures who report that symptomatology of osteomyelitis masquerades the bone malignancy [6]. So there are fair chances of delayed or misdiagnosis, which will definitely and adversely affect the treatment outcome [7]. In this article, we want to emphasise that if there is unannounced, and staggered natural course of chronic osteomyelitis which must be conceded for rechecking of diagnosis by biopsy and immunohistochemistry.
PBL has been reported in every age group (first decade to 8th decade) but the peak of the prevalence is in 6th to 7th decade with slight male preponderance. Most of literature have found (metaphysis or diaphysis of long bone) the femur (29%) followed by pelvis (19%) as the most common site of predilection [8,9]. Accordance to the Revised European-American Lymphoma (REAL) classification, the most common PBL is diffuse large B-cell lymphoma type (92%), but the other types like small lymphocytic lymphoma, Burkitt’s type, anaplastic large cell lymphoma and Hodgkin’s lymphoma are also mentioned [10]. Though the incidence of PBL is more in late decades and male sex, but in our case it was a female with quite early age. The PBL is also very less common in humerus, as it occurred in our case.
Small lymphocytic lymphoma (chronic lymphocytic leukaemia) is a sub-type of non-Hodgkin B-cell lymphoma, and has an indolent course. In this literature, we are discussing the rarity of the SLL arising from bone. Even after diligent search, there are very few sporadic cases of small lymphocytic lymphoma/chronic lymphocytic leukaemia (originating from bone) are reported in literature.
Vincelli ID et al., reported the chronic lymphocytic leukaemia arising from foot, which got treated by radiotherapy [11]. Tuscano C et al., reported, another case of chronic lymphocytic leukaemia originated from distal tibia [12]. So here we are presenting this case as a rarity to the horizon of knowledge.
Pain in the extremity is the most common presenting symptom of PBL and the radiological findings are nonspecific hence the feature can be identified as inflammation, osteomyelitis, neuropathy, etc. so the PBL contests for broad differential diagnosis. Diagnosis of PBL is affirmed by biopsy. FNAC usually clinches the diagnosis but sometimes the necrosis, crush artifacts and fibrosis are responsible for inadequate sampling and diagnostic error [13]. The definitive diagnosis is established by immunohistochemistry study which shows the antibodies to CD20, CD3 and CD45. Combined modality of chemotherapy and radiotherapy has been advocated by various studies with overall response rate of 94% and better 5-year survival rate [14,15].
It is obvious that the delay in diagnosis will have the impact on prognosis. Our case also succumbed to delayed/misdiagnosis due to erratic findings, i.e., histology suggestive of chronic infection, clinico-radiological scenario of infection. Blum YC et al., reported the case series of lymphoma dissimulating the chronic inflammation [16]. Our case is another one case of PBL, pretends to chronic osteomyelitis.
Crush artifacts and fibrosis probably could have given the misdiagnosis in first biopsy sampling. Usual presentation of PBL is also responsible for its misdiagnosis. While the PBL is conceded as treatable disease, but in our case the astray of diagnosis resulted to such a point that we procured the unusual treatment. Thus in such case report, we want to say that, in case of chronic osteomyelitis like scenario, which is recalcitrant to treatment, the elaborate diagnostic work-up is needed and PBL should be included in the differential diagnostic armamentarium [17].
Conclusion
Chronic osteomyelitis and PBL share the close presenting features and poses the diagnostic challenge. We have to pay the high attention, if there is aberration from normal course of chronic osteomyelitis. Undue clinical presentation and progression of chronic osteomyelitis must be verified by biopsy and immunohistochemistry. The misdiagnosis or cursory attention may culminate to unconventional treatment as in our case.
[1]. Ostrowski ML, Unni KK, Banks PM, Shives TC, Evans RG, O’Connell MJ, Malignant lymphoma of boneCancer 1986 58:2646-55.10.1002/1097-0142(19861215)58:12<2646::AID-CNCR2820581217>3.0.CO;2-U [Google Scholar] [CrossRef]
[2]. Parker F, Jackson H, Primary reticulum cell sarcoma of boneSurg Gynecol Obstet 1939 68:45-53. [Google Scholar]
[3]. Singh T, Satheesh CT, Lakshmaiah KC, Suresh TM, Babu GK, Lokanatha D, Primary bone lymphoma: A report of two cases and review of the literatureJ Cancer Res Ther 2010 6:296-98.10.4103/0973-1482.7336621119256 [Google Scholar] [CrossRef] [PubMed]
[4]. Ramadan KM, Shenkier T, Sehn LH, Gascoyne RD, Connors JM, A clinicopathological retrospective study of 131 patients with primary bone lymphoma: A population-based study of successively treated cohorts from the British Columbia Cancer AgencyAnn Oncol 2007 18(1):129-35.10.1093/annonc/mdl32917018705 [Google Scholar] [CrossRef] [PubMed]
[5]. Pinheiro RF, Filho FDR, Lima GG, Ferreira FVA, Primary non-Hodgkin lymphoma of bone: An usual presentationJ Cancer Res Ther 2009 5:52-53.10.4103/0973-1482.4877219293492 [Google Scholar] [CrossRef] [PubMed]
[6]. Cabanela ME, Sim FH, Beabout JW, Dahlin DC, Osteomyelitis appearing as neoplasms. A diagnostic problemArch Surg 1974 109:68-72.10.1001/archsurg.1974.013600100500124599774 [Google Scholar] [CrossRef] [PubMed]
[7]. Karuppal R, Manjunath S, Raman RV, Sandhya S, Immunohistochemistry in primary B-cell lymphoma of tibia masquerading as chronic osteomyelitisIndian J Orthop 2017 51(4):477-80.10.4103/0019-5413.20995228790479 [Google Scholar] [CrossRef] [PubMed]
[8]. Lin F, Staerkel G, Fanning TV, Cytodiagnosis of primary lymphoma of bone on fine-needle aspiration cytology specimens: Review of 25 casesDiagn Cytopathol 2003 28:205-11.10.1002/dc.1026612672096 [Google Scholar] [CrossRef] [PubMed]
[9]. Nasiri MRG, Varshoee F, Mohtashami S, Raziee HR, Aledavood A, Ghafarzadeh K, Primary bone lymphoma: A clinicopathological retrospective study of 28 patients in a single institutionJ Res Med Sci 2011 16:814-20. [Google Scholar]
[10]. Harris NL, Jaffe ES, Stein H, Banks PM, Chan JK, Cleary ML, A revised European-American classification of lymphoid neoplasms: A proposal from the International Lymphoma Study GroupBlood 1994 84:1361-92. [Google Scholar]
[11]. Vincelli ID, Cufari P, Al Sayyad S, Tuscano C, Porta N, Di Cristofano C, A patient with chronic lymphocytic leukaemia and bone localization: A case reportBlood 2015 126:5301 [Google Scholar]
[12]. Tuscano C, Vincelli ID, Arico’ D, Marchione AM, Versace P, Stelitano C, A rare case of appendicular skeleton localization in a patient with chronic lymphocytic leukaemia successfully treated with salvage radiation therapyAdv Radiat Oncol 2017 3(2):121-24.10.1016/j.adro.2017.01.00729904735 [Google Scholar] [CrossRef] [PubMed]
[13]. Maruyama D, Watanabe T, Beppu Y, Kobayashi Y, Sung-Won K, Tanimoto K, Primary bone lymphoma: A new and detailed characterization of 28 patients in a single-institution studyJpn J Clin Oncol 2007 37:216-23.10.1093/jjco/hym00717472971 [Google Scholar] [CrossRef] [PubMed]
[14]. Qureshi A, Ali A, Riaz N, Pervez S, Primary non-hodgkin’s lymphoma of bone: Experience of a decadeIndian J Pathol Microbiol 2010 53(2):267-70.10.4103/0377-4929.6434020551530 [Google Scholar] [CrossRef] [PubMed]
[15]. Leonard R, Prosnitz NG, Non–hodgkin’s lymphoma. In: Halperin EC, Perez CA, Brady LW, editorsPrinciple and Practice of Radiation Oncology 2008 PhiladelphiaLippincott Williams and Wilkins:1739-61. [Google Scholar]
[16]. Blum YC, Esterhai JL, Esmail AN, Lackman RD, Donthineni-Rao R, Lymphoma masquerading as infectionClin Orthop Relat Res 2005 432:267-71.10.1097/01.blo.0000150104.82757.4a15738831 [Google Scholar] [CrossRef] [PubMed]
[17]. Mika J, Schleicher I, Gerlach U, Adler CP, Uhl M, Knoeller SM, Primary bone lymphomas thought to be osteomyelitis urgently demand a rapid diagnosis in bone pathologyAnticancer Res 2012 32:4905-12. [Google Scholar]