Acute coronary syndrome and coronary artery disease combined account for 70 lacs deaths every year. Acute coronary syndrome is among the leading cause of mortality in Asia-Pacific region and it accounts for half of the total global burden. Among these patients the cardiovascular outcomes vary with age, gender, ethnicity, educational status [1]. Identification of acute myocardial infarction patients at risk of developing major adverse cardiovascular events at admission to hospital is necessary to reduce damage to cardiac myocytes and left ventricular dysfunction. Previous studies have reported use of echocardiographic measurements like the left atrial volume, ejection fraction in predicting adverse cardiac events during hospital admission in patients diagnosed to have ST-elevation acute myocardial infarction [2].
A restrictive filling of left ventricle is an important predictor of both morbidity and mortality in acute myocardial infarction patients. The left atrium during diastolic phase is exposed to left ventricular filling pressures through the mitral orifice opening. The factors which determine filling pressure during diastole also influence the left atrial size [3]. Hence, to know the LAVI as predictor of major in-hospital adverse cardiac events like heart failure, pulmonary oedema and cardiogenic shock, this study was taken.
Materials and Methods
This was a prospective observational study which was done on the patients who were admitted with ‘acute coronary syndrome’ in Shri BM Patil Medical College, Vijayapur, Karnataka, India, between November 2015 to August 2017. Institutional ethical committee approval was taken, (Ref.No/58/2015 dated 20-11-2015). The sample was determined by the prevalence rate of acute coronary syndrome, 1-10%, at 95% confidence level and at 5% margin of error, the sample size was 69-70 [4].
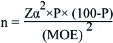
Zα=Z value at α level=95%
P=Prevalence rate=5%
MOE=Margin error=5%
Patients with significant valvular lesions like mitral stenosis or mitral regurgitation, congenital heart disease like atrial septal defects, ventricular septal defects, bundle branch block, poor acoustic window and age less than 18 years were excluded from study.
Clinical history and examination, electrocardiogram at admission, blood investigations like cardiac enzymes-Troponin T, Creatine Phosphokinase (CPK-MB), complete blood count, blood glucose, renal function test, serum electrolytes, chest x-ray to look for pulmonary oedema and cardiomegaly were recoreded.
Transthoracic 2D Echocardiography and Doppler study was done in patients with acute coronary syndrome within the first 24 hours and repeated if necessary. The echo machine used in this study was SIEMEN’S transthoracic two dimensional echo machine G450 with 3.5 MHz transducer. Left atrial volume was measured from standard apical 4 chamber view at the end of the systole using biplane method of discs. The border of left atrium includes the walls of the left atrium excluding left atrial appendages and pulmonary vein. LAVI has been calculated by dividing left atrial volume and body surface area using Mostellar formula [5].

BSA=Body surface area
W=Weight in kg
H=Height in cm
Patients with LAVI >32 mL/m2 were grouped into group A and patients with LAVI <32 mL/m2 were grouped into group B.
The major adverse cardiovascular events were decided by Killip’s classification in the following way:
Killip class I includes individuals with no clinical signs of heart failure.
Killip class II includes individuals with rales or crackles in the lungs, an S3, and elevated jugular venous pressure.
Killip class III describes individuals with frank acute pulmonary oedema.
Killip class IV describes individuals in cardiogenic shock or hypotension (measured as systolic blood pressure lower than 90 mmHg), and evidence of peripheral vasoconstriction (oliguria, cyanosis or sweating) [6].
Statistical Analysis
All characteristics were summarised descriptively. For continuous variables, the summary statistics of mean, Standard Deviation (SD) were used. For categorical data, the number and percentage were used in the data summaries. Chi-square (χ2)/Freeman-Halton Fisher-exact test were employed to determine the significance of differences between groups for categorical data. If the p-value was <0.05, then the results were considered to be statistically significant otherwise it was considered as not statistically significant. Data were analysed using SPSS software v.23.0.
Results
Total of 88 patients were admitted with acute coronary syndrome in Shri BM Patil Medical College, Vijayapur, between November 2015 to August 2017 were included in the study. Total of 84 patients were included in the present study that fulfilled the inclusion criteria and four patients were excluded of which one patient had left bundle branch block, one patient had severe aortic regurgitation with left bundle branch block, two patients had severe mitral regurgitation. Demographic data in group A and B are demonstrated in [Table/Fig-1].
| Variables | Group A | Group B | p-value |
|---|
| Age (years) | 68.1±9.8 | 53.2±11.6 | 0.028 |
| Sex (male/female) | 16/10 | 35/23 | 0.014* |
| Pulse rate (beats per minute) | 94±24.1 | 86±22.5 | 0.243 |
| Systolic blood pressure (mm of hg) | 126.2±26 | 136.1±24.6 | 0.561 |
| Diastolic blood pressure (mm of hg) | 81.7±16.9 | 84.2±16.1 | 0.687 |
| Hemoglobin (gm%) | 12.6±2.1 | 13±2.3 | 0.021* |
| Total leucocyte count (cells/cumm) | 12407.6±5624 | 13124±5737.1 | 0.191 |
| Random blood sugar (mg/dL) | 184.3±96.2 | 176±99.6 | 0.305 |
| Blood urea (mg/dL) | 28.7±13.9 | 27.6±14.1 | 0.216 |
| Serum creatinine (mg/dL) | 1.0±0.8 | 0.9±0.7 | 0.044* |
| Serum sodium (mmoL/L) | 137.6±3.6 | 140±4.0 | 0.967 |
| Serum potassium (mmoL/L) | 4.3±0.9 | 4.2±0.5 | 0.584 |
| Creatine kinase MB (IU/mL) | 79.1±68.5 | 78±66.7 | 0.164 |
| Left ventricular ejection fraction (%) | 37.9±5.1 | 46.7±5.95 | 0.001* |
| Body surface area (m2) | 1.2±0.3 | 1.22±0.2 | 0.028 |
| Left atrial volume (mL) | 44.6±9.6 | 24.1±10.1 | <0.001 |
| Left atrial volume index (mL/m2) | 43.2±11.2 | 22.9±10.9 | <0.001 |
Out of 84 patients with acute coronary syndrome, 51 patients (60.7%) were male and 33 patients (39.3%) were female. Out of 26 patients in group A, 16 patients (61.5%) were male and 10 patients (38.5%) were female and out of 58 patients in group B, 35 patients (60.3%) were male and 23 patients (39.6%) were female as depicted in [Table/Fig-2]. In this study, mean age was 68.1±9.8 years and 53.2±11.6 years in group A and group B respectively.
Age and sex distribution.
| Age (Yrs) | Male | Female | p-value |
|---|
| N | % | N | % |
|---|
| 19-29 | 0 | 0 | 0 | 0 | 0.026* |
| 30-39 | 1 | 2.0 | 1 | 3.0 |
| 40-49 | 10 | 19.6 | 0 | 0.0 |
| 50-59 | 16 | 31.4 | 5 | 15.2 |
| 60-69 | 16 | 31.4 | 19 | 57.6 |
| 70-79 | 4 | 7.8 | 4 | 12.1 |
| ≥80 | 4 | 7.8 | 4 | 12.1 |
| Total | 51 | 100.0 | 33 | 100.0 |
In group A, out of 26 patients common risk factors was age >50 years in 25 patients (96%) and in group B, out of 58 patients common risk factors were age >50 years in 47 patients as demonstrated in [Table/Fig-3].
Distribution of risk factors.
| Risk factors | LAVI <32 mL/m2 | LAVI ≥32 mL/m2 | Total | p-value |
|---|
| N | % | N | % | N |
|---|
| Non Modifiable | Age >50 yrs | 47 | 81 | 25 | 96.1 | 72 | 0.014* |
| Sex | Male | 35 | 68.6 | 16 | 31.4 | 51 | 0.918 |
| Female | 23 | 69.7 | 10 | 30.3 | 33 |
| Family history | 1 | 100 | 0 | 0 | 1 | <0.001* |
| Modifiable | Smoking | 13 | 65.0 | 7 | 35.0 | 20 | 0.044* |
| Alcohol | 9 | 90.0 | 1 | 10.0 | 10 | 0.025* |
| Tobacco chewing | 15 | 78.9 | 4 | 21.1 | 19 | 0.028* |
| Diabetes mellitus | 13 | 59.1 | 9 | 40.9 | 22 | 0.058 |
| Hypertension | 14 | 63.6 | 8 | 36.4 | 22 | 0.043* |
| Obesity | 4 | 36.3 | 7 | 63.6 | 11 | 0.211 |
Echocardiography done in 26 patients in group A, demonstrated anterior wall hypokinesia in nine patients (35%) and out of 58 patients in group B, anterior wall hypokinesia in 19 patients (32%). In group A, left ventricular ejection fraction was 37.9±5.1% and in group B, left ventricular ejection was 46.7±5.95% with p-value of <0.001 as demonstrated in [Table/Fig-4]. Mean left atrial volume in group A was 43.2±11.2 mL/m2 and in group B was 22.8±10.9 mL/m2 [Table/Fig-1]. Out of 26 patients in group A, LAVI in male patients was 40.4 mL/m2 and in female patients were 42.7 mL/m2. In group B, LAVI in male patients was 25.1 mL/m2 and in female patients it was 22.6 mL/m2.
Distribution of echocardiographic variables.
| Echocardiographic Variables | LAVI <32 mL/m2 | LAVI ≥32 mL/m2 | N | p-value |
|---|
| N | % | N | % |
|---|
| Regional wall motion abnormality | Anterior wall | 19 | 67.9% | 9 | 32.1 | 28 | 0.051 |
| Anterolateral | 5 | 71.4 | 2 | 28.6 | 7 |
| Anteroseptal | 8 | 66.6 | 4 | 33.3 | 12 |
| Inferior | 11 | 61.1 | 7 | 38.9 | 18 |
| Inferolateral | 10 | 76.9 | 3 | 23.1 | 13 |
| Lateral | 1 | 100 | 0 | 0 | 1 |
| Global | 1 | 50 | 1 | 50 | 2 |
| Normal | 3 | 100 | 0 | 0 | 3 |
| Diastolic dysfunction | Grade 0 | 44 | 84.6 | 8 | 15.4 | 52 | <0.001* |
| Grade 1 | 12 | 52.17 | 11 | 47.8 | 23 |
| Grade 2 | 2 | 25 | 6 | 75 | 8 |
| Grade 3 | 0 | 0 | 1 | 100 | 1 |
| Mean | Standard Deviation | Mean | Standard Deviation | | |
| Ejection fraction | | 46.7 | 5.95 | 37.9 | 5.1 | | <0.001* |
During hospital stay, 84 patients having acute coronary syndrome were observed for development of major adverse cardiovascular events like pulmonary oedema, cardiogenic shock, heart failure and death. In group A, most common major adverse cardiac event was cardiogenic shock in nine patients (34.6%) compared to four patients (6.8%) in group B with p-value<0.001, followed by pulmonary oedema in nine patients (34.6%) of group A compared to three patients (5.17%) in group B with p-value<0.001. In this study, major adverse cardiac events like pulmonary oedema (34.6% vs 5.2%), cardiogenic shock (34.6% vs 6.8%), heart failure (11.5% vs 3.4%) and death (19.2% vs 1.7%) were found to be higher in group A patients compared to group B patients with p-value<0.001, which is statistically very significant as shown in [Table/Fig-5].
Distribution of Major Adverse Cardiac Events (MACE).
| MACE | LAVI <32 mL/m2 | LAVI ≥32 mL/m2 | Total | p-value |
|---|
| N | % | N | % | N |
|---|
| Heart failure | 2 | 40.0 | 3 | 60.0 | 5 | 0.001* |
| Pulmonary oedema | 3 | 25.0 | 9 | 75.0 | 12 | <0.001* |
| Cardiogenic shock | 4 | 30.8 | 9 | 69.2 | 13 | <0.001* |
| Death | 1 | 16.7 | 5 | 83.3 | 6 | <0.001* |
| Others |
| 1st degree heart block | 1 | 100.0 | 0 | 0.0 | 1 | 0.075 |
| Bradycardia | 1 | 100.0 | 0 | 0.0 | 1 |
| Complete heart block | 1 | 100.0 | 0 | 0.0 | 1 |
| Monomorphic ventricular tachycardia | 0 | 0.0 | 1 | 100.0 | 1 |
| Ventricular premature complex | 1 | 100.0 | 0 | 0.0 | 1 |
| Polymorphic ventricular tachycardia | 2 | 100.0 | 0 | 0.0 | 2 |
*Significant at 5% level of significance (p<0.05)
Discussion
In group A patients (LAVI >32 mL/m2), average age was 68.1±9.8 years and in group B patients (LAVI <32 mL/m2), average age was 53.2±11.6 years. Older age group seems to be associated with increased LAVI (>32 mL/m2), due to physiological changes of aging like increased blood pressure, left atrial stiffness, progressive diastolic dysfunction with loss of early relaxation [7]. These findings were different from study done in 171 patients with acute coronary syndrome, where mean age in patients with LAVI <32 mL/m2 was 63±13 years and that off in patients with LAVI >32 mL/m2 was 70±13 years [8].
In this study male sex appears to be a risk factor for overall occurrence of acute coronary syndrome and sex does not vary between group A and group B. In a study done in total 395 acute coronary syndrome patients, patients with LAVI >32 mL/m2 female patients were 19 (31.7%) and in patients with LAVI <32 mL/m2, female patients were 65 (20%). In their study there were significantly more female patients in LAVI >32 mL/m2 group compared to LAVI <32 mL/m2 group [3].
Older age, diabetes mellitus and hypertension are associated with increased left atrial volume (>32 mL/m2), than other risk factors and they are prone for major adverse cardiac events. These findings were similar to study done in 171 patients with acute coronary syndrome [8]. The increased LAVI in diabetes mellitus and hypertension can be due to underlying diastolic dysfunction leading to increased left ventricular end diastolic pressure and raised LAV in those patients [9].
On electrocardiogram there was no significant difference in ST segment changes among both the groups Though electrocardiogram showed ST elevation in leads indicating particular area of infarction, findings in 2D echocardiography were contrasting in few patients. In a study done in 50 acute myocardial infarction patients, anteroseptal wall ST segment elevation was observed in 22% of patients, anterolateral wall in 26% of patients and inferior wall in 48% of patients which is different from this study [10].
On 2D-Echocardiography, there was no significant difference between wall motion abnormalities in patients of the two groups. This is because of severe systolic dysfunction after acute myocardial infarction which further leads to increase in left ventricular pressure and volume overload leading to back pressure and then to left atrial remodeling and further increase in LAV. In a study done in 395 patients with acute myocardial infarction and found the mean ejection fraction in patients with LAVI <32 mL/m2 to be 45.3% and in patients with LAVI >32 mL/m2 to be 41.9% where the difference between two groups was less significant than this study [3]. In another study done in 314 patients having acute myocardial infarction, patients in LAVI >32 mL/m2 group had ejection fraction of 44% and in patients with LAVI <32 mL/m2 ejection fraction was 50% and there was significantly lower ejection fraction of left ventricle in LAVI >32 mL/m2 group compared to LAVI <32 mL/m2 group [11].
In patients without primary left atrial pathology, left atrial enlargement occurs because of pressure overload due to diastolic dysfunction leading to increased left ventricular end diastolic pressure and exposure of left atrium to such high pressure and volume overload states [12]. Left atrial volume varies with body size. So, it is a better calculated by dividing it by body surface area. In this study, group A 39.9% patients had LAVI >32 mL/m2 and group B 60.1% had with LAVI <32 mL/m2. These findings were similar to a study done, where they also found LAVI >32 mL/m2 in 39% of total study population with acute myocardial infarction [11]. In another study done in 395 patients with acute coronary syndrome, LAVI >32 mL/m2 was identified in 63 patients (19%) which is lower than this study [3]. Another study done in 171 patients with acute coronary syndrome, LAVI >32 mL/m2 was identified in 78 patients (45%) which was higher than this study [8]. These contrasting results in different studies are probably because of differences in risk factors, previous cardiac insults, geographical locations. In this study, group A with increased LAVI is associated with old age, male sex, diabetes mellitus, hypertension, severe left ventricular dysfunction indicated reduced left ventricular ejection fraction in the patients.
The two main forms of acute cardiac failure are acute pulmonary oedema and cardiogenic shock. Both entities are major adverse cardiac events, with high mortality requiring diagnosis and management. Acute pulmonary oedema is due to the leakage of fluid through the alveolar capillary membrane due to an acute cardiac episode. Cardiogenic shock is characterised by hypotension with systolic blood pressure <90 mmHg or decreased mean arterial pressure >30 mmHg, absent or decreased diuresis (<0.5 mL/kg/h). The most common cause is left ventricular failure due to acute myocardial infarction [13].
Common major adverse cardiac events were cardiogenic shock in 34.6% of which early initiation of treatment prevented mortality. Patients having LAVI >32 mL/m2 had worse prognosis in terms of major adverse cardiac events like heart failure, pulmonary oedema, cardiogenic shock and death. So, in general, patients having LAVI <32 mL/m2 has good outcome. Early initiation of treatment prevented mortality in patients with LAVI >32 mL/m2 and helped in early recovery. These complications associated are predicted by increased LAVI which indicate severe systolic and diastolic dysfunction in the patients leading increased end diastolic pressure of left ventricle and major adverse cardiac events like pulmonary oedema, heart failure, cardiogenic shock and death. So, patients with raised LAVI should observe closely for development of major adverse cardiac events. In another study done in 395 patients with acute myocardial infarction concluded that increased LAVI predicts the mortality [3]. Observations in this study were similar to a study done, in which they found that in 78 patients with LAVI >32 mL/m2, the number of patients with major adverse cardiovascular events like pulmonary oedema, heart failure, shock, reinfarction and death were significantly higher compared to number of patients with LAVI <32 mL/m2 and recommended routine echocardiographic measurement of LAV to predict prognosis in patients with acute coronary syndrome [8]. The left atrial volume predicts survival after acute myocardial infarction and LAVI >32 mL/m2 was an important independent predictor of mortality due to any cause and proved in a previous study [11]. In a similar study done in 61 patients with acute ST elevation myocardial infarction, they found LAVI >32 mL/m2 predicted 100% chance of developing heart failure [14]. In this study, acute coronary syndrome patients in group A (LAVI >32 mL/m2) were found to have more major adverse cardiac events. Hence, LAVI should be measured in all patients with acute coronary syndrome so that early treatment can be initiated and major adverse cardiac events be prevented.
Limitation
This study has some limitations. The patients were selected at a single center. Left atrial size could have been measured with newer techniques, such as real-time 3D echocardiography, but 2D echocardiography was used due to limited experience. In addition, it is worth noting that the number of variables assessed as compared with the sample size might have reduced the power to identify other factors.
Conclusion
Routine measurement of left atrial volume and calculation of LAVI in patients with acute coronary syndrome is necessary to prevent major adverse cardiovascular events like heart failure, pulmonary oedema, cardiogenic shock and death.
*Significant at 5% level of significance (p<0.05)