A Curious Case of Pneumomediastinum caused after Diesel Aspiration
Jyoti Bajpai1, Amritesh Mishra2, Surya Kant3, Darshan Kumar Bajaj4
1 Senior Resident, Department of Respiratory Medicine, King George’s Medical University, Lucknow, Uttar Pradesh, India.
2 Junior Resident, Department of Respiratory Medicine, King George’s Medical University, Lucknow, Uttar Pradesh, India.
3 Professor and Head, Department of Respiratory Medicine, King George’s Medical University, Lucknow, Uttar Pradesh, India.
4 Assistant Professor, Department of Respiratory Medicine, King George’s Medical University, Lucknow, Uttar Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Jyoti Bajpai, B Block, 703, Halwasiya Lorepur, New Hyderabad, Lucknow-226007, Uttar Pradesh, India.
E-mail: jyotibajpai33@gmail.com
Subcutaneous emphysema and Pneumomediastinum can occur as an uncommon complication of inhalation of irritant. It is a rare complication of hydrocarbon ingestion. There are many causative factors like oesophageal, chest trauma and iatrogenic in nature. Other causes include assisted ventilation and medical or dental procedures as well as several diseases. It can also spontaneously occur due to coughing, vomiting, and forceful straining, such as in childbirth or strenuous exercise. However, subcutaneous emphysema and pneumo mediastinum as a consequence of ingestion of hydrocarbons use is very rare with only a few reported cases. Here, we report an uncommon scenario after accidental diesel ingestion masquadering as subcutaneous emphysema.
Pneumonitis, Pneumothorax, Subcutaneous emphysema
Case Report
A 36-year-old adult male, non-smoker, non-diabetic and non-hypertensive farmer presented to the OPD with chief complaint of breathlessness, for the past ten days. The patient gave a history of cough without expectoration and fever two months back for which he was put on standard Antitubercular Therapy (ATT) by a local physician. He did not respond to therapy and discontinued ATT.
On examination, he was conscious and well oriented. His pulse rate was 120 beats per minute with a blood pressure of 90/60 mm Hg. He had a respiratory rate of 26 breaths per minute with oxygen saturation of 84% on room air and he was afebrile. There was decreased air entry on the left side with bilateral crepitation. The rest of his physical examination was unremarkable.
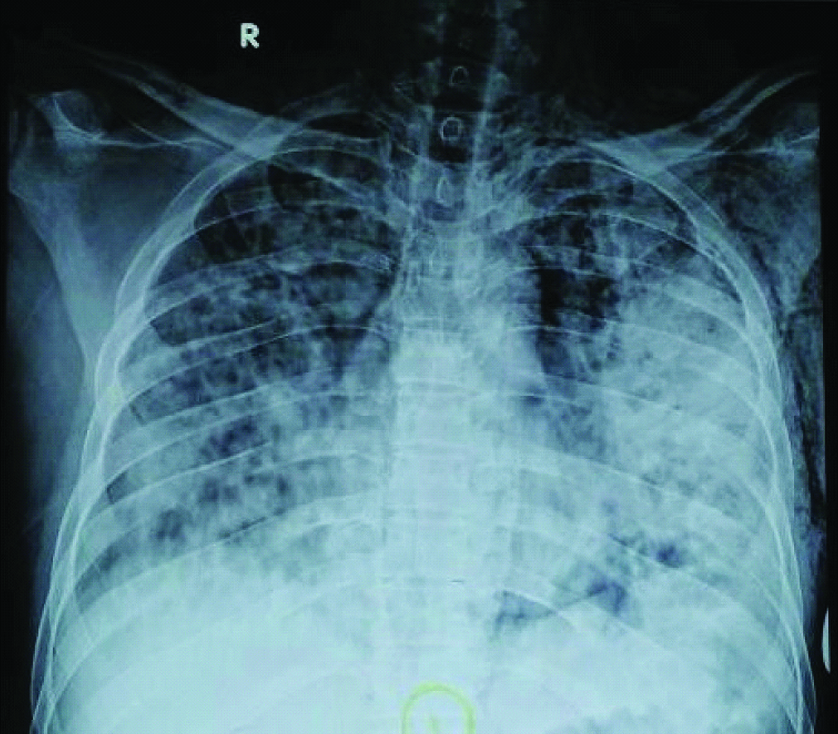
Routine blood investigations were within normal limits, Mantoux showed no induration; he was unable to expectorate sputum and chest X-ray AP view showed bilateral consolidation with subcutaneous emphysema [Table/Fig-1].
Chest X-ray AP view showing bilateral consolidation with subcutaneous emphysema.
With neither the history nor investigations suggesting a diagnosis of TB or bacterial pneumonia, patient’s history was reviewed. He gave a history of accidental diesel aspiration at his farm two months back during transfer from a container to the generator. He had developed mild left sided chest pain which was relieved on taking analgesics. One week later, he developed dry cough and low grade fever for which he was started on ATT.
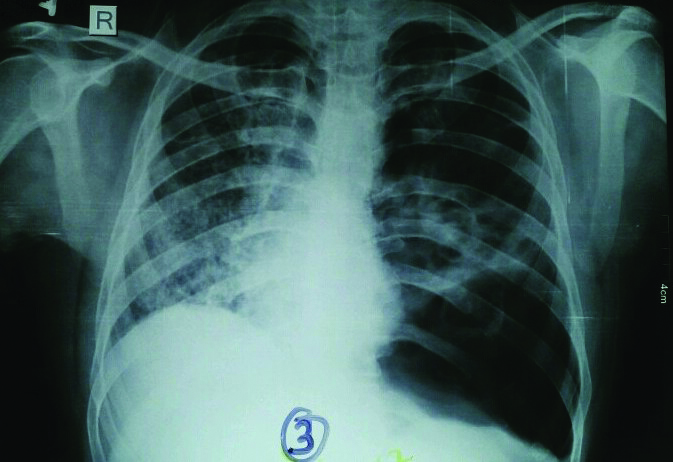
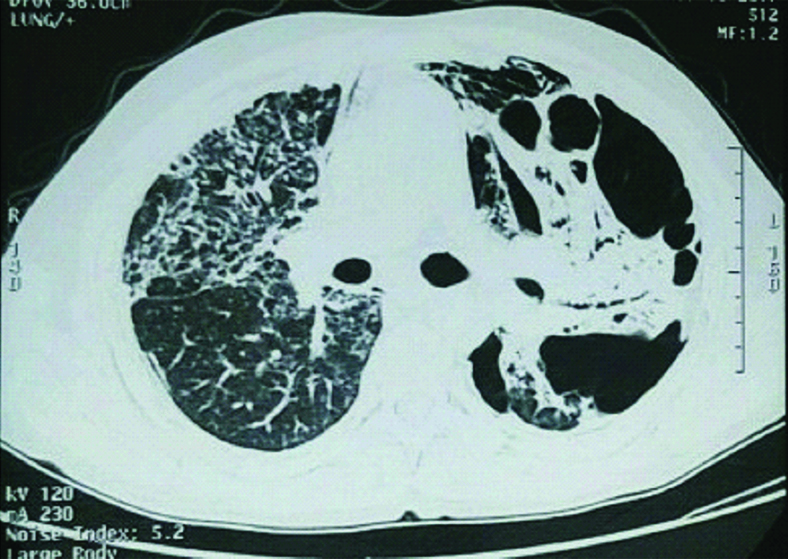
At our centre, the patient was put on intravenous antibiotics, analgesics and anti-tussives and high flow oxygen. ATT was stopped as there was no evidence of Tuberculosis (TB). Repeat chest radiograph-PA view was done after 10 days which revealed a cavitary lesion in left middle zone with areas of hyperlucency [Table/Fig-2]. CECT thorax was done which showed left sided consolidation with various shaped cavities and areas of emphysematous changes [Table/Fig-3].
Chest X-ray AP view showing left side pneumothorax with right side consolidation.
CECT thorax lung window showing left side cavitatory consolidation.
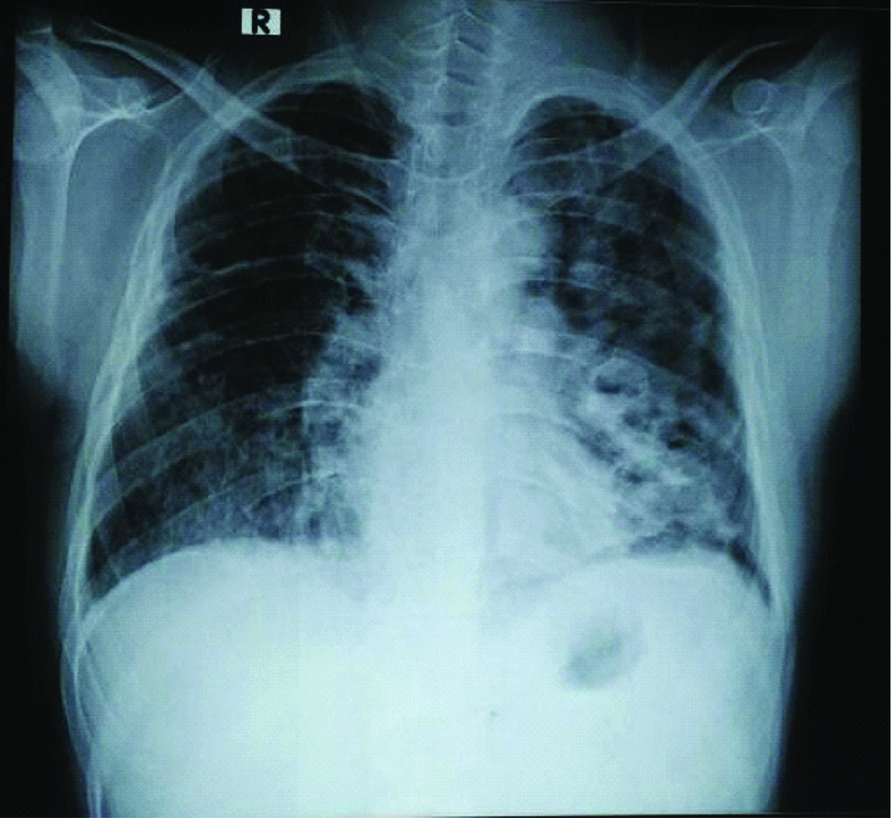
Patient was put on antibiotics and analgesics therapy and was discharged in stable condition and was asked to review after 15 days. The chest radiograph-PA view, after 15 days of discharge from hospital, showed clinical improvement. Patient is now stable and doing well [Table/Fig-4].
Chest X-ray AP view after therapy showing improvement.
Discussion
Aspiration is defined as entry of material such as stomach contents, pharyngeal secretions from the oropharynx or gastrointestinal tract into larynx and lower airway [1]. Aspiration syndromes include Mendelson’s syndrome, airway obstruction, lung abscess, lipoid pneumonia, chronic interstitial fibrosis, and Mycobacterium fortuitum pneumonia. Lipoid pneumonia is classified as exogenous, endogenous, and idiopathic. Exogenous lipoid pneumonia is a rare entity resulting from inhalation of fatty substances. Siphonaging of diesel/kerosene in rural areas in India is not a very uncommon practice. Diesel aspiration usually presents as chronic respiratory illness but may also present acutely. Pneumo-mediastinum is frequently associated with other forms of extra-alveolar air, including pulmonary interstitial emphysema, pneumo-pericardium, pneumothorax, subcutaneous emphysema, pneumo-retroperitoneum, and pneumo-peritoneum. The majority of patients with spontaneous pneumo-mediastinum have predisposing factors that cause increase in airway pressure, which leads to alveolar rupture. Toxin ingestion (Ecstacy) is a very rare cause of Pneumo-mediastinum leading to subcutaneous emphysema [2-4]. Spontaneous Pneumomediastinum develops after rupture of perivascular alveoli. Following the rupture of alveoli air enters in mediastinum via vascular sheath and subsequently deeper along facial planes into the neck [5]. Two common mechanism of perivascular rupture include sudden increase in the bronchovascular pressure gradient (invasive ventilation and valsalvamaneuver) and decrease in pulmonary interstitial pressure such as in asthma and bronchiolitis [6]. Aspiration of hydrocarbon can lead to a vast variety of respiratory symptoms ranging from simple cough to critical and life threatening condition such as pneumothorax. Hydrocarbon pneumonia also popularly called as fire eater pneumonia develops due to ingestion of volatile low viscous hydrocarbons [7]. Mineral oil pneumonia is inflammation of the lung due to the aspiration of mineral oil [8]. Most commonly found in certain occupation related persons such as drivers, automobile mechanics and farmers. Pulmonary oedema, atelectasis or consolidation is the most frequent presentations [9]. The spectrum of presentation with oil pneumonitis is varied and includes breathlessness, cough, chest pain and haemoptysis. The central nervous system, the gastrointestinal tract and the lungs are most commonly involved. Systemic complications of these substances include central nervous system and cardiovascular system but rarely fatal. The most serious and fatal complications mainly occur because of pulmonary toxicity, in the form of aspiration pneumonitis, lipoid pneumonia, lung abscess, pleural effusion and rarely, pneumothorax [10,11].
Pneumatocele formation is the well-known complication of hydrocarbon pneumonitis [12]. The radiological lesions are generally out of proportion to the clinical findings [13]. Radiographic findings include unilateral or bilateral lung consolidation, pneumatoceles, pleural effusion, atelectasis and spontaneous pneumothorax [14].
Generally they affect the basal regions because they are low viscous and elicit very little cough response in upper airway tract and thus settle in basal regions leading to basal crepitation and consolidation [15]. It is presumed that the most common site is right middle lobe because the patient had to bend in a characteristic way for shiphonaging the diesel which generally is aspirated in the right middle lobe [16]. The treatment is usually empirical, as there is insufficient data advocating the utility of corticosteroids and antibiotics [17].
In a country like ours where tuberculosis is widespread and endemic, more often patients presenting with cough, breathlessness and radiological opacities are initiated with ATT even without microbiological confirmation. Such practices though practically sound in remote areas, can lead unwanted ATT regimens and prescriptions. In such a scenario, eliciting past history of exposure turned to be prudent and ameliorated prolonged ATT with its attendant adverse effects.
Conclusion
The current case vignette highlights the unusual and delayed manifestations of accidental hydrocarbon ingestion leading to diagnostic challenges. The history of ingestion may be concealed and only an active history search could elicit it as in our case. The clinical presentation can be varied from a mere consolidation or a pleural effusion to life threatening situations like Pneumomediastinum and Pneumothorax.
[1]. Marik PE, Aspiration pneumonitis and pneumonia: a clinical reviewN Engl J Med 2001 344(9):665-71.10.1056/NEJM20010301344090811228282 [Google Scholar] [CrossRef] [PubMed]
[2]. Marasco SF, Lim HK, Ecstasy-associated pneumomediastinumAnnals of the Royal College of Surgeons of England 2007 89(4):389-93.10.1308/003588407X18337317535617 [Google Scholar] [CrossRef] [PubMed]
[3]. Rezvani K, Kurbaan AS, Brenton D, Ecstasy induced pneumomediastinumThorax 1996 51(9):960-61.10.1136/thx.51.9.9608984713 [Google Scholar] [CrossRef] [PubMed]
[4]. Gungadeen A, Moor J, Extensive subcutaneous emphysema and pneumomediastinum after ecstasy ingestionCase Rep Otolaryngol 2013 2013:79586710.1155/2013/79586724187639 [Google Scholar] [CrossRef] [PubMed]
[5]. Yi MS, Kim KI, Jeong YJ, Park HK, Lee MK, CT findings in hydrocarbon pneumonitis after diesel fuel siphonageAm J Roentgenol 2009 193(4):1118-21.10.2214/AJR.09.247119770336 [Google Scholar] [CrossRef] [PubMed]
[6]. Koç İ, Dökme A, Pneumonia due to diesel fuel aspiration: A case reportGaziantep Med J 2015 21(1):62-64.10.5455/GMJ-30-163889 [Google Scholar] [CrossRef]
[7]. Pham K, Sverchek J, McPheeters RA, Chemical Pneumonitis from Hydrocarbon AspirationWest J Emerg Med 2008 9(3):165 [Google Scholar]
[8]. Blanc PD, Acute pulmonary responses to toxic exposure. In: Murray JF, Nadel JA, et alTextbook of Respiratory Medicine 2010 5th edPhiladelphiaElsevier10.1016/B978-1-4160-4710-0.00068-7 [Google Scholar] [CrossRef]
[9]. Mallavarapu RK, Katner HP, Pneumatocele complicating acute hydrocarbon pneumonitisClin Toxicol (Phila) 2008 46(9):91110.1080/1556365080226650118792828 [Google Scholar] [CrossRef] [PubMed]
[10]. Khanna P, Devgan SC, Arora VK, Shah A, Hydrocarbon pneumonitis following diesel siphonageIndian J Chest Dis Allied Sci 2004 46:129-32. [Google Scholar]
[11]. Verma AK, Singh A, Kishore K, Kant S, A rare cause of pneumothorax: Diesel aspiration pneumonitisMuller J Med Sci Res 2018 9(1):30-33.10.4103/mjmsr.mjmsr_9_17 [Google Scholar] [CrossRef]
[12]. Fishman JA, Aspiration, empyema, lung abscess and anaerobic infection. In: Fishman AP, Elias JA, Fishman JA, Grippi MA, Senior RM, Pack AI, editorsFishman’s Pulmonary Diseases and Disorders 2008 4th edNew YorkMcGraw Hill:2150 [Google Scholar]
[13]. Hadda V, Khilnani GC, Bhalla AS, Mathur S, Lipoid pneumonia presenting as non resolving community acquired pneumonia: A case reportCases J 2009 2:933210.1186/1757-1626-2-933220062592 [Google Scholar] [CrossRef] [PubMed]
[14]. Marchiori E, Zanetti G, Mano CM, Irion KL, Daltro PA, Hochhegger B, Lipoid pneumonia in 53 patients after aspiration of mineral oil: Comparison of high-resolution computed tomography findings in adults and childrenJ Comput Assist Tomogr 2010 34(1):09-12.10.1097/RCT.0b013e3181a9ec9f20118714 [Google Scholar] [CrossRef] [PubMed]
[15]. Siddiqui EU, Razzak JA, Naz F, Khan SJE, Factors associated with hydrocarbon ingestion in childrenJ Pak Med Assoc 2008 58(11):608-12. [Google Scholar]
[16]. Baron SE, Haramati LB, Rivera VT, Radiological and clinical findings in acute and chronic exogenous lipid pneumoniaJ Thorac Imaging 2003 18(4):217-24.10.1097/00005382-200310000-0000214561906 [Google Scholar] [CrossRef] [PubMed]
[17]. Marchioni E, Zanetti G, Mano CM, Hochhegger B, Exogenous lipid pneumonia. Clinical and radiological manifestationsRespir Med 2011 105(5):659-66.10.1016/j.rmed.2010.12.00121185165 [Google Scholar] [CrossRef] [PubMed]