Study of Treatment Pattern and Treatment Satisfaction with its Impact on Quality of Life among Psoriasis Patients
Srija Gopal1, Selvalaxmi Gnanasegaran2, Gerard Marshall Raj3, Sakthi Balan Murugesan4, Mangaiarkkarasi Adhimoolam5, Roshini Menon6
1 Postgraduate, Department of Pharmacology, Sri Venkateshwaraa Medical College Hospital and Research Centre, Pondicherry University, Ariyur, Puducherry, India.
2 Postgraduate, Department of Pharmacology, Sri Venkateshwaraa Medical College Hospital and Research Centre, Pondicherry University, Ariyur, Puducherry, India.
3 Assistant Professor, Department of Pharmacology, Sri Venkateshwaraa Medical College Hospital and Research Centre, Pondicherry University, Ariyur, Puducherry, India.
4 Assistant Professor, Department of Pharmacology, Sri Venkateshwaraa Medical College Hospital and Research Centre, Pondicherry University, Ariyur, Puducherry, India.
5 Professor and Head, Department of Pharmacology, Sri Venkateshwaraa Medical College Hospital and Research Centre, Pondicherry University, Ariyur, Puducherry, India.
6 Professor and Head, Department of Dermatology, Venereology and Leprosy, Sri Venkateshwaraa Medical College Hospital and Research Centre, Pondicherry University, Ariyur, Puducherry, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Mangaiarkkarasi Adhimoolam, Professor and Head, Sri Venkateshwaraa Medical College Hospital and Research Centre, Ariyur-605102, Puducherry, India.
E-mail: drmangaimurali@gmail.com
Introduction
Psoriasis is an immune mediated dermatological disorder affecting physical, psychological and social functioning of the individual.
Aim
This study explored the pattern of drug use, quality of life and treatment satisfaction in psoriasis patients and to ascertain whether the satisfaction varies among different treatments.
Materials and Methods
This cross-sectional study was conducted among 50 psoriasis patients, age group more than 18 years of both the genders, attending the dermatology department in a tertiary care teaching hospital. Quality of life and treatment satisfaction of the psoriatic patients were assessed using Psoriasis Disability Index (PDI) and Psoriasis Treatment Satisfaction Questionnaire (PTSQ) respectively which contained various domains for topical, phototherapy and systemic treatment. Data was analysed with one-way ANOVA by SPSS software version 20.0.
Results
Among the 50 patients, 44% received combination of topical and oral therapy and 24% received all three treatment regimens (topical, oral, phototherapy). Statistical significance was observed with PDI assessment with the duration of disease (with six months to one year, >one year) (p<0.001). Mean global satisfaction total score also showed statistical significance with phototherapy when compared with other therapies (p<0.01).
Conclusion
Our study highlighted the effect of different dermatological therapy with high level of satisfaction with phototherapy which can be recommended by the clinicians to the patient who need it. The satisfaction levels of safety among all the three regimens were found to be equal and the Quality of life was impaired as the duration of disease progressed.
Global satisfaction, Phototherapy, Psoriasis disability index, Systemic treatment, Topical, Total score
Introduction
Psoriasis is a chronic and common autoimmune disease affecting approximately 2% of the world’s population [1]. This non contagious disease can negatively impact on the patients’ physical, psychological, and social functioning with men and women being equally affected [2,3]. The impact of psoriasis on the psychological aspect is similar to the chronic diseases like diabetes mellitus and cancer on grounds of severity [4]. Psoriasis is a serious condition strongly affecting the way a person sees himself feeling stigmatized and the way he is seen by others which leads to avoidance of public interaction followed by isolation [5]. Psoriasis has tremendous economic and financial ramifications linked to depression and suicidal tendencies in patients [6]. The current therapy available are topical therapy, phototherapy and systemic therapy. Physicians often start with topical agents, phototherapy, and escalating to systemic anti-psoriatic medications, then to biologicals. Mild forms of the disease may be treated with topical corticosteroids, emollients, coal tar, topical vitamin D3 analogues (calcipotriol) and topical retinoids. While the more extensive form, those resistant to treatment and the more severe forms such as the arthropathic, erythrodermic and pustular forms require systemic treatment [7,8]. The anti-inflammatory, anti-proliferative, vaso-constrictive immunosuppressive properties of topical corticosteroids had made it the first line management for plaque psoriasis [9]. Systemic immunosuppressants usually leads to adverse effects with multi organ involvement. This trial and error process usually frustrates the patient more. The pattern of therapy depends upon the type, severity and duration of the disease. Patient-reported outcomes and patient centered care are being integrated while taking decisions about the treatment for psoriasis [10,11].
There may be wide variations in the pattern of treatment in different geographical areas depending upon the facilities and resources. Non-adherence and treatment dissatisfaction are common with psoriasis patients. Psoriasis ravages the quality of life of affected individuals which is also influenced by the treatment prescribed. In the Indian literature, there are very few analysed data and reports which suggested the physician role in the prescribing of different treatment options with appropriate ones, improving the well-being of the patients by reducing the negative thought about the disease in addition to drug therapy [12,13]. Thus, assessment of the extent of disease in terms of the clinical severity alone by a health professional may not suffice, and a more holistic approach to the quality of life is mandatory. Hence, the present study was designed to explore the pattern of drug use, quality of life and treatment satisfaction in psoriasis patients and to ascertain whether the satisfaction varies between different treatment options.
Materials and Methods
This cross-sectional study was conducted among 50 psoriasis patients attending Dermatology, Venereology and Leprosy department (DVL) (out-patient and in-patient) of a tertiary care teaching hospital in Puducherry over a period of six months (October 2017 to March 2018). Convenient random sampling method was adopted. All psoriasis patients with age group more than 18 years, both male and female irrespective of the disease severity were included in this study. Patients who were not able to comprehend the questionnaire and patients with severe medical diseases which may affect their life quality like chronic obstructive pulmonary disease, liver cirrhosis, heart failure, malignant disease and end stage renal disease were excluded. The study was commenced after obtaining approval from Scientific Research Committee and Institutional Ethics Committee (SVMCH/IEC/2017/49). The study procedure was fully explained to the patients after obtaining the written and informed consent.
A specially designed case record form was used to record the patient details like demographic data (name, age, gender, residential address, occupation) usage of medication, questionnaire for assessment of quality of life and treatment satisfaction. Psoriasis Disability Index (PDI) questionnaire was used to assess the quality of life which consists of 10 questions regarding daily activities, employment, personal relationships, leisure, and treatment effects [12]. The answers for each question were given individual marks (very much: 0, a lot:1, a little:2, not at all:2). Summation of the scores indicated the quality of life. The resulting score ranged between 0-45. The scores were expressed in percentage. Higher the score, the quality of life was more impaired. Similarly treatment satisfaction was assessed using Psoriasis Treatment Satisfaction Questionnaire (PTSQ) with three separate sections for topical therapy, phototherapy, and systemic therapy [14]. Satisfaction scores like global, safety of the medication, convenience and proper information provided by the doctor were assessed among the above three therapies. Answers were graded using a 5- point Likert scale and the possible answers scores are 0-very dissatisfied: 1-dissatisfied: 2-undecided: 3-satisfied: 4-very satisfied. The total score was calculated by summing of each answer and generating the possible range of values ranging from 5-25 which were expressed in percentage for comparison. Higher the total score, poorer the quality of life. The PDI questionnaire and treatment satisfaction were adopted based on the previous studies [12,14]. Both the questionnaires were translated in vernacular language before administration to the patients; the questionnaires were back translated to English language and thus, the validity and reliability were reaffirmed (Cronbach’s alpha:0.8).
Statistical Analysis
Data were entered and analysed using SPSS Software 20.0 version (SPSS, Inc., Chicago, IL). Descriptive statistics were performed, mean and SD were used for summarising numerical values; whereas frequency and percentage for categorical variables. One-way ANOVA followed by post-hoc Tukey test was used to assess the disability index and treatment satisfaction. The p-value <0.05 was considered as statistically significant.
Results
In our study, 52% of the subjects belonged to age group ranging 31-50 years and most of the psoriasis patients belong to the middle class category according to modified BG Prasad’s classification (42%). Around 72% of the patients had no co-morbidities as shown in [Table/Fig-1].
Demographic details of the study population (n=50).
| Demographic data | N (%) |
|---|
| Age (years) |
| 18-30 | 12 (24) |
| 31-50 | 26 (52) |
| >51 | 12 (24) |
| Gender |
| Male | 28 (56) |
| Female | 22 (44) |
| Socio economic status (Modified B.G.Prasad classification) |
| Low | 15 (30) |
| Lower middle | 9 (18) |
| Middle | 21 (42) |
| Upper middle | 3 (6) |
| Upper | 2 (4) |
| Duration of disease |
| < 6 months | 12 (24) |
| 6 months-1 year | 17 (34) |
| > 1 year | 21 (42) |
| Co-morbid conditions |
| Diabetes | 7 (14) |
| Hypertension | 5 (10) |
| Both | 2 (4) |
| Nil | 36 (72) |
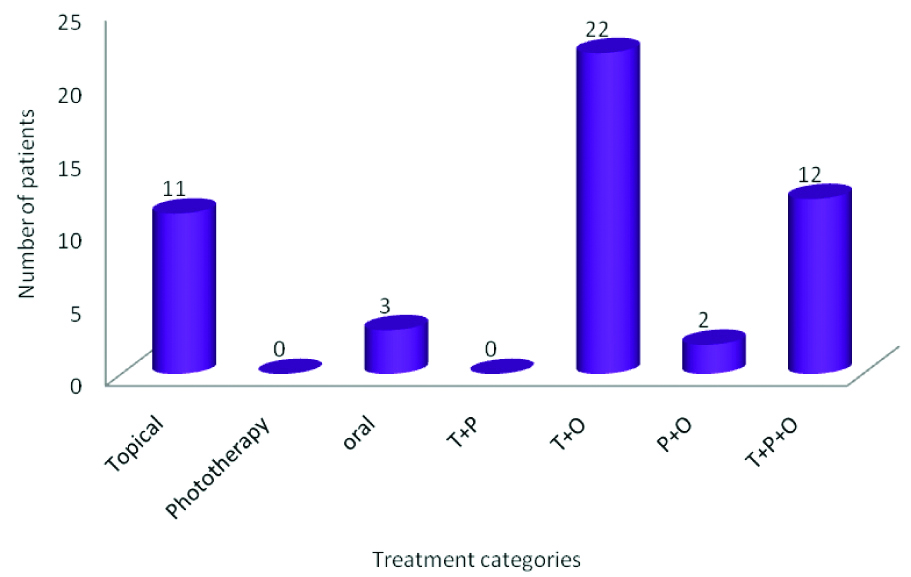
A 44% received combination of topical and oral therapy as represented in [Table/Fig-2]. This study was conducted on 3 main groups which include topical, phototherapy and oral and no patients were taking phototherapy alone at present. [Table/Fig-2] was projected to show the distribution among different treatment regimens and their combination both past and current treatment.
Distribution of different treatment regimens among the psoriasis patient.
T: Topical; O: Oral; P: Phototherapy
As represented in [Table/Fig-3], PDI score was high in psoriasis patients with duration of disease more than six months to one year and more than one year compared to disease duration less than six months. [Table/Fig-4] represents the comparison of different treatment regimens like topical, phototherapy and systemic therapy with treatment satisfaction levels (global, safety, convenience and information provided). The total scores were high with phototherapy when compared to other two therapies (p=0.002).
PDI assessment in comparison with duration of disease.
| Duration of disease | PDI Score Mean±SD | p-value |
|---|
| <6 months | 6.58±2.02 | |
| 6 months-1 year | 9.12±2.73 | 0.001* |
| >1 year | 11.33±4.25 | 0.001* |
Values are expressed in Mean±SD. *p-value <0.001 between the groups
Analysis was done by one-way ANOVA followed by post-hoc Tukey test
Comparison of the individual treatment satisfaction levels among the different combinations. Values are expressed in Mean±SD.
| Satisfaction scores | Topical Therapy (N=45) Mean±SD | Phototherapy (N=14) Mean±SD | Systemic Therapy (N=37) Mean±SD | p-value |
|---|
| Global | 3.61±0.8 | 4.26±0.58 | 3.74±0.80 | 0.021 |
| Safety | 3.47±0.58 | 3.86±0.72 | 3.51±0.54 | 0.078 |
| Convenience | 3.54±0.88 | 4.06±0.86 | 3.30±0.95 | 0.025 |
| Information | 3.63±0.56 | 4.00±0.34 | 3.51±0.63 | 0.019 |
| Total score | 14.22±2.02 | 16.31±2.05 | 13.08±2.36 | 0.002* |
*p<0.01 of the total score in phototherapy when compared with other therapies
Analysis was done by one-way ANOVA followed by post-hoc Tukey test
[Table/Fig-4] shows high satisfaction scores for phototherapy according to their answers for their Treatment Satisfaction Questionnaire (TSQ).
Discussion
Our study highlighted the clinical effect of pattern of different treatment, quality of life and the level of satisfaction among the psoriasis patients treated with topical, phototherapy and systemic therapy. Among the study population (N=50), males and females were 28 and 22 respectively. Patients who received the topical therapy were 45, phototherapy were 14 and systemic therapy were 37 reflecting the maximum number of patients in topical and systemic therapy in our study. This could be due to the severity of the disease as well as location of the lesions. Study done by Horn EJ et al., among the moderate to severe psoriasis patients showed that less than 50% of the patients were receiving systemic therapy similar to our observation [15]. Varma SK et al., studied the pattern of drug prescription in psoriasis patients and analysed most of the patients were effectively treated with topical medications and additional systemic and/or phototherapy were required only for severe cases [16]. The quality of life in psoriasis patients was durable after prolonged use of biologic agents as put forth by Chaptini C et al., [4]. Since psoriasis is a recurrent disease, the affected individuals may experience both disability and significant impairment of quality of life. They were usually assessed by PDI and DLQI questionnaire which is the most often used tools due to their reliability and reproducibility. In this present study, the clinical severity of the disease was measured using PDI questionnaire which showed that the maximum scores were seen with disease duration more than one year when compared to less than one year (p<0.001) indicating the impairment of quality of life in those patients. This was similar to study done by Rakhesh SV et al., who also found a compelling evidence that psoriasis affects the quality of life, and highlighted the importance of adopting a multidimensional assessment of psoriasis [12]. We also observed that 42% of the patients had the disease for more than one year. The present study showed that quality of life was impaired as the duration of disease progressed.
PDI assessment demonstrated greater severity of the disease both physically and mentally but no association between the disease duration and quality of life in a study done by Pakran J et al., contrary to our study [17]. Also, Barot PA et al., showed that DLQI questionnaire scores were high with the section for symptoms and feelings with impaired impacts on the quality of life of the patients [18]. Torres RA et al., demonstrated the quality of life of psoriasis patient by correlating the PDI, PASI and DLQI questionnaire and found out that clinical changes are reflected in the quality of life [19]. The response pattern in our patients could be due to the influence of financial and treatment related problems mostly of the middle (42%) and lower socioeconomic (30%) group.
In addition, the combination of topical and oral treatment perceivers were more than those compared with topical treatments in the form of coal tar, liquid paraffin and steroids which is much better tolerated psychologically and beneficial in our patients.
Our study indicated on the whole that the patients treated with phototherapy were more satisfied when compared to topical and systemic therapy (p=0.002). The global satisfaction for topical and systemic therapy was lower than phototherapy whereas the safety among all the three therapies showed no significant difference. So this shows that phototherapy has been shown to be effective and safe in psoriasis patients. Systemic and topical therapies are lagging behind phototherapy in terms of global satisfaction and convenience. Dissatisfaction with the treatment could lead to discontinuation of the therapy for long-term psoriasis management. Our results were supported by Finch T et al., who found that treatment satisfaction levels were high with phototherapy and systemic treatment whereas global satisfaction levels was significantly lower with topical therapy [14]. Study done by Schaarschmidt M et al., demonstrated that treatment satisfaction of moderate to severe psoriasis showed greater satisfaction for biologicals, followed by traditional systemic medications, phototherapy or topical agents which is in contrary with our study [8]. Yet another study done by Belinchon I et al., also supports the above mentioned observation [20].
Another multicenter study showed 42% of the patients were satisfied with their traditional Chinese or herbal medicines [21]. Our study showed PDI related quality of life has high scores indicating high severity of the disease with poor quality of life. Our observation also showed that treatment satisfaction based on the questionnaire suggesting high level of satisfaction with phototherapy than compared to systemic and topical therapy. The above study provides new insights impacting the quality of life and treatment satisfaction among the patients with psoriasis in our area.
Limitation
Our study limitations include that it was a cross-sectional and single centered study carried out at a tertiary care teaching hospital. However, the present study could provide a basic data for further larger studies with large sample size at different setting level. The patients answers for the satisfaction questionnaire could be based on the recall of previous and current treatment and also the different combinations adopted in the course of treatment.
Conclusion
Our study highlighted the effect of different dermatological therapy in psoriasis patients. The level of satisfaction based on global, convenience of usage and information provided were high with phototherapy. So the clinicians should consider treatment with phototherapy for patients who require the same. The levels of satisfaction with the treatment in terms of safety were equal among all the three regimens and the quality of life was impaired as the duration of disease progressed.
Values are expressed in Mean±SD. *p-value <0.001 between the groups
Analysis was done by one-way ANOVA followed by post-hoc Tukey test
*p<0.01 of the total score in phototherapy when compared with other therapies
Analysis was done by one-way ANOVA followed by post-hoc Tukey test
[1]. Baker EL, Coleman CI, Reinhart KM, Phung OJ, Kugelman L, Chen W, Effect of biologic agents on non-PASI outcomes in moderate-to-severe plaque psoriasis: Systematic review and meta-analysesDermatol Ther. (Heidelb) 2012 2(1):0910.1007/s13555-012-0009-323205332 [Google Scholar] [CrossRef] [PubMed]
[2]. Hjortsberg C, Bergman A, Bjarnason A, Heikkila H, Hjelmgren J, Svensson A, Are treatment satisfaction, quality of life, and self-assessed disease severity relevant parameters for patient registries? experiences from finnish and Swedish patients with psoriasisActa Derm Venereol 2011 91:409-14.10.2340/00015555-109421461549 [Google Scholar] [CrossRef] [PubMed]
[3]. Langham S, Langham J, Goertz HP, Ratcliffe M, Large-scale, prospective, observational studies in patients with psoriasis and psoriatic arthritis: A systematic and critical reviewBMC Medical Research Methodology 2011 11:3210.1186/1471-2288-11-3221453459 [Google Scholar] [CrossRef] [PubMed]
[4]. Chaptini C, Quinn S, Marshman G, Durable dermatology life quality index improvements in patients on biologics associated with psoriasis areas and severity index: A longitudinal studyAustralasian Journal of Dermatology 2015 57(3):e72-e75.10.1111/ajd.1235326010650 [Google Scholar] [CrossRef] [PubMed]
[5]. Dowlatshahi EA, Wakkee M, Arends LR, Nijsten T, The prevalence and odds of depressive symptoms and clinical depression in psoriasis patients: A systematic review and meta-analysisJournal of Investigative Dermatology 2014 134(6):1542-51.10.1038/jid.2013.50824284419 [Google Scholar] [CrossRef] [PubMed]
[6]. Russo PA, Ilchef R, Cooper AJ, Psychiatric morbidity in psoriasis: A reviewAustrals J Dermatol 2004 45(3):155-61.10.1111/j.1440-0960.2004.00078.x15250891 [Google Scholar] [CrossRef] [PubMed]
[7]. Michalsen A, Eddin O, Salama A, A case series of the effects of a novel composition of a traditional natural preparation for the treatment of psoriasisJournal of Traditional and Complementary Medicine 2016 6(4):395-98.10.1016/j.jtcme.2015.08.00627774425 [Google Scholar] [CrossRef] [PubMed]
[8]. Schaarschmidt M, Kromer C, Herr R, Schmieder A, Goerdt S, Peitsch WK, Treatment satisfaction of patients with psoriasisActa Derm Venereol 2015 95(5):572-78.10.2340/00015555-201125394584 [Google Scholar] [CrossRef] [PubMed]
[9]. Maccari F, Improvement of inflammatory dermatoses severity and quality of life in patients treated with a betamethasone valerate plaster (LIBERE study)Journal of Dermatological Treatment 2016 27(1):59-63.10.3109/09546634.2015.103569225898980 [Google Scholar] [CrossRef] [PubMed]
[10]. Radtke MA, Spehr C, Reich K, Rustenbach SJ, Feuerhahn J, Augustin M, Treatment satisfaction in psoriasis: development and use of the PsoSat patient questionnaire in a cross-sectional studyDermatology 2016 232(3):334-43.10.1159/00044463527073875 [Google Scholar] [CrossRef] [PubMed]
[11]. Ahn SC, Gustafson CJ, Sandoval LF, Davis SA, Feldman SR, Cost effectiveness of biologic therapies for plaque psoriasisAm J Clin Dermatol 2013 14(4):315-26.10.1007/s40257-013-0030-z23696234 [Google Scholar] [CrossRef] [PubMed]
[12]. Rakhesh SV, D Souza M, Sahai A, Quality of life in psoriasis: A study from south IndiaIndian J Dermatol Venereol Leprol 2008 74(6):600-06.10.4103/0378-6323.4510119171982 [Google Scholar] [CrossRef] [PubMed]
[13]. Bhosle MJ, Kulkarni A, Feldman RS, Balkrishnan R, Quality of life in patients with psoriasisHealth and Quality of Life Outcomes 2006 4(1):3510.1186/1477-7525-4-3516756666 [Google Scholar] [CrossRef] [PubMed]
[14]. Finch T, Shim TN, Roberts L, Johnson O, Treatment satisfaction among patients with moderate-to-severe psoriasisJ Clin Aesthetic Dermatol 2015 8(4):26-30. [Google Scholar]
[15]. Horn EJ, Fox KM, Patel V, Chiou CF, Dann F, Lebwohl M, Are patients with psoriasis undertreated? Results of National Psoriasis Foundation surveyJ Am Acad Dermatol 2007 57(6):957-62.10.1016/j.jaad.2007.06.04217706322 [Google Scholar] [CrossRef] [PubMed]
[16]. Varma SK, Sutradhar SD, A cross-sectional study of drug prescription pattern in psoriasis patients attending dermatology and venereology department in a rural tertiary care teaching hospitalInt J Basic Clin Pharmacol 2017 6(8):1987-91.10.18203/2319-2003.ijbcp20173283 [Google Scholar] [CrossRef]
[17]. Pakran J, Riyaz N, Nandakumar G, Determinants of quality of life in psoriasis patients: A cluster analysis of 50 patientsIndian J Dermatol 2011 56(6):689-93.10.4103/0019-5154.9183022345772 [Google Scholar] [CrossRef] [PubMed]
[18]. Barot PA, Brahmbhatt NY, Ninama HV, Kharadi DB, Malhotra SD, Quality of life in patients with psoriasis at a tertiary care teaching hospital- A cross sectional studyNJMR 2015 5(2):93-97. [Google Scholar]
[19]. Torres RA, Silva SA, Magalhaes RF, Morcillo AM, Velho PE, Comparison of quality of life questionnaires and their correlation with the clinical course of patients with psoriasisAn Bras Dermatol 2011 86(1):45-49.10.1590/S0365-0596201100010000521437521 [Google Scholar] [CrossRef] [PubMed]
[20]. Belinchon I, Rivera R, Blanch C, Comellas M, Lizan L, Adherence, satisfaction and preferences for treatment in patients with psoriasis in the European Union: A systematic review of the literaturePatient Preference and Adherence 2016 10:2357-67.10.2147/PPA.S11700627895471 [Google Scholar] [CrossRef] [PubMed]
[21]. Tsai TF, Ho JC, Chen YJ, Hsiao PF, Lee WR, Chi CC, Health-related quality of life among patients with moderate-to-severe plaque psoriasis in TaiwanDermatologica Sinica 2018 36:190-95.10.1016/j.dsi.2018.06.006 [Google Scholar] [CrossRef]