Cheyne Stokes Breathing in a Case of Tubercular Meningitis with Hydrocephalus
Parag Papalkar1, Sourya Acharya2, Samarth Shukla3
1 Resident, Department of Medicine, DMIMS/JNMC, Wardha, Maharashtra, India.
2 Professor, Department of Medicine, DMIMS/JNMC, Wardha, Maharashtra, India.
3 Professor, Department of Pathology, DMIMS/JNMC, Wardha, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sourya Acharya, Department of Medicine, J.N Medical College ABVR Hospital, DMIMS University Sawangi (Meghe), Wardha-442001, Maharashtra, India.
E-mail: souryaacharya74@gmail.com
Apnea, Chemoreceptors, Near apnea, Ventilation
Dear Editor,
Breathing patterns are usually regular and seldom attracts attention. However, certain forms of breathing may be seen in patients of severe heart failure, strokes, meningitis, encephalitis, brain tumours, head trauma, severe diabetes, or metabolic alkalosis in which there are recurrent apneas or near apneas. Cheyne J and Stokes W described a symmetrical and regularly recurring waxing and waning of breathing with apneas almost 200 years back [1,2]. In neurology, it is claimed that Cheyne stokes breathing can be an altered variation of Biot’s breathing occurring in meningitis [3]. In this article we discuss a similar finding seen in a case of tubercular meningitis.
A 22-year-old female presented to emergency with 2 weeks history of headache, fever, on and off vomiting. Headache was diffuse without any history of photophobia or phonophobia. Fever was of moderate grade, intermittent in nature. There was no history of seizures, diplopia or any focal neurological deficit. Patient went to a local village doctor for the same and was receiving some alternative medications. On the day of admission, patient had an episode of generalised tonic clonic seizures for which she was brought to this hospital.
On examination patient was in a post-ictal state. She was drowsy with Glasgow coma scale of 5/14 and her pupils were semi-dilated sluggishly reacting to light. Her breathing was laboured. Central nervous system examination revealed hyperreflexia in all four limbs with bilateral extensor plantar responses. In view of laboured breathing, patient was intubated and put on mechanical ventilator. She was started with empirical antibiotics and anti-epileptics.
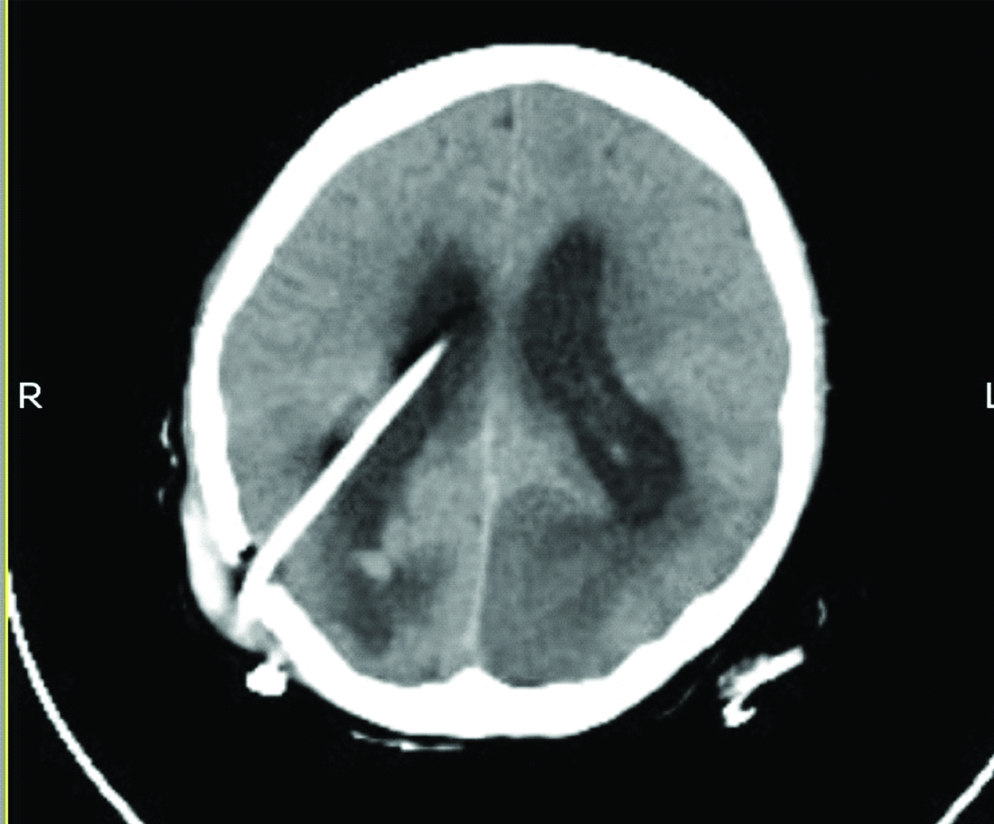
Computed Tomography (CT) of brain revealed a provisional diagnosis of hydrocephalus [Table/Fig-1]. Lumbar puncture was done and Cerebrospinal Fluid (CSF) revealed total leucocyte count of 2500/mm3 with 88% lymphocytes, sugar-30 mg/dL and protein-200 mg/dL, CSF Adenosine deaminase-45 U/L (cut-off >30 U/L) suggestive of Tubercular meningitis.
CT image depicting evidence of dilated bilateral lateral ventricle, third ventricle, fourth ventricle and cisterna magna suggestive of communicating hydrocephalus.

Patient was started on anti-tubercular treatment in the form of Tab.isoniazid-300 mg od, Tab. rifampin-450 mg od, Tab. pyrazinamide-750 mg bid, Tab. Ethambutol 800 mg od and empirical antibiotics in the form of third generation cephalosporins were continued. Patient underwent ventriculo-peritoneal shunt on the second day of admission [Table/Fig-2]. Patient’s condition remained the same even after surgery. She eventually succumbed after four days of admission. One hour before her death she developed Cheyne stokes pattern of respiration [Video-1]. Patient consent was taken before taking the video.
CT image depicting hydrocephalus with shunt in situ.
Discussion
Breathing is primarily regulated by feedback of signals from peripheral chemoreceptors i.e., the carotid and aortic bodies that sense changes in the PO2 and PCO2 in the arterial blood and multiple central chemoreceptors in the brain stem, which detect changes in hydrogen ion [4,5]. Hydrogen ion levels at chemoreceptors are determined by cerebral blood flow. Signals from these receptors act on neurons located mainly in the rostral medulla, which cause the respiratory muscles to contract, setting the tidal volume and frequency of breathing. Respiratory control maintains levels of carbon dioxide and oxygen in the blood within narrow limits. Respiratory neurons sense CO2 /H+ changes, and peripheral chemoreceptors sense changes in oxygen level.
Increased ventilation decreases the gas stores of CO2 and reduces PCO2. Similarly opposite effect is seen in decreased ventilation. Oxygen stores are quite small compared to the CO2 stores. The stores of oxygen fall quite rapidly during apnea. The levels of PCO2 and PO2 in the blood are transmitted to the chemoreceptors by the circulation. Apneas occur at low levels of PCO2 in anaesthetized, comatose, and sleeping humans [6-8]. During apnea PCO2 rises and PO2 fall causing ventilation to recover leading to normalcy. Prolongation of the circulation time between the lungs and the brain as well as increased sensitivity of the central and peripheral chemoreceptors can prolong these oscillations, thus producing unstable respiratory control as seen in neurological causes of Cheyne stokes’ breathing.
Cheyne stokes’ breathing has a poor prognosis when occurring in neurologic emergencies like, Cerebrovascular disease, Subarachnoid haemorrhage, Hydrocephalus, Trauma, Cerebral tumour, Meningitis, Encephalitis, Narcolepsy [9-13].
Conclusion
Cheyne stokes’ breathing is an altered pattern of respiration seen in several situations. Its mechanism is complex and primarily mediated through chemo-receptors and levels of PO2 and PCO2 in the arterial blood. In neurology, Cheyne stokes’ breathing is a warning sign of poor prognosis.
Supplementry Material
Supplementary Video-1:
[1]. Cheyne J, A case of apoplexy, in which the fleshy part of the heart was converted into fatDublin Hospital Rep 1818 2:216-23. [Google Scholar]
[2]. Stokes W, The Diseases of the Heart and the Aorta 1854 Dublin, IrelandHodges and Smith:323-24. [Google Scholar]
[3]. Biot MC, Contribution a l’etude du phenomene respiratoire de Cheyne-StokesLyon Med 1876 23:517-28.:56167 [Google Scholar]
[4]. Feldman JL, Mitchell GS, Nattie EE, Breathing: rhythmicity, plasticity, chemosensitivityAnnu Rev Neurosci 2003 26:239-66.10.1146/annurev.neuro.26.041002.13110312598679 [Google Scholar] [CrossRef] [PubMed]
[5]. Cherniack NS, Longobardo GS, Cheyne-Stokes breathing: An instability in physiologic controlN Engl J Med 1973 288(18):952-57.10.1056/NEJM1973050328818104571351 [Google Scholar] [CrossRef] [PubMed]
[6]. Dempsey JA, Skatrud JB, A sleep-induced apneic threshold and its consequencesAm Rev Respir Dis 1986 133(6):1163-70. [Google Scholar]
[7]. Younes M, Ostrowski M, Thompson W, Leslie C, Shewchuk W, Chemical control stability in patients with obstructive sleep apneaAm J Respir Crit Care Med 2001 163(5):1181-90.10.1164/ajrccm.163.5.200701311316657 [Google Scholar] [CrossRef] [PubMed]
[8]. Cherniack NS, Oxygen sensing: Applications in humansJ Appl Physiol 2004 96(1):352-58.10.1152/japplphysiol.00755.200314660496 [Google Scholar] [CrossRef] [PubMed]
[9]. Posner JB, Saper CB, Schiff ND, Plum F, Examination of the comatose patient. In: Posner JB, Saper CB, Schiff ND, Plum F, editorsPlum and Posner’s Diagnosis of Stupor and Coma 2007 4th ednNew YorkOxford University Press:38-87.10.1093/med/9780195321319.003.0056 [Google Scholar] [CrossRef]
[10]. Rowat AM, Wardlaw JM, Dennis MS, Abnormal breathing patterns in stroke: relationship with location of acute stroke lesion and prior cerebrovascular diseaseJ Neurol Neurosurg Psychiatry 2007 78:277-79.10.1136/jnnp.2006.10222817060339 [Google Scholar] [CrossRef] [PubMed]
[11]. Bonnin-Vilaplana M, Arboix A, Parra O, García-Eroles L, Montserrat JM, Massons J, Cheyne-stokes respiration in patients with first-ever lacunar strokeSleep Disord 2012 2012:25789010.1155/2012/25789023471518 [Google Scholar] [CrossRef] [PubMed]
[12]. Parra O, Arboix A, Stroke and sleep-disordered breathing: A relationship under constructionWorld J Clin Cases 2016 4(2):33-37.10.12998/wjcc.v4.i2.3326881189 [Google Scholar] [CrossRef] [PubMed]
[13]. Oliveira MF, Nacif SR, Castellano O, Sousa UO, Rotta J, Pinto F, Improvement of central sleep apneas following ventricular shunt for normal pressure hydrocephalusJ Neuropsychiatry Clin Neurosci 2015 27:e206-08.10.1176/appi.neuropsych.1412037526222970 [Google Scholar] [CrossRef] [PubMed]