Salivary gland lesions are encountered in day-to-day practice and inflammation occurs, which can lead to the development of neoplasm. Fine Needle Aspiration Cytology (FNAC) is a diagnostic technique based on morphologic findings of individuals and group of cells aspirated using a fine needle. FNAC was introduced in the 1920’s and later on it become very populardue to the ease of its performance and rapidity of diagnosis [1]. In today’s era it has become an essential diagnostic investigation. Around the world, the annual incidence of all salivary gland tumour is 0.4-13.5 cases per 100,000 and 0.4-2.6 per 100000 for malignant tumour [2]. Salivary gland tumours usually occur in adults with a slight female predominance, but for unknown reasons Warthin’s tumour occurs more in males. Benign tumours appear in the 5th to 7th decade of life and malignant tumours appear somewhat later [3,4]. These tumours represent less than 2% of tumours in humans and about 65% to 80% arises in parotid, 10% in submandibular, and the remaining in sublingual gland. Pleomorphic adenoma, being the most common neoplasm, represents 60% in parotid [4]. In UPUMS, FNAC of the salivary glands is usually performed on patients during their first clinical visit as an initial procedure for further management of patients. Herein, we have reviewed our seven and half years’ experience in FNAC of salivary glands with the aim to evaluate the diagnostic performance of FNAC for salivary glands lesions in comparison to the histopathological findings with more emphasis on discordant cases, which will result the diagnostic significance of histopathology and finally aid in the treatment of patients.
Materials and Methods
This was a retrospective study carried out at the Department of Pathology, UPUMS, Saifai, Etawah, (UP), India from January 2012 to July 2018. All relevant clinical details were obtained for all the cases in well-designed pro-forma.
The pro-forma was including clinical finding such as age, sex, history of illness, ultrasonography, CT scan finding, cytopathology and histopathology. The sample size was 202, in current study, we have included all those cases of salivary gland pathologies in which the diagnoses was made on the basis of cytopathology or histopathology. Cases of salivary gland swelling diagnosed on FNAC and its correlation with histopathology during that period were included while autolysed biopsies and inadequate FNAC were excluded. In all patients before FNAC, examination of swelling or growth was also done. FNAC was done with 21G needle with suction provided by 10 mL syringe. Smears were prepared and stained with Haematoxyl in and Eosin (H and E), Papanicolaou (Pap) staining and May-Grünwald-Giemsa (MGG) stain. After surgery, specimens were fixed in 10% formalin and send for histopathology examination.
For histopathology, 2-4 μm sections were cut, stained with H&E and screened. All the cytology and histology slides were collected from records reviewed by other three pathologists.
To determine sampling and interpretation errors Intra and inter variability in diagnosis of cases was rarely seen which was excluded with the help of clinical history, diagnostic features and the support of senior pathologists. The histopathological diagnosis is considered as the gold standard for determining the concordance and discordance of the cases to assess sensitivity and specificity of FNAC.
Statistical Analysis
A descriptive study was carried out for all the variables included in the study. The whole data was entered in Microsoft excel master sheet and analysed using SPSS Version 20.0 software. Chi-square will be used to compare the categorical values. Spearman’s correlation coefficient was used to assess the relationship between the two variables. A value of p<0.05 was taken as significant and <0.01 as highly significant whereas p-value>0.05 was taken as non-significant.
Results
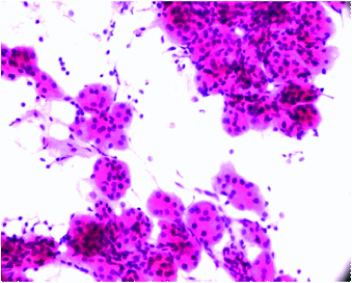
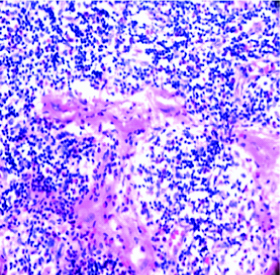
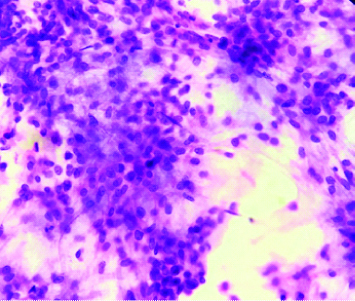
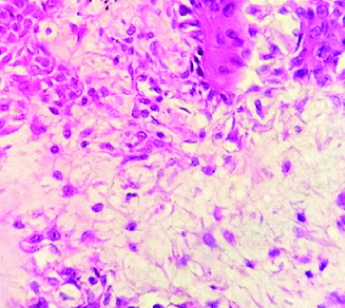
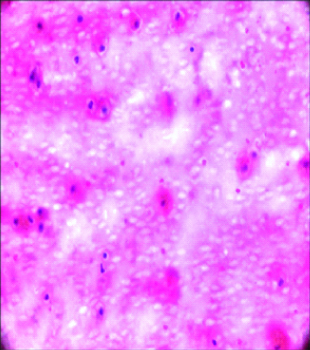
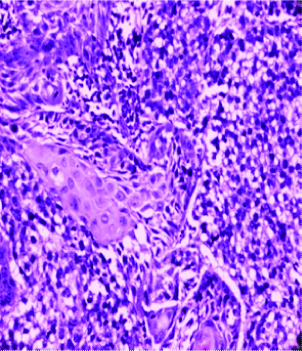
The age of the patients ranged from 7-80 years. FNAC was done in 109 (53.96%) male patients and 93 (46.03%) female patients. Of the 202 cases, 97 (48.01%) were non-neoplastic and among neoplastic lesions, 71 (35.14%) were benign and 34 (16.83%) were malignant on FNAC. Histopathology was carried out in 93 (46.03%) cases. The submandibular gland was a common site for salivary gland lesions in 104 (51.48%) cases and sialoadenitis was a common pathology seen in 71 (35.14%) cases [Table/Fig-1,2]. Pleomorphic adenoma was frequent neoplasm [Table/Fig-3,4]. A cyto-histo concordance was achieved in 80 (39.6%) cases while discordance was seen in 13 (6.43%) cases. Discordorance was seen in majority with Ex carcinoma pleomorphic adenoma followed by mucoepidermoid carcinoma [Table/Fig-5,6]. FNAC showed a sensitivity of 72.41% and specificity of 96%.
H and E (FNA) stained smear of chronic sailoadenitis (H and E, 40X).
H and E stained section of Kuttner’s tumour (H and E, 10X).
MGG (FNA) stained smear of Pleomorphic adenoma (MGG, 40X).
H and E stained section of Pleomorphic adenoma (H and E, 40X).
H and E (FNA) stained smear of cystic lesion of salivary gland (H and E, 40X).
H and E stained section of Mucoepidermoid carcinoma (H and E, 40X).
Discussion
FNAC is a commonly accepted, sensitive and specific technique for the diagnosis of both neoplastic and non-neoplastic lesions of the salivary gland [5]. In present study, the age of the patient ranged from 8-80 year. The maximum number of cases investigated by FNAC was seen between the ages of 41-60 years, which accounted for 83 (41.08%) cases [Table/Fig-7]. This was consistent with other studies [6-8]. Male to female ratio was 1.1:1. The reason behind this might be less number of registration as in rural areas women often come to hospital when their condition is serious or disease was found common in males in present study due to some unknown facts.
Age wise distribution of patients with salivary gland lesions.
| Age distribution | <21 years | 21-40 years | 41-60 years | 61-80 years | Total |
|---|
| Male | 9 | 40 | 48 | 12 | 109 (53.96%) |
| Female | 13 | 42 | 35 | 3 | 93 (46.03%) |
| Total | 22 (10.89%) | 82 (40.59%) | 83 (41.08%) | 15 (7.42%) | 202 (100%) |
The enlargement of salivary gland may occurs due to non-neoplastic lesions which includes a spectrum of disorder ranging from developmental to inflammatory to functional disorders.
Sialoadenitis may occur due to infective agent, stones, malignancy, autoimmune and idiopathic. It was present in 71 (35.14%) cases, while sialoadenitis of the submandibular gland accounted for 55 (77.46%) cases. Similar results were observed by other authors [9,10]. Who also found inflammation of the salivary gland as a common pathology [Table/Fig-8]. Kuttner’s tumour or chronic sclerosing sialadenitis is a chronic inflammatory condition affecting salivary gland which is relatively rare and present as hard indurated mass undistinguishable from tumour. It mainly involves submandibular gland. We also found two cases of kuttner’s tumour in submandibular gland, Sialoadenosis or the non-inflammatory, non-infections and non-tumourous swelling of the salivary gland. It appears in adulthood and can last for decade. Some associated disorders seen are alcohol abuse, breast feeding, bulimia, chemical exposure, diabetes renal failure and thyroid disorders. In present study we found (7.2%) cases of sialoadenosis which was forming a bulk in non-neoplastic disorders after sialoadenitis. The other less common benign disorders were cystic lesions and abscess which was forming (2.9%) and (2.4%) respectively which may be secondary to inflammatory or infective pathology.
Location wise distribution of salivary gland.
| Diagnosis | Parotid gland | Submandibular gland | Sublingual gland | Minor salivary gland | Total |
|---|
| Sialoadenitis | 12 (16.90%) | 55 (77.46%) | 4 (5.63%) | 0 | 71 (35.14%) |
| Sialoadenosis | 6 (40%) | 8 (53.33%) | 0 | 1 (6.66%) | 15 (7.42%) |
| Cystic lesion | 3 (50%) | 3 (50%) | 0 | 0 | 06 (2.97%) |
| Abscess | 2 (40%) | 3 (60%) | 0 | 0 | 05 (2.47%) |
| Pleomorphic adenoma | 42 (68.85%) | 14 (22.95%) | 3 (4.91%) | 2 (3.27%) | 61 (30.19%) |
| Warthin’s tumour | 6 (100%) | 0 | 0 | 0 | 6 (2.97%) |
| Oncocytic lesion | 1 (50%) | 1 (50%) | 0 | 0 | 2 (0.99%) |
| Basal cell adenoma | 0 | 1 (50%) | 0 | 1 (50%) | 2 (0.99%) |
| Mucoepidermoid carcinoma | 6 (66.66%) | 2 (22.22%) | 1 (11.11%) | 0 | 9 (4.45%) |
| Adenoid cystic carcinoma | 2 (40%) | 1 (20%) | 1 (20%) | 1 (20%) | 5 (2.47%) |
| Squamous cell carcinoma | 1 (25%) | 3 (75%) | 0 | 0 | 4 (1.98%) |
| Acinic cell carcinoma | 0 | 0 | 0 | 1 (100 %) | 1 (0.49%) |
| Carcinoma ex pleomorphic adenoma | 2 (100%) | 0 | 0 | 0 | 2 (0.99%) |
| Metastasis | 0 | 13 (100%) | 0 | 0 | 13 (6.43%) |
| Total | 83 (41.08%) | 104 (51.48%) | 9 (4.45%) | 6 (2.97%) | 202 (100%) |
In the present study, 105 (51.98%) cases were diagnosed by FNAC as neoplastic, of which 71 (35.1%) cases were benign and 34 (16.81%) were malignant. This was comparable with other studies [11,12] which also found that benign lesions were more than malignant lesions. Pleomorphic adenoma is a benign mix salivary gland tumour of the major salivary gland, primarily the parotid gland. Among benign tumours, pleomorphic adenoma was seen in 61 (30.19%) cases, while that of the parotid gland, included 42 (20.79%) cases. Present results were consistent with other studies [3,4,12,13]. It was also the frequent tumour which showed maximum concordance [Table/Fig-9].
Cytological and histological correlation (concordance) of salivary gland lesions.
| Diagnosis | Cytopathology | Histopathology |
|---|
| Non-neoplastic | 97 | 15 |
| Acute and chronic sialoadenitis | 71 | 08 |
| Sialoadenosis | 15 | 05 |
| Abscess | 05 | 00 |
| Cystic lesion | 06 | 00 |
| Kuttner | 00 | 02 |
| Benign | 71 | 41 |
| Pleomorphic adenoma | 61 | 34 |
| Basal cell adenoma | 02 | 02 |
| Warthin’s tumour | 06 | 04 |
| Oncocytic tumour | 02 | 01 |
| Malignant | 34 | 24 |
| Adenoid cystic carcinoma | 05 | 03 |
| Mucoepidermoid carcinoma | 09 | 06 |
| Acinic cell carcinoma | 01 | 02 |
| Squamous cell carcinoma | 04 | 02 |
| Pleomorphic adenoma ex carcinoma | 02 | 06 |
| Metastasis (secondary) | 13 | 05 |
Mucoepidermoid carcinoma is composed of a variable mixture of squamous cells, mucus secreting and intermediate cells occasionally focal sebaceous gland, goblet cells also seen. They are the most common form of primary malignant tumour of the salivary glands [14]. In the present study, among malignant cases diagnosed by FNAC, mucoepidermoid carcinoma was present in 9 (4.45%) cases and was the most common malignancy followed by adenoid cystic carcinoma, acinic cell carcinoma, carcinoma ex pleomorphic adenoma, and metastasis.
Discordant diagnoses between cytology and histopathology is common, which occurs due to multiple factors. Cytology details should be carefully examined for scanty cytoplasm, high nucleus to cytoplasmic ratio, naked nuclei, nuclear moulding, and hyperchromasia to avoid erroneous diagnosis among the non-neoplastic lesions Kuttnertumour was also diagnosed as sialoadenitis on cytology.
On cytological examination, discordant pleomorphic adenoma was common, which on histopathological examination was diagnosed as carcinoma ex pleomorphic adenoma, myoepithelioma and adenoid cystic carcinoma. This is a significant misdiagnosis because the cytological smears may have missed evidence of malignancy and it happened as a sampling error rather than interpretative error. However, other causes include marked cellular degeneration and the cytologist not being aware of rare salivary gland lesions. This problem has previously been highlighted by Klijanienko J et al., who found that carcinoma ex pleomorphic adenoma has the highest false negative rate (35.3%) of all malignant salivary gland tumours [15].
Adenoid cystic carcinoma can be misdiagnosed as pleomorphic adenoma on cytological examination, since the fibrillar stroma component and uniform epithelial cells are present in both. Similarly, pleomorphic adenoma can be misdiagnosed as mucoepidermoid carcinoma on cytological examination because aspiration of mucoidpauci cellular fluid may suggest low grade mucoepidermoid carcinoma [14,15]. We also diagnosed a case of mucoepidermoid carcinomaon histology which was found cystic lesion on cytology [Table/Fig-10].
Cases with discordance in cytohistopathological diagnosis.
| Cytological diagnosis | Histopathological diagnosis | Discordantcases |
|---|
| Pleomorphic adenoma | Carcinoma ex pleomorphic adenoma | 4 |
| Pleomorphic adenoma | Myoepithelioma | 1 |
| Mucoepidermoid carcinoma | Pleomorphic adenoma | 1 |
| Cystic lesion | Mucoepidermoid carcinoma | 2 |
| Sialoadenitis | Kuttner tumours | 2 |
| Pleomorphic adenoma | Adenoid cystic carcinoma | 1 |
| Sialoadenosis | Acinic cell carcinoma | 2 |
Acinic cell carcinoma shows cells resembling normal salivary gland cells which lead to false diagnosis of sialoadenosis. However, it is unlikely that acinc cell tumours have fatty element fragments [12].
The present study had a sensitivity of 72.41%, specificity of 96%, positive predictive value of 85.71%, negative predictive value of 87.34%, and diagnostic accuracy of 87.34% [Table/Fig-11], which was comparable with other studies [16-20].
Diagnostic accuracy of FNAC for salivary glands compared with other studies [16-20].
| Studies | Number of cases | Diagnostic accuracy | Sensitivity | Specificity | Positive predictive value | Negative predictive value |
|---|
| Stramandinoli RT et al., [16] | 79 | 82.3% | 68.2% | 87.7% | 68.2% | 87.7% |
| Piccioni LO et al., [17] | 176 | 97% | 81% | 99% | 93% | 98% |
| Stow N et al., [18] | 104 | 92.3% | 86.9% | 92.3% | 96.8% | 86.6% |
| Postema RJ et al., [19] | 380 | 96% | 88% | 99% | 95% | 97% |
| Rehman H et al., [20] | 50 | 78% | 53.28% | 88.57% | 72.7% | 79.9% |
| Present study | 202 | 87.34% | 72.41% | 96% | 85.71% | 87.34% |
Finally, the pitfull of FNAC in salivary gland pathologies are cytological features which sometimes may overlap. However, patient’s history including clinical and radiological examination along with histopathology must be helpful in reaching accurate diagnosis.
Limitation
The limit of this study is less number of salivary gland cases because of less number of patients registrations and histopathology in every case was not possible as patient could not come for surgery.
Conclusion
FNAC is an excellent preliminary diagnostic technique for the diagnosis of salivary gland swelling. However, it may be challenging sometimes especially when cytological features overlaps. Therefore, it is mandatory to use FNAC for primary investigation and it should always be done in conjunction with histopathology along with patient clinical history, physical examination and ultrasonography to reach the correct diagnosis.