Histopathological Panorama of Leprosy in a Tertiary Care Hospital of Bihar
Ruchi Sinha1, Mamta Kumari2, Punam Prasad Bhadani3
1 Additional Professor, Department of Pathology/Laboratory Medicine, All India Institute of Medical Sciences, Patna, Bihar, India.
2 Senior Resident, Department of Pathology/Laboratory Medicine, All India Institute of Medical Sciences, Patna, Bihar, India.
3 Additional Professor, Department of Pathology/Laboratory Medicine, All India Institute of Medical Sciences, Patna, Bihar, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Mamta Kumari, R Block, Road No. 1, QNOH/1, Patna-800001, Bihar, India.
E-mail: mdoc659@gmail.com
Introduction
Leprosy also known as Hansen’s disease is one of the oldest disease known to mankind. It is a chronic infectious disease caused by Mycobacterium leprae. It still remains as a major public health problem facing India. Nearly, 60% of all world leprosy cases are reported from India. The spectrum of presentation of leprosy is very wide. Histopathology is an important tool in making a definitive diagnosis. The objective of the study is to describe the histopathological profile of leprosy in the state of Bihar.
Aim
To study the histopathological spectrum of leprosy at a tertiary care centre of Bihar.
Materials and Methods
A retrospective hospital-based study of clinically diagnosed leprosy cases was conducted over a period of 28 months (January 2015 to April 2017). Lesional skin biopsies obtained were fixed, processed and stained with Haematoxylin and Eosin (H&E) followed by Ziehl-Neelsen (ZN) staining. The lesions were classified on microscopy as per Ridley-Jopling classification.
Results
A total of 200 cases were studied. Highest incidence was in the 11 to 30 years age group for both males and females. Males were more affected (M:F=2.4:1). Most common clinical feature was loss of sensation. The commonest reported histopathological type was borderline lepromatous (43%) followed by borderline (17%). Overall ZN staining was positive in 56 (28%) cases.
Conclusion
The spectrum of presentation of leprosy is very wide and there is clinical overlap between different types of leprosy. Histopathology still remains the gold standard for early diagnosis and classification of the disease. Accurate diagnosis forms the backbone for appropriate treatment and preventing deformities and drug resistance.
Histopathology, Leprosy, Skin biopsies
Introduction
Leprosy is one of the oldest diseases known to man. It is a chronic infectious disease caused by Mycobacterium leprae (M. leprae). Hansen’s disease was discovered by Sir Gerhard Armauer Hansen in 1873 [1]. Although, leprosy had already been described in Susruth Samhita (600 BC) [2]. It is a granulomatous disease primarily affecting the skin and peripheral nerves. It can also involve muscles, eyes, bone, testis and internal organs to a varying extent [3]. Clinically and histopathologically presentation of leprosy depends on the host cellular immune response [4]. The diagnosis depends on microscopy and demonstration of Acid Fast Bacilli (AFB) on tissue biopsy [5,6].
With developed programmes and unified approach there have been substantial reduction in the disease burden but leprosy is still one of the major public health problem in India. National Leprosy Eradication Programme (NLEP) has been successful in achieving the target of eliminating leprosy {Prevalence Rate (PR) of <1/10000 population} from India in January 2006 [7]. Despite this, India still alone accounts for nearly 60% world leprosy cases [8]. The scenario in Bihar is far from rosy and the state is still a hotspot for leprosy. Though, Bihar had achieved elimination of leprosy in 2015-2016, it defaulted in 2016-2017 (PR of 1.10/10,000 population). The national PR was 0.66/10,000 population as on 31st March 2017. The state is the topmost contributor of all registered national leprosy cases. Its contribution was 10.62% in 2015-2016 which increased to 14.78% as on 31st March 2017. Bihar also accounted for 16.10% of country’s new cases in 2016-2017 as compared to 12.71% cases in 2015-2016 [9,10]. The Annual New Case Detection Rate (ANCDR) for 2016-2017 was 18.38/100,000 population for Bihar as compared to national ANCDR of 10.71/100,000 population [10]. Out of 38 districts in Bihar, 28 districts reported ANCDR >10/100,000 population and 21 districts have PR of >1/10,000 population [10].
In the absence of treatment leprosy tends to be progressive and can cause permanent damage to skin, nerves, limbs and eyes leading to disfigurement. The disability rate due to leprosy in India was 4.46/million population in 2015-2016 while for 2016-2017 it was 3.94/million population. In Bihar the disability rate was higher being, 5.02/million population in 2015-2016 and 5.38/million population for the year 2016-2017 [9,10]. Hence, histopathological examination remains a cornerstone in the diagnosis and appropriate management of this disease.
This study was conducted as there is a paucity of leprosy related histopathological data from Bihar.
Materials and Methods
A retrospective hospital-based study was conducted in Department of Pathology, All India Institute of Medical Sciences, Patna over a period of 28 months (January 2015 to April 2017). Clinically diagnosed patients of leprosy of all age groups and both sexes were included. A 3 mm lesional skin punch biopsies obtained by dermatologists. These biopsies were formalin-fixed, routinely processed and stained with H&E followed by ZN staining. The lesions were graded as per the Ridley-Jopling classification into tuberculoid leprosy, borderline tuberculoid, borderline, borderline lepromatous and lepromatous leprosy. A new variant of leprosy was described by Wade, known as Histioid leprosy [11].
Results
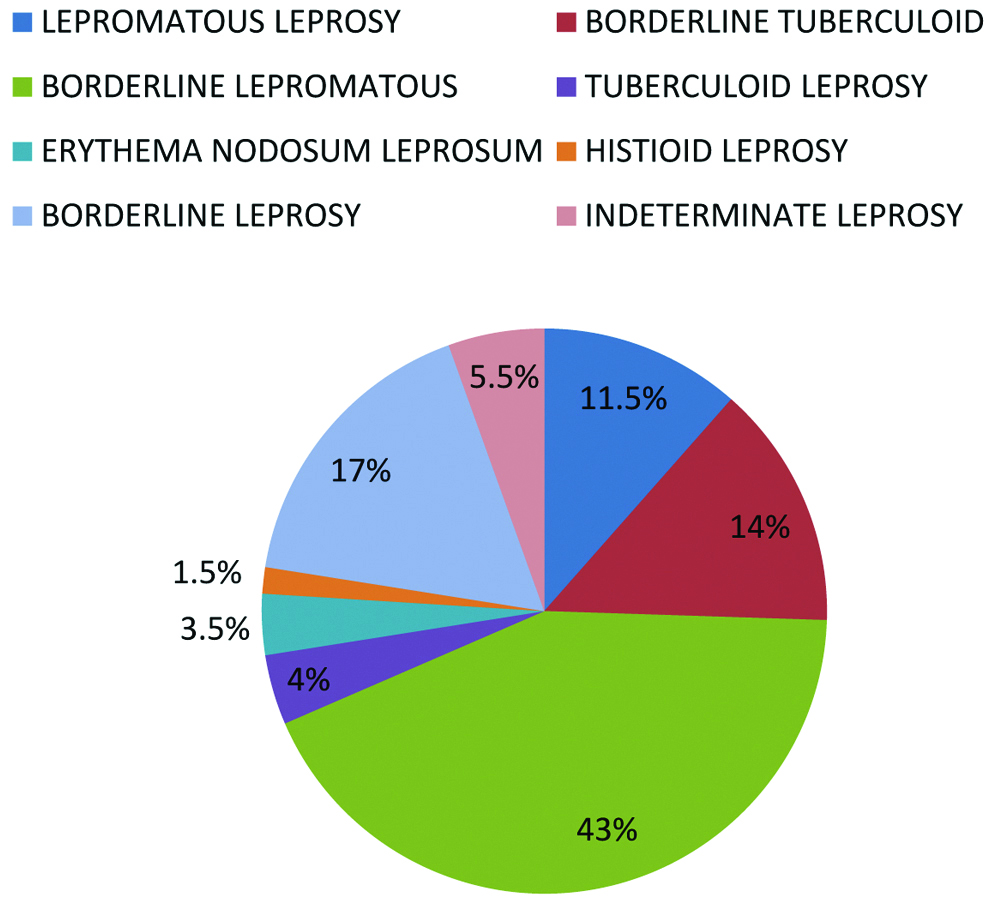
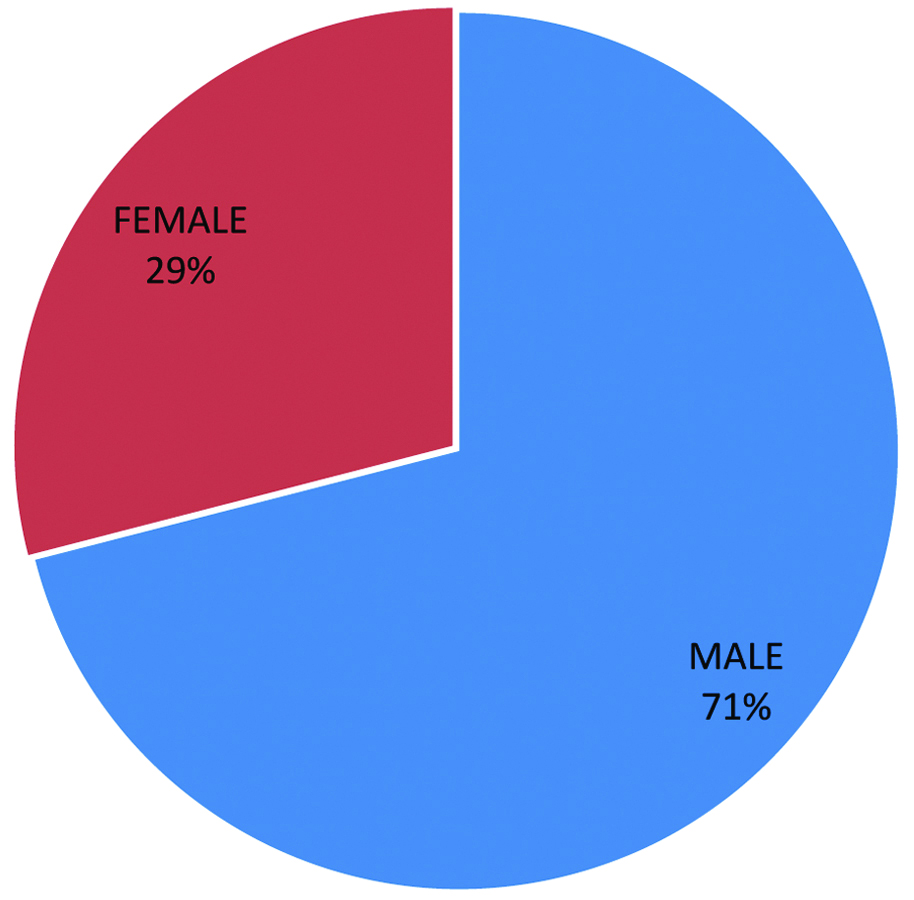
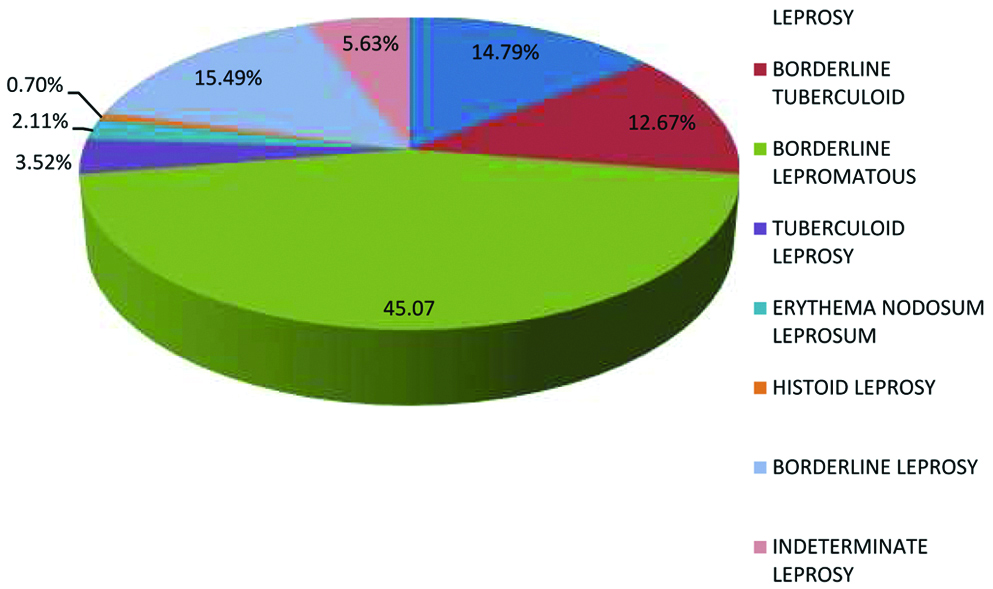
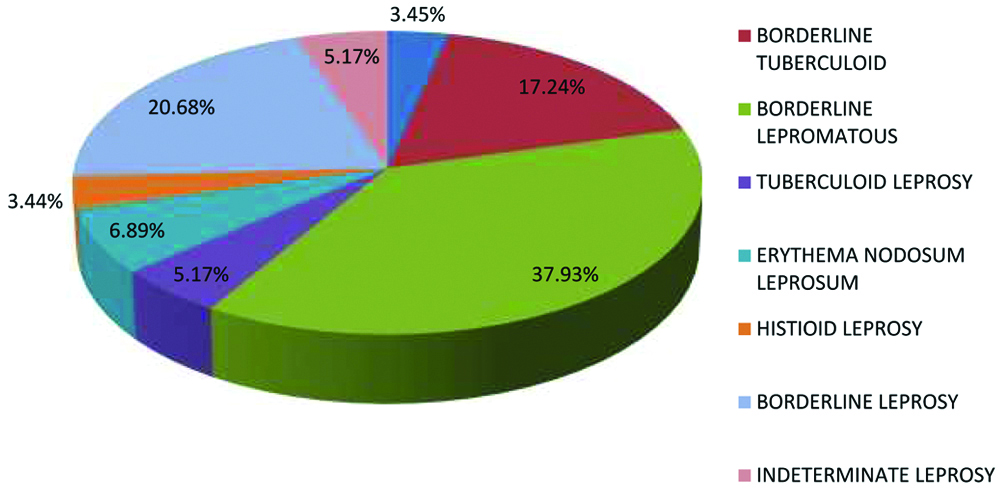
A total of 200 cases were studied. On histopathology, borderline category was the most frequently reported with borderline lepromatous leprosy (43%) being the most common subtype [Table/Fig-1] followed by borderline leprosy (17%). Tuberculoid leprosy (TT) was seen in 4%. Only 1.5% cases of Histioid leprosy were found. There was a male preponderance, with a male to female ratio of 2.4:1 [Table/Fig-2]. Out of 200 cases, 71% were male [Table/Fig-3] and 29% were female [Table/Fig-4]. All subtypes of leprosy were more common in males than females. The age of the patients ranged from 10-80 years [Table/Fig-5] with mean of 25 years. Highest incidence was in the 11-30 years age group. Most common clinical feature was loss of sensation (52.3%). Hypopigmented patches accounted for 20.4% of all cases followed by erythematous skin lesions (14.6%), neural thickening (11.3%) and deformities (1.4%). Overall, ZN staining was positive in 56 cases (28%) with 100% positivity and negativity seen in Lepromatous Leprosy (LL) and BT [Table/Fig-6] cases, respectively. Only 31% cases of BL were positive on ZN stain.
Distribution of histopathological types.
Gender distribution of leprosy case.
Distribution of leprosy cases for males (n=142).
Distribution of leprosy cases for female (n=58).
Distribution of leprosy cases according to age group.
| Age group in year | 1-10 | 11-20 | 21-30 | 31-40 | 41-50 | 51-60 | 61-70 | 71-80 | Total |
|---|
| Lepromatous leprosy | 0 | 4 | 6 | 3 | 5 | 2 | 2 | 1 | 23 |
| Borderline tuberculoid | 2 | 12 | 9 | 2 | 2 | 0 | 1 | 0 | 28 |
| Borderline lepromatous | 1 | 20 | 13 | 18 | 19 | 10 | 5 | 0 | 86 |
| Tuberculoid leprosy | 1 | 3 | 2 | 1 | 0 | 0 | 0 | 1 | 8 |
| Erythema nodosum leprosum | 0 | 1 | 3 | 2 | 0 | 0 | 1 | 0 | 7 |
| Histioid leprosy | 0 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 3 |
| Borderline leprosy | 0 | 5 | 9 | 8 | 5 | 5 | 2 | 0 | 34 |
| Indeterminate leprosy | 0 | 2 | 6 | 1 | 1 | 1 | 0 | 0 | 11 |
Distribution of ZN stain positivity cases among different histopathological type.
| Type | Total cases | Positivity | Percentage (%) |
|---|
| Lepromatous leprosy | 23 | 23 (M=21, F=2) | 100%+ve |
| Borderline tuberculoid | 28 | 0 (M=0, F=0) | 100%-ve |
| Borderline lepromatous | 86 | 27 (M=27, F=0) | 31.39%+ve |
| Tuberculoid leprosy | 8 | 0 (M=0, F=0) | 0% |
| Erythema nodosum leprosum | 7 | 4 (M=2, F=2) | 57.14%+ve |
| Histioid | 3 | 2 (M=1, F=1) | 66.66%+ve |
| Borderline | 34 | 0 (M=0, F=0) | 0% |
| Indeterminate | 11 | 0 (M=0, F=0) | 0% |
| Total | 200 | 56 | 28%+ve |
Discussion
Leprosy is a chronic granulomatous disease caused due to infection by M. leprae. Depending upon the immune status of the host; leprosy can have varied clinico-pathological presentations. Accurate diagnosis and classification are important for correct timely treatment, management and prevention of disabilities. There are various classification systems like India, Madrid, Ridley-Jopling classification, etc., The most widely used Ridley-Jopling classification is based on clinical, bacteriological, pathological and immunological parameters [12]. Indeterminate and histioid subtypes of leprosy were also included in present study. Histopathological examination of skin lesions remains the gold standard for diagnosis [13]. The findings used for microscopic diagnosis are involvement of sub-epidermal zone, granuloma formation, density of lymphocytic infiltrate, nerve involvement, presence of M. leprae and epithelioid cells and other cellular elements in biopsy sections [14].
Leprosy can occur at all ages [15]. In the present study majority of the cases belonged to 11-30 years age group. This is in contrast to other published Indian studies which found most of the cases in 21-40 age groups [16-23]. This is a cause for concern since this is the prime productive age and has economical implications for the nation.
In the present study males were more affected than female. Other studies too have reported a male preponderance [Table/Fig-7] [16-23].
Comparative study of histopathological spectrum of leprosy by different authors with present study.
| Histopathological classification | Kaur S et al., [13] | Kaur I et al., [17] | Giridhar M et al., (2006-2008) [18] | Singh A et al., (2007-2010) [19] | Thapa DP and Jha AK (2008-2012) [25] | Manandhar U et al., (2009-2010) [26] | Bijjaragi S et al., (2010-2011) [27] | Mathur MC et al., [24] | Kakkad K et al., (2011-2014) [22] | Kumar A et al., [20] | Bommakanti J et al., [23] | Agravat AH et al., (2015-2016) [21] | Present study (2015-2017) |
|---|
| TT | 03 | 0 | 14 | 12 | 14 | 10 | 22 | 43 | 04 | 80 | 07 | 21 | 08 |
| LL | 04 | 51 | 16 | 16 | 04 | 10 | 27 | 21 | 16 | 42 | 10 | 33 | 23 |
| BT | 11 | 14 | 42 | 38 | 14 | 30 | 65 | 39 | 20 | 40 | 39 | 17 | 28 |
| BL | 21 | 43 | 08 | 26 | 02 | 14 | 18 | 22 | 08 | 30 | 11 | 22 | 86 |
| IL | 0 | 0 | 18 | 04 | 12 | 04 | 11 | 08 | 0 | 34 | 03 | 01 | 11 |
| BB | 02 | 02 | 0 | 16 | 0 | 04 | 28 | 07 | 02 | 106 | 0 | 0 | 34 |
| HL | 0 | 0 | 0 | 05 | 0 | 0 | 0 | 0 | 0 | 15 | 0 | 02 | 03 |
| ENL | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 76 | 0 | 06 | 07 |
The most common type of leprosy in the present study was BL (43%), followed by BB (17%), BT (14%), LL (11.5%), indeterminate (5.5%), TT (4%), ENL (3.5%) [Table/Fig-8,9 and 10] and Histioid (1.5%). The borderline group constituted the major spectrum (74%) of the disorder which includes BT, BB and BL. There are divergent reports regarding the common subtype of leprosy. Similar findings have been reported by other published Indian papers [13,18-20,22,23]. Contrary to present findings, study conducted by Kaur I et al., observed LL type [Table/Fig-7] to be the commonest type in their series [17] while, Mathur MC et al., found TT to be the most common type [24]. Other set of studies have reported BT as the most frequent histopathogical type [25-27]. This variation could be due to the regional differences, socioeconomic and immune status of the study population [18]. With treatment, borderline group move towards tuberculoid pole and with delayed treatment, it moves towards lepromatous pole [28].
Tuberculoid leprosy (40X).
Borderline tuberculoid leprosy (40X).
Erythema nodosum leprosum (40X).
Various factors influence histopathological diagnosis of leprosy including the size of specimen, biopsy site and depth of biopsy age of lesion, immunological status of patient and treatment history [23]. Serial biopsies from same lesion or from paired lesion help in understanding the disease better [22].
Classification of leprosy cases into paucibacillary and multibacillary variants is important for multidrug treatment. WHO study group (1982) included IL, TT [Table/Fig-8], BT in the paucibacillary spectrum while BB, BL, LL were classified as multibacillary to prevent drug resistance [29]. However, in 1988 WHO expert committee made modification to include only smear negative IL, TT, BT [Table/Fig-9] cases in paucibacillary group and any case belonging to these types with smear positivity are to be typed as multibacillary [30]. Diagnosis of leprosy must be a multidisciplinary effort of the dermatologist, pathologist and microbiologist.
Conclusion
The spectrum of leprosy presentation is very wide. Diagnosing this disease is a challenge. Histopathology plays an important role in making definite diagnosis. It still remains the gold standard for early diagnosis and classification of leprosy. Leprosy is curable with multidrug therapy. Accurate diagnosis is required for proper treatment, preventing deformities and drug resistance. Histopathology, also useful for monitoring treatment response.
In the present study, the most common affected age group was 11-30 years with male predominance is a cause for concern as this is the economically productive group. The predominance of borderline spectrum and multibacillary leprosy could be due to lower socioeconomic status, poor sanitary conditions, overcrowding and illiteracy in the state of Bihar. The findings of this study might help state and centre policymakers to develop more effective strategies for truly achieving the target of eradicating leprosy.
[1]. Tan SY, Graham C, Armauer Hansen (1841-1912): discoverer of the cause of leprosySingapore Med J 2008 49:520-21. [Google Scholar]
[2]. Lowe J, Comments on the history of LeprosyLepr Rev 1947 18:54-63.10.5935/0305-7518.1947001320265196 [Google Scholar] [CrossRef] [PubMed]
[3]. Kumar B, Rai R, Kaur I, Systemic involvement in leprosy and its significanceIndian J Lepr 2000 72:123-42.10.5935/0305-7518.20010011 [Google Scholar] [CrossRef]
[4]. Abulafia J, Vignale RA, Leprosy: Pathogenesis updatedInt J Dermatol 1999 38:321-34.10.1046/j.1365-4362.1999.00650.x10369539 [Google Scholar] [CrossRef] [PubMed]
[5]. Lucus SB, Ridley DS, The use of histopathology in leprosy diagnosis and researchLepr Rev 1989 60:257-62.10.5935/0305-7518.198900312607878 [Google Scholar] [CrossRef] [PubMed]
[6]. Nayak SV, Shivarudrappa AS, Nagarajapa AH, Ahmed SM, Role of modified rapid AFB method in histopathological sections of Hansen diseaseInd Dermatol Venerol Leprol 2003 69:173-74. [Google Scholar]
[7]. Announcement: India achieves national elimination of leprosyIndian J Lepr 2006 78:101 [Google Scholar]
[8]. https://www.who.int/mediacentre/factsheets/fs101/en/ [Google Scholar]
[9]. NLEP–Progress Report for the year 2015-2016. Central Leprosy Division, Directorate General of Health services, Ministry of Health and Family Welfare Government of India, Nirman Bhavan, New Delhi [Google Scholar]
[10]. NLEP Annual Report 2016-2017. Central Leprosy Division, Directorate General of Health Services, Ministry of Health and Family Welfare Government of India, Nirman Bhavan, New Delhi [Google Scholar]
[11]. Wade HW, The histioid leproma AbstractInt J Lepr 1960 28:469 [Google Scholar]
[12]. Ridley DS, Jopling WH, A classification of leprosy for research purposesLepr Rev 1962 33:119-28.10.5935/0305-7518.1962001414492126 [Google Scholar] [CrossRef] [PubMed]
[13]. Kaur S, Sharma VK, Basak P, Kaur I, Radotra BD, Concurrent skin and nerve histology in leprosy and its role in classification of leprosyLepr Rev 1993 64:110-15.10.5935/0305-7518.199300138341113 [Google Scholar] [CrossRef] [PubMed]
[14]. Ridley DS, Jopling WH, Classification of leprosy according to immunity. A five group systemInt J Lepr Other Mycobacterial Dis 1996 34:255-73. [Google Scholar]
[15]. Noorden SK, The epidemiology of leprosy. In: Hastings RC, editor, Leprosy 1985 New YorkChurchill Livingstone:15-29. [Google Scholar]
[16]. Sehgal VN, Ghorpade A, Saha K, Urban leprosy an appraisal from Northern IndiaLepr Rev 1984 55:159-66.10.5935/0305-7518.198400196748847 [Google Scholar] [CrossRef] [PubMed]
[17]. Kaur I, Indira D, Dogra S, Sharma VK, Das A, Kumar B, Relatively spared zones in leprosy: A clinic-pathological study of 500 patientsInt J Lepr 2003 71:227-29.10.1489/1544-581X(2003)71<227:RSZILA>2.0.CO;2 [Google Scholar] [CrossRef]
[18]. Giridhar M, Arora G, Lajpal K, Chahal KS, Clinicohistopathological concordance in leprosy- A clinical, histopathological and bacteriological study of 100 casesIndian J Lepr 2012 84:217-25. [Google Scholar]
[19]. Singh A, Gaur R, Ambey R, Spectrum of leprosy patients with clinico-histopathological correlation: A hospital based studyAsian J Med Science 2013 4:11-16.10.3126/ajms.v4i4.7997 [Google Scholar] [CrossRef]
[20]. Kumar A, Negi SR, Vaishnav K, A study of clinico-histopathological correlation of leprosy in a tertiary care hospital in western district of RajasthanJournal of Research in Medical and Dental Science 2014 2:43-48.10.5455/jrmds.20142310 [Google Scholar] [CrossRef]
[21]. Agravat AH, Dobrariya T, Dhruva GA, A study of histopathological spectrum of leprosyInt J of Scientific Research 2016 5:133-35. [Google Scholar]
[22]. Kakkad K, Padhi T, Pradhan K, Agrawal KC, A study of clinical, bacteriological & histopathological correlation in leprosy cases attending a government medical college in western Odisha: some observationsIndian J Lepr 2016 88:97-103. [Google Scholar]
[23]. Bommakanti J, Putta S, Gokhale S, Histopathological relevance in clinical spectrum of Hansen’s diseaseJMSCR 2016 4:14678-84.10.18535/jmscr/v4i12.61 [Google Scholar] [CrossRef]
[24]. Mathur MC, Ghimire RBK, Shrestha P, Kedia SK, Clinicohistopathological correlation in leprosyKathmandu University Medical Journal 2011 36:248-51.10.3126/kumj.v9i4.6338 [Google Scholar] [CrossRef]
[25]. Thapa DP, Jha AK, Clinico-histopathological correlation in leprosy: a tertiary care hospital based studyOur Dermatol Online 2013 4:294-96.10.7241/ourd.20133.71 [Google Scholar] [CrossRef]
[26]. Manandhar U, Adhikhari RC, Sayami G, Clinico-histopathological correlation of skin biopsies in leprosyJournal of Pathology of Nepal 2013 3:452-58.10.3126/jpn.v3i6.8992 [Google Scholar] [CrossRef]
[27]. Bijjaragi S, Kulkarni V, Suresh KK, Chatura KR, Kumar P, Correlation of clinical and histopathological classification of leprosy in post elimination eraIndian J Lepr 2012 84:271-75. [Google Scholar]
[28]. Jopling WH, McDougall AC, Definition, epidemiology and world distributionThe handbook of leprosy 1996 Ed. 5New DelhiCBS Publishers and Distributors:1-9. [Google Scholar]
[29]. WHO chemotherapy of leprosy for control programmes. WHO Tech Rep Ser. Geneva,WHO;1982;675 [Google Scholar]
[30]. Leprosy: Guidelines for multidrug treatment in endemic districts, National Leprosy Eradication Programme, 1989. Directorate General of Health Services, Ministry of Health and Family Welfare. New Delhi; Govt. of India;1994 [Google Scholar]