Pemphigus Vulgaris: Case Report and Review of Literature
Preeti Ahankare1, Divyesh Wankhedkar2, Sangeeta Patankar3, Gokul Sridharan4
1 Postgraduate, Department of Oral Pathology and Microbiology, YMT Dental College and Hospital, Navi Mumbai, Maharashtra, India.
2 Lecturer, Department of Oral Pathology and Microbiology, YMT Dental College and Hospital, Navi Mumbai, Maharashtra, India.
3 Professor and Head, Department of Oral Pathology and Microbiology, YMT Dental College and Hospital, Navi Mumbai, Maharashtra, India.
4 Associate Professor, Department of Oral Pathology and Microbiology, YMT Dental College and Hospital, Navi Mumbai, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Gokul Sridharan, Institutional Area, Sector 4, Kharghar, Navi Mumbai, Maharashtra, India.
E-mail: drgokuls@gmail.com
Autoimmune mucocutaneous disorders of oral cavity constitute an important group of lesions that pose diagnostic, therapeutic and prognostic difficulties to the dental clinician. Pemphigus vulgaris is an autoimmune blistering condition that usually affects the oral mucosa and is characterised by autoantibodies directed against the desmoglein component of the keratinocytes. It manifests clinically as vesicles, bullae or desquamative gingivitis and histopathologically shows the presence of acantholysis. Immunofluorescent demonstration of IgG antibodies against desmoglein usually confirms the diagnosis. The resemblance in clinical appearance to other oral diseases mandates the inclusion of pemphigus vulgaris in the differential diagnosis of oral vesiculo-bullous lesions. Adequate knowledge of diagnostic and therapeutic modalities helps the clinician in appropriate management. This paper presents a case report of pemphigus vulgaris affecting both oral cavity and skin along with a brief review of literature.
Autoimmune disorders, Oral mucosa, Pemphigus vulgaris
Case Report
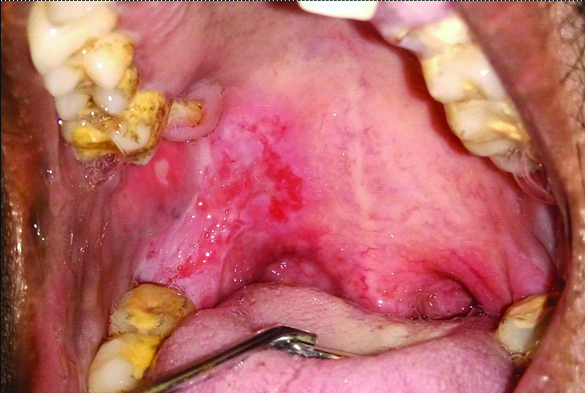
A 44-year-old male patient reported to the Department of Oral Pathology and Microbiology with a chief complaint of pain and burning sensation associated with ulcers in the upper right back region of mouth for the past 25-30 days. The patient was apparently alright prior to the occurrence of ulcerative lesions of the oral cavity. A history of weight loss and fever for 15 days along with itching and skin lesions on the back, chest and lower limbs was elicited. The overall general condition of the patient was fair and there was no history of fever, malaise and any other systemic problems. There was no history of allergy to drugs, chemicals and food substances. The oral hygiene was poor and the patient had habit of chewing tobacco but no associated lesions and drinking alcohol 3-4 times per day since 20 years. Intraoral examination revealed diffuse erythematous lesions with ulceration on the hard palate extending from maxillary tuberosity to the retromolar area and soft palate of the right side [Table/Fig-1]. Along with the oral lesions, the patient had difficulty in swallowing. On general examination, raw eroded and crusted areas with a central erythematous zone were present on the chest and the back region [Table/Fig-2]. Considering the oral and dermal manifestations, the condition was provisionally diagnosed as pemphigus.
Oral manifestation of the lesion at initial presentation.
Dermal manifestations of the lesion at initial presentation.

Considering the clinical presentation, the differential diagnosis that can be considered are erythema multiforme, lichen planus, lupus erythematosus, pemphigoid, recurrent aphthous stomatitis, acute herpetic gingivostomatitis and epidermolysis bullosa. Erythema multiforme is characterised by target-shaped skin lesions, oral erosions, involvement of lips in the form of erosions and crusts occurring in response to an allergic reaction to viral particles or drugs. The lack of a known history of allergy and absence of target lesions helped in ruling out this lesion. Lichen planus is an immune mediated disorder chiefly seen as interconnecting white striae affecting the oral mucosa and skin. Variant of lichen planus namely bullous and erosive lichen planus may occur in the oral cavity and is considered as an important differential diagnosis in the present case. While lichen planus is generally bilaterally symmetrical, it may not be always applicable to the bullous and erosive form. Additionally, the absence of Wickham’s striae and negative Nikolsky’s sign may help in excluding this lesion. However absolute exclusion of lichen planus needs histopathological confirmation. Pemphigoid is an autoimmune disorder characterised by autoantibodies against the hemidesmosomal components of basement membrane. Clinically, this condition is seen in older age group, shows the presence of intact vesicles for longer duration and usually heals with scarring. Acute herpetic gingivostomatitis is a viral infection caused by herpes simplex virus infection and clinically presents with prodromal symptoms followed by the onset of small yellowish vesicles that rapidly rupture, giving rise to ulcers with an erythematous halo. The lesion usually runs a short course of 7 to 10 days and eventually heals without scarring. The absence of prodromal symptoms, presence of skin lesions and the long duration of the lesions were helpful in its exclusion. Recurrent aphthous stomatitis are generally induced by certain underlying trigger factors, appear as ulcers in oral mucosa with yellowish base, surrounded by an erythematous halo and regular margins and are self-limiting with absence of skin lesions.
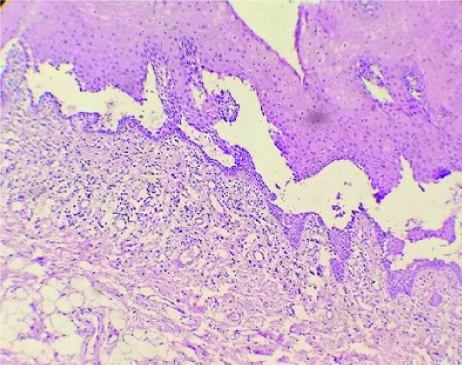
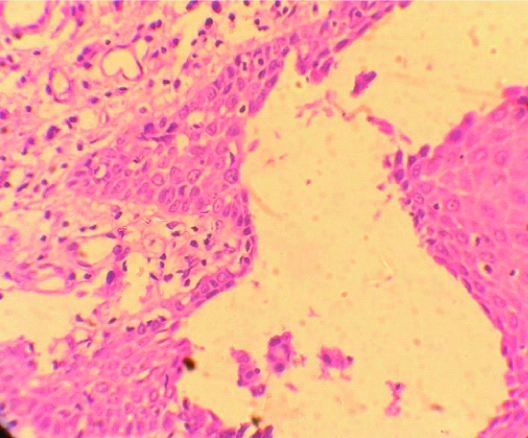
Microscopic examination of the oral lesion in the present case showed a non-keratinised stratified squamous epithelium with intra-epithelial split and high power magnification which confirmed the presence of acantholytic cells in the split region [Table/Fig-3,4]. The underlying connective tissue showed non-specific infiltration of chronic inflammatory cells. The patient was then referred to dermatologist for evaluation of the skin lesions. Histopathological and direct immunofluorescence of the skin lesions confirmed the diagnosis as pemphigus vulgaris. The patient was started with oral prednisolone, calcium, Vitamin D, Azathioprine and a liquid diet treatment. A two week follow-up from beginning of the treatment showed completed resolution of oral lesions [Table/Fig-5]. The skin lesions, however, did not completely subside indicating the severity of the condition leading to poor patient compliance. The patient did not continue the treatment and later was lost to follow-up.
Photomicrograph (10x) showing non-keratinized stratified squamous epithelium with intra-epithelial split.
Photomicrograph (40X) showing intra-epithelial split with acantholytic cells.
Clinical image of the oral cavity two weeks post therapy.

In the present case, the oral findings were unusual in that they manifested as ulcerated and erythematous areas rather than the typical vesicles which are the hallmark of pemphigus vulgaris. While pemphigus vulgaris is generally reported in females, the present case reported an occurrence in an otherwise healthy male.
Discussion
Pemphigus is a life-threatening mucocutaneous disorder affecting the skin and mucous membrane which is clinically presented by vesicle formation and histologically by intra-epithelial cleft and acantholysis [1,2]. Pemphigus vulgaris is a common autoimmune blistering disease always affecting the oral mucosa and it can be the initial site of presentation before involving the skin or other mucous membranes [3]. The oral manifestations of pemphigus vulgaris typically run a chronic course causing blisters, erosions and ulcers of the oral mucosa [1]. The dermal manifestation is not a common occurrence and many times the oral lesions are the primary clinical presentation of pemphigus vulgaris [4]. The worldwide prevalence of pemphigus vulgaris is about 0.1 to 0.5% per million population per year [5]. The incidence of pemphigus, however, varies as per the geographic area and ethnic population. Literature data suggest that the incidence of pemphigus vulgaris ranges from 0.76 to 16 per million population per year in Europe [6]. In India, the prevalence of pemphigus vulgaris is lesser than the rest of the world and is in the range of 0.09% to 1.8% [7]. Pemphigus vulgaris has a prolonged clinical course with significant morbidity and mortality [8]. If pemphigus is left untreated, for two years the mortality is 50% and at the end of 5 years, it is nearly 100%. The causes of mortality included extensive skin involvement, septicemia, bronchopneumonia, electrolyte imbalance and secondary systemic infections [1,7].
The oral manifestations of pemphigus vulgaris may either precede or occur in conjunction with cutaneous lesions. A definitive diagnosis is made based on the clinical features, histopathologic features and immunological tests so as to aid in appropriate and prompt therapeutic intervention. Several literature data have reported cases of pemphigus vulgaris with oral and cutaneous manifestations which are tabulated in [Table/Fig-6] [9-14].
Summary of cases of pemphigus vulgaris with oral and cutaneous manifestations reported in the literature.
| Author and Year | Age/Sex | Oral Manifestations | Cutaneous manifestation | Treatment | Prognosis |
|---|
| Rath SK et al., [9] | 36 year/Female | Oral and gingival ulcers since 3 months associated with burning sensation | Small eruptions on skin of face, back and extremities since 3 weeks | 0.1% Triamcinolone acetonide ointment for oral lesions and 0.05% Clobetasol with Soframycin twice daily for skin lesions along with 20 mg prednisolone orally | Lesions under control and regular follow-up |
| Temilola D et al., [10] | 54 year/Female | Painful oral ulcers preceded by vesicles involving the hard palate, soft palate, buccal mucosa and gingiva for 9 months | Ocular involvement after a few weeks following oral involvement. Later small erythematous lesions on extensor surfaces of both thighs | Systemic prednisolone 60 mg/day for 7 days and topical steroids for ocular involvement | Oral and ocular lesions healed after 7 days of treatment. Skin lesions developed later and the patient was referred to dermatologist |
| Ramineni HB et al., [11] | 24 year/Female | Multiple oral ulcers for one month not relieved on medication | Later, generalised fluid filled vesicles all over the body | Oral prednisolone 100 mg for one week, gradually tapered and symptomatic treatment | Patient was responding well to treatment |
| Vijay P et al., [12] | 40 year/Female | Ulcerative and eroded lesions on tongue and buccal mucosa present intermittently since one year | Concomitant presence of reddish brown eroded and ulcerated lesions on arms and trunk | Oral prednisolone 60 mg/day for 4 days with gradual tapering and topical application for oral lesions | Symptomatic relief at 15 days follow-up |
| Aggarwal A and Jain S, [13] | 53 year/Female | Linear erosions on buccal mucosa, labial mucosa and gingiva since 3 days | Widespread ulcerative lesions on anterior neck below chin region since 2 weeks | 2 cycles of IV dexamethasone 100 mg for 3 days along with 500 mg of cyclophosphamide at interval of 4 weeks. A 30 mg/day prednisolone during the interval period | Complete remission of the lesion at the end of therapy |
| Vasudevan V et al., [14] | 49 year/Male | Multiple ulcers on right and left buccal mucosa and floor of the mouth | Multiple ulcers on scalp, back, trunk and extremities | Prednisolone 60 mg/day for a month with tapering of dose | One-month follow-up showed regression of lesions in oral cavity and several body sites |
The current treatment strategies for treatment of pemphigus vulgaris include topical and systemic corticosteroids in combination with immunosuppressants such as azathioprine or mycophenolate. Treatment can also be augmented with intravenous immunoglobulin or plasmapheresis, which aims to reduce circulating autoantibody levels. Treatment with the anti-CD20 antibody rituximab has been shown to be effective in inducing short-term disease remission [15]. Following remission of the lesions, it is necessary for a maintenance regimen to control the disease as well as reduce the side effects of the drugs. The duration of medical treatment varies depending on the extent of involvement by the lesion.
Conclusion
Pemphigus vulgaris is a common, yet life threatening autoimmune mucocutaneous disorder with increased tendency to affect the oral mucosa. The oral manifestations of pemphigus vulgaris are usually the initial and at times the sole manifestation encountered by the clinician. Timely diagnosis and prompt treatment are hence necessary for complete cure with reduced morbidity and mortality owing to the chronic and often fatal course of this condition.
[1]. Black M, Mignogna MD, Scully C, Pemphigus vulgarisOral Dis 2005 11:119-30.10.1111/j.1601-0825.2005.01139.x15888101 [Google Scholar] [CrossRef] [PubMed]
[2]. Nagaraju B, Ramu A, Vidhyadhara S, Gunasree H, Arun Kumar C, A case study on pemphigus vulgarisIndian Journal of Pharmacy Practice 2016 9(4):266-68.10.5530/ijopp.9.4.9 [Google Scholar] [CrossRef]
[3]. Robinson NA, Yeo JF, Lee YS, Aw DCW, Oral pemphigus vulgaris: A case report and literature updateAnn Acad Med Singapore 2004 33(Suppl):63S-68S. [Google Scholar]
[4]. Da silva K, Mandel L, Early manifestation of pemphigus vulgaris. A case reportN Y State Dent J 2007 73:42-44. [Google Scholar]
[5]. Karisetty B, Reddy KN, Lahkar M, Prevalence of Pemphigus vulgaris and Pemphigus Foliaceus in tertiary care hospital in India: an updateThe Pharma Innovation Journal 2013 2:68-72. [Google Scholar]
[6]. Huang YH, Kuo CF, Chen YH, Yang YW, Incidence, mortality, and causes of death of patients with pemphigus in Taiwan: a nationwide population-based studyJournal of Investigative Dermatology 2012 132:92-97.10.1038/jid.2011.24921850023 [Google Scholar] [CrossRef] [PubMed]
[7]. Kanwar AJ, De D, Pemphigus in IndiaIndian J DermatolVenereolLeprol 2011 77:439-49.10.4103/0378-6323.8239621727691 [Google Scholar] [CrossRef] [PubMed]
[8]. Alpsoy E, Akman-Karakas A, Uzun S, Geographic variations in epidemiology of two autoimmune bullous diseases: pemphigus and bullous pemphigoidArch Dermatol Res 2015 3017:291-98.10.1007/s00403-014-1531-125589418 [Google Scholar] [CrossRef] [PubMed]
[9]. Rath SK, Reenesh M, Gingival pemphigus vulgaris preceding cutaneous lesion: A rare case reportJournal of Indian Society of Periodontology 2012 16:588-91.10.4103/0972-124X.10692223493851 [Google Scholar] [CrossRef] [PubMed]
[10]. Temilola D, Holmes H, Mulder Van Staden S, Afrogheh A, Engelbrecht J, Oral pemphigus vulgaris with skin and ocular involvementSADJ 2018 73:83-85. [Google Scholar]
[11]. Ramineni HB, Yerraguntla M, Pulimila S, Kukkapalli NB, Suryadevara V, Pemhigus vulgaris: a rare case reportInt J Res Med Sc 2015 3:1543-44.10.18203/2320-6012.ijrms20150186 [Google Scholar] [CrossRef]
[12]. Vijay P, Pardhe N, Singhal I, Oral mucosal pemphigus with cutaneous involvement: Rare case reportInternational Journal of Current Research 2016 8:43666-67. [Google Scholar]
[13]. Aggarwal A, Jain S, Self-limiting cutaneous pemphigus preceding the oral lesions- A case reportActa Scientific Dental Sciences 2019 3:59-63. [Google Scholar]
[14]. Vasudevan V, Bharathan VV, Radhika , Pemphigus vulgarisJournal of Indian Academy of Oral Medicine and Radiology 2008 20:121-23.10.4103/0972-1363.52781 [Google Scholar] [CrossRef]
[15]. Ellebrecht CT, Payne AS, Setting the target for pemphigus vulgaris therapyJCI Insight 2017 2(5):e9202110.1172/jci.insight.92021 [Google Scholar] [CrossRef]