Glans Cyst- A Rare Anomaly
Rama Kishan Saran1, Kiran Mirdha2, Sanya Saran3, Rajendra Prasad Takhar4
1 Associate Professor, Department of Surgery, Dr. S. N. Medical College, Jodhpur, Rajasthan, India.
2 Senior Specialist, Department of Obstetric and Gynaecology, Umaid Hospital and S. N. Medical College, Jodhpur, Rajasthan, India.
3 Student, Geetangali Medical College and Hospital, Udaipur, Rajasthan, India.
4 Associate Professor, Department of Respiratory Medicine, Government Medical College, Kota, Rajasthan, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Kiran Mirdha, Senior Specialist, Department of Obstetric and Gynaecology, Umaid Hospital and S. N. Medical College, Jodhpur-342003, Rajasthan, India.
E-mail: 9414803205k@gmail.com
The glans cyst of the penis is an uncommon occurrence and was first described by Lantin and Thompson in 1956. These cysts are generally asymptomatic; however, may present with varied symptoms including dysuria, acute urinary retention, and difficulty in micturition. Cyst may also impact normal anatomy of the penis. Here, we report three cases of glans cyst presenting as slow growing, non-tender, soft cystic swelling measuring 1×1.5 to 2.5×2.5 cm size. The diagnosis of this cyst was made primarily based on physical examination and the management included complete surgical excision. Histopathological examination showed monolocular cystic cavity lined by a pseudo stratified columnar epithelium in two cases and stratified squamous epithelium in the third case.
External urethral meatus cyst, Mucus cyst of the penis, Parameatal cyst, Raphe cyst
Case 1
Parents of a four-year-old child observed slow growing, non-tender, soft cystic swelling of 1×1.5 cm over the glans which was present since birth.
Case 2
A 17-year-old boy had non-tender, soft cystic swelling of 1.8×2.2 cm which was slowly growing since last six months.
Case 3
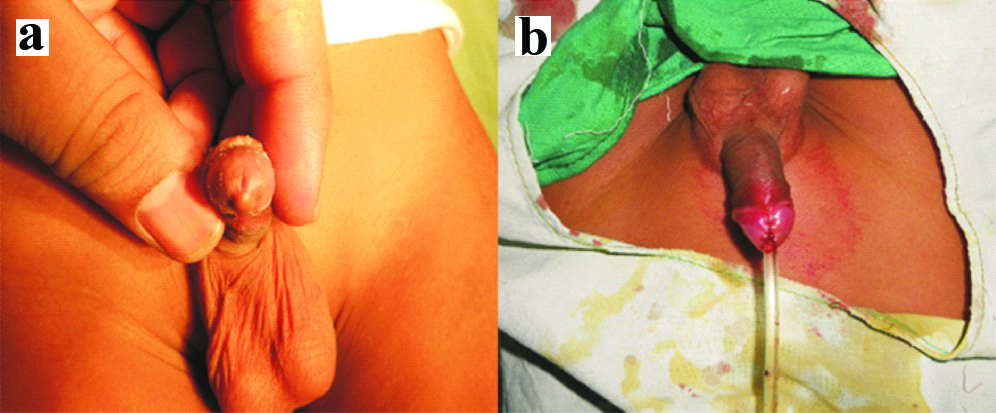
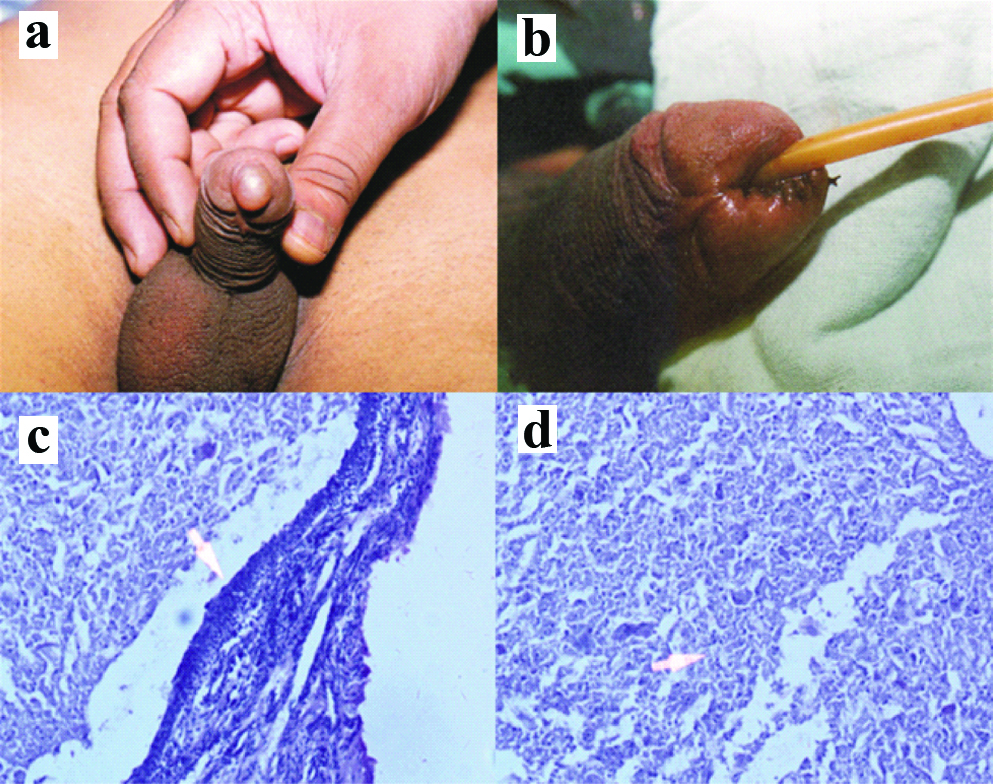
A 22-year-old boy had similar swelling of size 2.5×2.5 cm with mild pain on pressing, which was growing slowly since last one year [Table-Fig-1a,2a and 3a]. There was no history of trauma or penile surgery. General physical and systemic examination was unremarkable. Haemogram, blood biochemistry and urine examination were normal. Diagnosis was based on clinical finding only.
Case 1 (a) parameatal cyst; (b) postoperative image.
Case 2 (a) median raphe cyst; (b) postoperative image; (c) cyst lined by pseudostratified columnar epithelium (H&E stain) (arrow); (d) necrotic degenerative material in cyst (arrow).
Case 3 (a) glans cyst; (b) postoperative image.
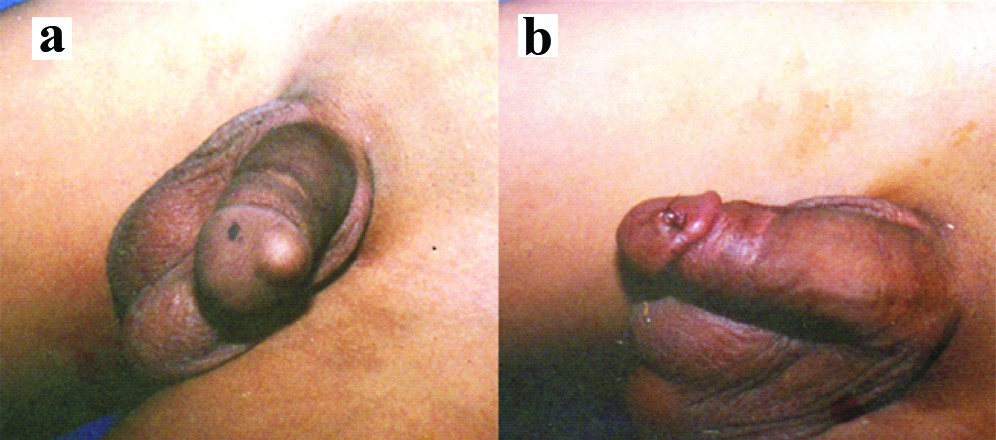
All three patients had complete excision of cyst under spinal anaesthesia (in adult patients) or general anaesthesia (in child Case 1) and the edges were sutured with 4-0/5-0 chromic catgut [Table-Fig-1b,2b and 3b]. Per urethral catheter was kept for 24 hours. Postoperative period was uneventful. Patients were discharged from hospital after first dressing in between second and fifth postoperative day. All three patients passed urine in good stream and urine cultures were sterile. After the surgical excision, good cosmetic results were obtained, without meatal stricture or urine flow problems.
Histopathological examination revealed monolocular cystic cavity lined by a pseudostratified columnar epithelium (Case 1 and 2) and stratified squamous epithelium (Case 3) of varying thickness with no evidence of inflammation, cavity filled with mucus material (Case 1) and necrotic degenerative material (Case 2 and 3) [Table-Fig-2c,d]. No recurrence was observed at the one-year follow-up.
Discussion
The glans cyst of the penis is uncommon benign lesion which affects young men [1,2]. Various terms used to describe glans cyst include mucus cyst of the penis, raphe cyst, parameatal cyst, and hidrocystoma [3]. Glans cyst was first described by Thompson IM and Lantin PM, where they reported two cases and since then several cases have been reported [4]. The [Table-Fig-4] summarises previous reports of glans cyst [5-13].
Summary of previous reports [4-13].
| Author | Age (years) | Size | History | Treatment | Histology |
|---|
| Thompson IM and Lantin PM [4] | 21 | NS | Present since birth without pain. Pain during intercourse. | Simple enucleation under LA | NS |
| NS | NS | Present since birth. Pain during intercourse. | Not removed | NS |
| Kawakami S et al., [5] | 18 | 8×8 mm | First noticed when patient was 16 years old | Excision | Columnar cells |
| 10 | 7×7 mm | Become aware of the cyst 8 month | Excision | Transitional cells |
| 12 | 6×6 mm | Since patient was 6 years old | Excision | NS |
| 9 | 5×5 mm | Cyst for 5 years | Excision | Columnar cells |
| Dini M et al., [6] | 67 | 0.6 cm | Small asymptomatic cystic lesion | Excision | Mucinous columnar cells |
| 22 | 0.75 cm | Present without any symptoms since childhood | Excision | Metaplastic pluristratified epithelium |
| Neeli SI et al., [7] | 12 | 1×1 cm | Present since early childhood | Excision | Columnar epithelium |
| Lal S and Ankur A [8] | 7 | 0.8 cm | Swelling on right side of glans for five months | Excision | Columnar epithelium |
| Nobeyama Y and Nakagawa H [9] | 33 | 5-10 mm (multiple) | 10-year history of slowly growing multiple nodules | NS | NS |
| Sinha RK et al., [10] | 47 | 1×1 cm | Gradually increasing cyst for one and half year | Excision | Squamous and columnar epithelium |
| 4 | 0.5 cm | Increasing swelling for three months | Excision | NS |
| Patil SB et al., [11] | 10 | 1.0×0.8 cm | Increased frequency of micturition (6 months) and burning micturition (1 month) | Excision with meatal reconstruction | NS |
| Shaw SC et al., [12] | Newborn | NS | Small yellowish cystic lesion at tip of penis adjacent to external urethral meatus | None. Discharged with advice to follow-up | - |
| Kaselas C et al., [13] | Newborn (7 days) | NS | Cyst on the urethral meatus | Excision | Squamous epithelium |
| Present cases | 4 | 1×1.5 cm | Present since birth | Excision | Pseudostratified columnar epithelium |
| 17 | 1.8×2.2 cm | Slowly growing since last 6 months | Excision | Pseudostratified columnar epithelium |
| 22 | 2.5×2.5 cm | Slowly growing since last 1 year | Excision | Stratified squamous epithelium |
NS: Not specified
Glans cysts are generally asymptomatic, hence there may be hesitancy in seeking medical help; however, sometimes these may present with symptoms like dysuria, difficulty in micturition and acute retention. Glans cysts may also impact the normal appearance [1-3].
These cysts usually appear spontaneously during the second decade of life but can also present in infants. The aetiology of glans cysts is fully unknown; however, it is thought to be caused due to the obstruction of the paraurethral ducts which could be spontaneous or secondary to infection [7,14,15]. Ichiyanagi N et al., found prostatic-specific antigen in parameatal cysts demonstrating possible role of accessory male sex glands [16]. Another report by Soyer T et al., parameatal cysts in new-born females were found to be associated with vaginal bleeding and enlargement of the breast showing possible role of oestrogen [17].
The Thompson IM and Lantin PM, explained it to be caused due to the persistence of cystic spaces in the separation line of the prepuce from the glans [4]. Different treatment modalities have been reported for the management of glans cysts including waiting for impulsive rupture, marsupialisation, complete removal of the cyst and aspiration with needle [1,2,14,18]. There are less chances of recurrence in patients where complete excision is done. The cysts are generally small (less than 1 cm diameter); however, in present cases the cysts were slightly bigger (1×1.5 cm to 2.5×2.5 cm). Hence, these cases were comparatively rare considering their normal pattern.
Histological examination generally shows different types of epithelium like columnar, transitional, cuboidal or squamous [2]. In the present cases, the cyst wall was lined by a pseudo stratified columnar epithelium/stratified squamous epithelium.
Conclusion
Glans cysts of the penis are uncommon; usually benign and asymptomatic. Only physical examination could be sufficient to make a diagnosis. To obtain good clinical and cosmetic outcomes and to reduce the risk of recurrence complete surgical excision is necessary.
NS: Not specified
[1]. Onaram M, Tan MO, Camtosun A, Irkilata L, Erdem O, Bozkirli I, Parameatal cyst of urethra: A rare congenital anomalyInt Urol Nephrol 2006 38(2):273-74.10.1007/s11255-006-0034-116868696 [Google Scholar] [CrossRef] [PubMed]
[2]. Koga S, Arakaki Y, Mastsuoka M, Ohyama C, Parameatal urethral cysts of the glans penisBr J Urol 1990 65(1):101-03.10.1111/j.1464-410X.1990.tb14668.x2310917 [Google Scholar] [CrossRef] [PubMed]
[3]. Stovall TG, Muram D, Long DM, Paraurethral cyst as an unusual cause of acute urinary retentionJ Reprod Med 1989 34(6):423-25. [Google Scholar]
[4]. Thompson IM, Lantin PM, Parameatal cysts of the glans penisJ Urol 1956 76(6):753-55.10.1016/S0022-5347(17)66761-2 [Google Scholar] [CrossRef]
[5]. Kawakami S, Yamada T, Watanabe T, Negishi T, Parameatal urethral cyst: case reports and review of the literatureUrol Int 1994 53(3):169-71.10.1159/0002826637645147 [Google Scholar] [CrossRef] [PubMed]
[6]. Dini M, Baroni G, Colafranceschi M, Median raphe cyst of the penis: a report of two cases with immunohistochemical investigationAm J Dermatopathol 2001 23(4):320-24.10.1097/00000372-200108000-0000811481524 [Google Scholar] [CrossRef] [PubMed]
[7]. Neeli SI, Patne P, Kadli S, Hiremath S, Parameatal cyst of glans penisJ Sci Soc 2012 39:45-46.10.4103/0974-5009.96476 [Google Scholar] [CrossRef]
[8]. Lal S, Ankur A, Parameatal cyst: a presentation of rare case and review of literatureJ Clin Diagn Res 2013 7(8):1757-58. [Google Scholar]
[9]. Nobeyama Y, Nakagawa H, Case of epidermal cyst on the glans penisJ Dermatol 2013 40(7):575-77.10.1111/1346-8138.1217623663242 [Google Scholar] [CrossRef] [PubMed]
[10]. Sinha RK, Mukherjee S, Mitra N, Saha B, Kumar J, Parameatal cyst: a report of two cases and review of literatureMalays J Med Sci 2015 22(6):71-73. [Google Scholar]
[11]. Patil SB, Patil NA, Kundargi VS, Biradar AN, Para-meatal urethral cyst with bladder calculi: A case report and review of the literatureInt J Appl Basic Med Res 2015 5(3):220-21.10.4103/2229-516X.16537026539378 [Google Scholar] [CrossRef] [PubMed]
[12]. Shaw SC, Vinod MS, Devgan A, Parameatal urethral cystMed J Armed Forces India 2018 74(1):76-77.10.1016/j.mjafi.2017.02.00729386737 [Google Scholar] [CrossRef] [PubMed]
[13]. Kaselas C, Spyridakis I, Patoulias D, Tsioulas P, Patoulias I, Parameatal urethral cyst in a newborn-a case report and review of the literatureJ Clin Diagn Res 2016 10(1):SD01-02.10.7860/JCDR/2016/16738.703326894139 [Google Scholar] [CrossRef] [PubMed]
[14]. Shiraki IW, Parameatal cysts of the glans penis: A report of 9 casesJ Urol 1975 114(4):544-48.10.1016/S0022-5347(17)67079-4 [Google Scholar] [CrossRef]
[15]. Hill JT, Ashken MH, Parameatal urethral cyst: A review of 6 casesBr J Urol 1977 49(4):323-25.10.1111/j.1464-410X.1977.tb04146.x912259 [Google Scholar] [CrossRef] [PubMed]
[16]. Ichiyanagi N, Shibata T, Matsumura T, Ishimaru H, Sakai K, Immunohistochemical identification of prostate-specific antigen in a parameatal urethral cyst of the glans penisBr J Urol 1998 81(1):170-71.10.1046/j.1464-410x.1998.00353.x9467501 [Google Scholar] [CrossRef] [PubMed]
[17]. Soyer T, Aydemir E, Atmaca E, Paraurethral cysts in female newborns: role of maternal estrogenesJ Ped Adol Gyn 2007 20(4):249-51.10.1016/j.jpag.2007.04.00717673138 [Google Scholar] [CrossRef] [PubMed]
[18]. Fujimoto T, Suwa T, Ishil N, Kabe K, Paraurethral cyst in female newborn: is surgery always advocated?J Pediatr Surg 2007 42(2):400-03.10.1016/j.jpedsurg.2006.10.03017270557 [Google Scholar] [CrossRef] [PubMed]