Ultrasound Guided Superficial Cervical Plexus and Superior Trunk Interscalene Block as Sole Anaesthetic Technique for Acromioclavicular Joint Fixation Surgery
Anju Annie Paul1, RV Ranjan2, Sagiev Koshy George3, Shishir Murugharaj Suranigi4
1 Senior Resident, Department of Anaesthesiology and Critical Care Medicine, Pondicherry Institute of Medical Sciences, Puducherry, India.
2 Professor, Department of Anaesthesiology and Critical Care Medicine, Pondicherry Institute of Medical Sciences, Puducherry, India.
3 Professor and Head, Department of Anaesthesiology and Critical Care Medicine, Pondicherry Institute of Medical Sciences, Puducherry, India.
4 Professor, Department of Orthopaedics, Pondicherry Institute of Medical Sciences, Puducherry, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Anju Annie Paul, Senior Resident, Department of Anaesthesiology and Critical Care Medicine, Pondicherry Institute of Medical Sciences, Ganapathi Chetikulam, Kalapet-605014, Puducherry, India.
E-mail: anjuannie12@gmail.com
Treating pain that patient experiences from repair of distal clavicle fracture can be a challenge for the anaesthesiolgists. The primary technique employed in the management of distal clavicular surgeries is by incorporating the use of interscalene block. One important factor that reduces the overall effectiveness of the interscalene block is the inability to cover area incised for the surgery due to the dual innervation in this region. While in contrast the use of cervical plexus block for clavicular pain is relatively new, studies have shown that the combination of superficial cervical plexus and selective C5 nerve root blockade under USG is a novel approach to alleviate the pain associated with distal clavicular fracture repair. In this case report, authors describe the use of combination of Ultrasound guided superficial cervical plexus plus superior trunk interscalene block as sole anaesthetic technique in management of right Acromial-clavicular disruption.
Brachial plexus, Clavicular surgeries, Regional anaesthesia
Case Report
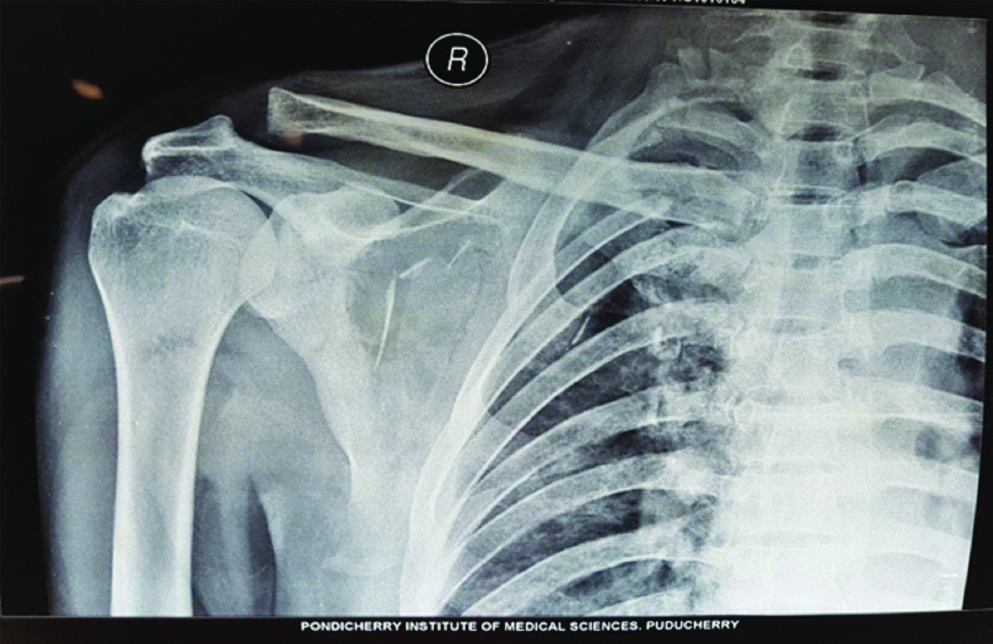
A 40-year-old male sustained a polytrauma following Road Traffic Accident (RTA) resulting in Right distal acromio-clavicular joint disruption, along with, right knee Anterior Cruciate Ligament (ACL) tear, multiple rib fractures, bilateral haemopneumothorax, Para symphyseal fracture of the mandible and crush injury of the right hand [Table/Fig-1].
X-ray right shoulder joint with Acromial-clavicular disruption.
The patient weighed about 70 kg and did not have any significant medical history. Following RTA, he had a Glasgow coma scale (GCS) 15/15, but later developed stridor for which tracheostomy was done on emergency basis and Intercostal drain was placed for the bilateral haemopneumothorax. He underwent facial and hand surgeries under general anaesthesia and was uneventful. The tracheostomy stroma was closed on postoperative day 10 and he was planned for right Acromial-clavicular joint fixation along with ACL reconstruction after 15 days post injury and was graded as ASA II. Airway examination revealed restricted mouth opening with restricted neck extension. After obtaining informed written consent, patient was connected to monitors like non invasive BP, pulse oximeter, electrocardiogram and intravenous access was established on the non-operative side. In view of multiple injuries including facial and chest trauma, doctors decided to avoid general anaesthesia, therefore, the primary plan was subarachnoid block for ACL repair and superficial cervical plexus block plus superior trunk interscalene block as Plan A for clavicular repair, however as a standby we kept the difficult intubation cart including fibro optic bronchoscope prepared.
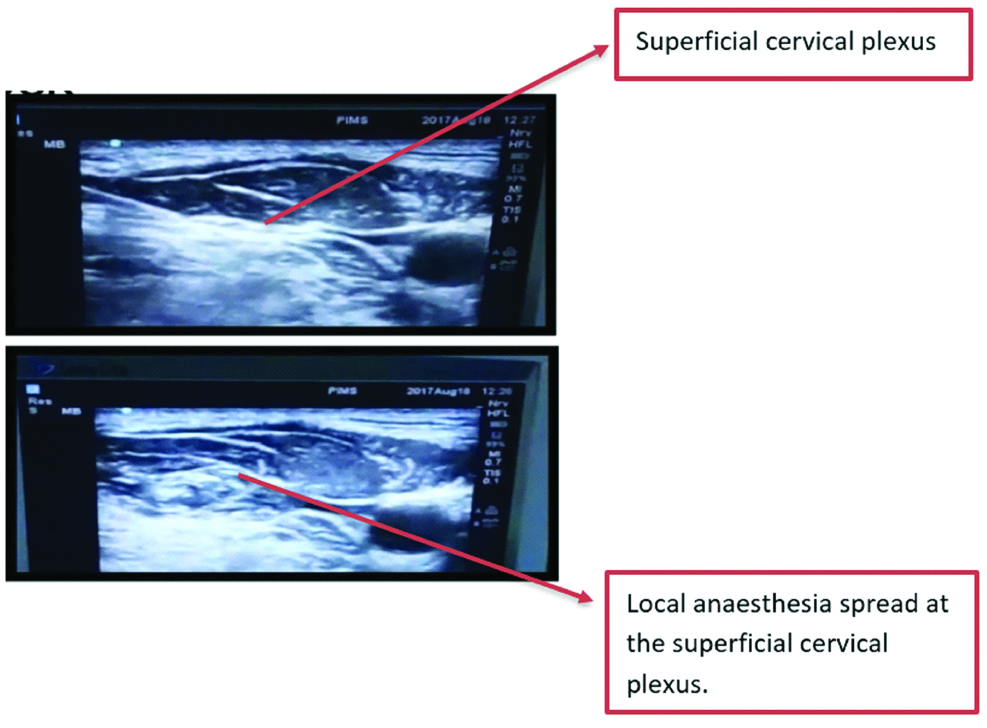
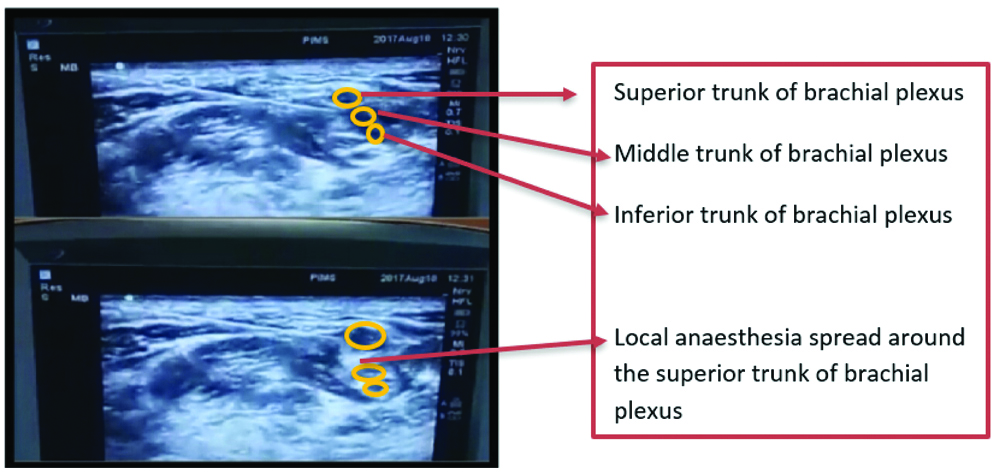
Subarachanoid block was given with 2.6 mL of 0.5% bupivacaine with 30 mcg clonidine for arthroscopic ACL reconstruction. Intraoperative period was uneventful following which ultrasound guided superficial cervical plexus and superior truck interscalene block was given using high frequency linear probe (sonosite). Prior to the start of the procedure Inj. dexmedetomidine was started as a bolus of 1 mcg/kg over 10 minutes followed by 0.2 mcg/kg/minute as infusion throughout the surgery. The superficial cervical plexus block was performed with block needle (stimuplex B Braun) with patient in supine position and head turned to contralateral side [Table/Fig-2]. Posterior border of sternocleidomastoid, internal jugular vein and carotid artery were identified and 5 mL of 0.375% of levobupivacaine was infiltrated at the posterior border of sternocleidomastoid muscle along its tapering posterolateral border but superficial to the prevertebral fascia, after that the USG transducer was placed transversally parallel to the clavicle to identify brachial plexus next to subclavian artery. After identifying brachial plexus transducer, it was moved in cephalad direction till authors identified roots of brachial plexus between scalene muscles. The final target position of the needle was posterior to the space between the C5 and C6 roots [Table/Fig-3] and 12 mL of 0.375% levobupivacaine was deposited around the superior trunk. Sensory blockade was assessed using the pinprick test at the surgery site and also checked for pain with mobilisation of the arm and palpation of the clavicle by the surgeon. The procedure lasted 90 minutes in semi-sitting position with good patient comfort, haemodynamic stability and no demand for additional sedation or analgesics. No clinical signs of respiratory distress were encountered. Patient first experienced pain at eight hours following surgery which was managed by oral Nonsteroidal Anti-inflammatory Drugs (NSAIDS).
In-Plane longitudinal ultrasound view of superficial plexus block.
In-Plane longitudinal ultrasound view of superior trunk interscalene block.
Discussion
Ultrasound in anaesthesia has revolutionised day to day practice. USG guided brachial plexus block have become more successful and sole anaesthetic technique for upper limb surgeries. However, regional anaesthesia for clavicle surgeries has not been practiced much as the clavicle receives multiple innervations. The supraclavicular, subclavian, long thoracic and suprascapular nerves, alone or together, may be responsible for pain transmission after clavicular fracture and post clavicle surgery.
These nerves usually arise from Superficial Cervical Plexus (SCP) and C5 nerve root, through suprascapular nerve and its branches. The cervical plexus gives four terminal branches: greater auricular, lesser occipital, supraclavicular, and transverse cervical nerves. These nerves enter the skin at the middle of the posterior border of the sternocleidomastoid muscle at the level of C3, a point which lies superior to the locus and known as Erb’s point. Chances of failed block are high when landmark techniques are used to block these plexuses. Also, the fear of local anaesthetic toxicity should be kept in mind since it involves two separate plexus blocks. For this reason, general anaesthesia used to be the mainstay for clavicle surgeries whereas superficial cervical plexus block or interscalene blocks were used for post op analgesia for these surgeries [1]. Pal A et al., reported a case of combination of Interscalene Brachial Plexus Block and Superficial Cervical Plexus Block for Fracture Clavicle Surgery in a patient with Dilated Cardiomyopathy, where they used peripheral nerve stimulator to block these plexuses in a dilated cardiomyopathy patient [2]. They had used large volume of 25 mL for interscalene and 10 mL for cervical plexus block; however patient had an uneventful course perioperatively. Kline JP, reported a case of Ultrasound-Guided Placement of Combined Superficial Cervical Plexus and Selective C5 Nerve Root Catheter to treat clavicular pain [3].
Choi SD et al., reported a successful postoperative analgesia after open reduction and internal fixation for clavicle fracture using a cervical plexus block by classic approach using 0.5% bupivacaine which provided 14 hours pain free interval following surgery [4]. Valdés-Vilches LF and Sánchez-del Aguila MJ, has reported a low-volume (1.5-2 mL) selective supraclavicular nerve blockade, together with a low-volume (8-15 mL) brachial plexus supraclavicular approach to achieve adequate depth of blockade for clavicle surgeries [5]. Balaban O et al., reported a retrospective analysis of Ultrasound-Guided Combined Interscalene-Cervical Plexus Block for Surgical Anaesthesia in Clavicular Fractures, where 12 patients underwent surgery for clavicle fracture using same technique as the present case [1]. However, volume of drug used by them was higher (0.5 mL/kg) compared to the present case report. Dillane D et al ., reported the use of combination of blocks guided by ultrasound as a sole technique in a patient undergoing Open Reduction and Internal Fixation (ORIF) for clavicle fracture [6]. Shrestha BR and Sharma P, reported that Interscalene and Superficial cervical plexus block can be used as a technique for procedures on clavicle fracture especially in patients where general anaesthesia is considered unsafe [7]. Ueshima H and Otake H, performed and reported a selective supraclavicular nerve block and fifth, sixth nerve blocks for the clavicular fracture repair in a patient with bilateral pneumothorax using 0.75% levobupivacaine [8]. The present case had multiple injuries with anticipated difficult intubation scenario. Even though all the difficult intubation cart were available, authors did not want to subject the patient for “cannot intubate cannot ventilate scenario”, hence the use of USG guided regional anaesthesia minimised the complications related to intubation and also helped us to use lowest possible volume of local anaesthetic yet providing good surgical anaesthesia.
Conclusion
Combined ultrasound guided Interscalene and Superficial cervical plexus block can be used as an effective technique for clavicle fracture reduction surgeries especially in patients who will have better outcome with avoidance of general anaesthesia. However, prospective randomised studies are required to prove the efficacy of this technique in clavicle surgeries.
[1]. Balaban O, Dulgeroglu TC, Aydin T, Ultrasound-guided combined interscalene-cervical plexus block for surgical anaesthesia in clavicular fractures: a retrospective observational studyAnaesthesiol Res Pract 2018 2018:784212810.1155/2018/784212829973954 [Google Scholar] [CrossRef] [PubMed]
[2]. Pal A, Dawar N, Biswas R, Biswas C, A combination of interscalene brachial plexus block and superficial cervical plexus block for fracture clavicle surgery in a patient with dilated cardiomyopathyIndian Anaesthetists Forum 2011 Special section; 1-3 [Google Scholar]
[3]. Kline JP, Ultrasound-guided placement of combined superficial cervical plexus and selective C5 nerve root catheters: a novel approach to treating distal clavicle surgical painAANA J 2013 81(1):19-22. [Google Scholar]
[4]. Choi DS, Atchabahian A, Brown AR, Cervical plexus block provides postoperative analgesia after clavicle surgeryAnaesth Analg 2005 100(5):1542-43.10.1213/01.ANE.0000149049.08815.0015845732 [Google Scholar] [CrossRef] [PubMed]
[5]. Valdés-Vilches LF, Sánchez-del Aguila MJ, Anaesthesia for clavicular fracture: selective supraclavicular nerve block is the keyReg Anaesth Pain Med 2014 39(3):258-59.10.1097/AAP.000000000000005724747317 [Google Scholar] [CrossRef] [PubMed]
[6]. Dillane D, Ozelsel T, Gadbois K, Anaesthesia for clavicular fracture and surgeryReg Anaesth Pain Med 2014 39(3):256-57.10.1097/AAP.000000000000006124747314 [Google Scholar] [CrossRef] [PubMed]
[7]. Shrestha BR, Sharma P, Regional anaesthesia in clavicle surgeryJNMA: J Nepal Med Assoc 2017 56(206):265-67.10.31729/jnma.3152 [Google Scholar] [CrossRef]
[8]. Ueshima H, Otake H, Successful clavicle fracture surgery performed under selective supraclavicular nerve block using the new subclavian approachJA Clin Rep 2016 2(1):34-36.10.1186/s40981-016-0061-629492429 [Google Scholar] [CrossRef] [PubMed]