Role of Primary Diaphragmatic Repair in Traumatic Diaphragmatic Herniation: Case Series and Review of Literature
JMV Amarjothi1, OLN Babu2, Villalan Ramasamy3, Jeyasudhahar Jesudason4
1 Registrar, Department of Surgical Gastroenterology, Madras Medical College, Chennai, Tamil Nadu, India.
2 Professor, Department of Surgical Gastroenterology, Madras Medical College, Chennai, Tamil Nadu, India.
3 Registrar, Department of Surgical Gastroenterology, Madras Medical College, Chennai, Tamil Nadu, India.
4 Registrar, Department of Surgical Gastroenterology, Madras Medical College, Chennai, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: JMV Amarjothi, 3, Evrsalai, Chennai-3, Tamil Nadu, India.
E-mail: drmosesvikramamarjothi@hotmail.com
Diaphragmatic rupture due to blunt trauma (especially small ruptures) can be effectively treated by primary closure by either laparotomy or laparoscopy with minimal morbidity and mortality. Here, we present a series of cases where the diaphragmatic rupture was managed by primary repair emphasising the role of primary diaphragmatic repair in traumatic rupture. It places a premium on effective early diagnosis of such cases, which is difficult. Though, these injuries may be associated with other organ injuries, early diagnosis and effective treatment are the key to the management of diaphragmatic injuries due to blunt trauma.
Diaphragmatic hernia, Diaphragmatic rupture, Early rupture, Primary repair
Introduction
Traumatic herniation of abdominal contents may occur in the setting of trauma. Early diagnosis of the same may be difficult.
Case Series
A case series of 12 cases (M:F:9:3) of blunt injury causing diaphragmatic hernia is presented. The median time to presentation was 3.5 days (range: 1-10 days). The average size of the defect was 7.25 cm (mean) (range: 3-15 cm), which was on the left side in all the cases. Most common symptom on presentation was breathlessness (91.6%, n=11). As all patients presenting were haemodynamically stable, CT was done in all patients. It identified the defect in all, whereas X-ray chest identified the defect in 75% (n=9). The treatment included open laparotomy (n=7), thoracotomy (in one patient), laparoscopy (in four patients) which was then converted to open after identifying the defect (two patients) and totally laparoscopic (where the defect was closed laparoscopically) in two patients. All patients were treated by hernia content reduction and primary repair of the diaphragm using two layers of reinforced non absorbable prolene sutures. The most common herniated organ included the stomach (n=11) where two had doubtful viability suggestive of perforation necessitating primary closure of the defect in the stomach. Musculoskeletal injuries were seen in three (one-Both bone fracture lower limb, one- humeral fracture left, one-pubic rami fracture) Associated splenic injury was seen in two patients of which one had laceration with haematoma necessitating a splenectomy. Postoperative course was associated with pneumonia (n=3) and intra-abdominal collection (n=3). One patient expired due to sepsis from pneumonia and intra-abdominal sepsis. Mean hospital stay was 14.6 days (8-25 days). On postoperative follow-up of 18 months, there was no recurrence in those who had presented for follow-up [Table/Fig-1,2,3,4,5,6,7,8,9 and 10].
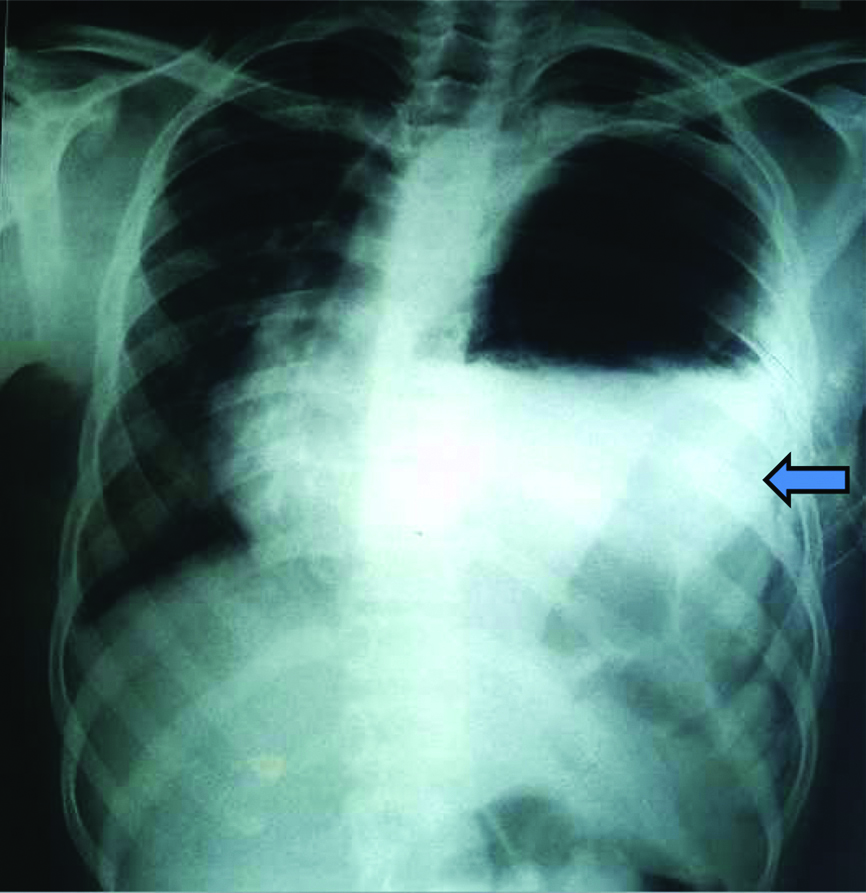
X-ray in traumatic diaphragmatic hernia done showing left lung opacity suggestive of hydropneumothorax (blue arrow).
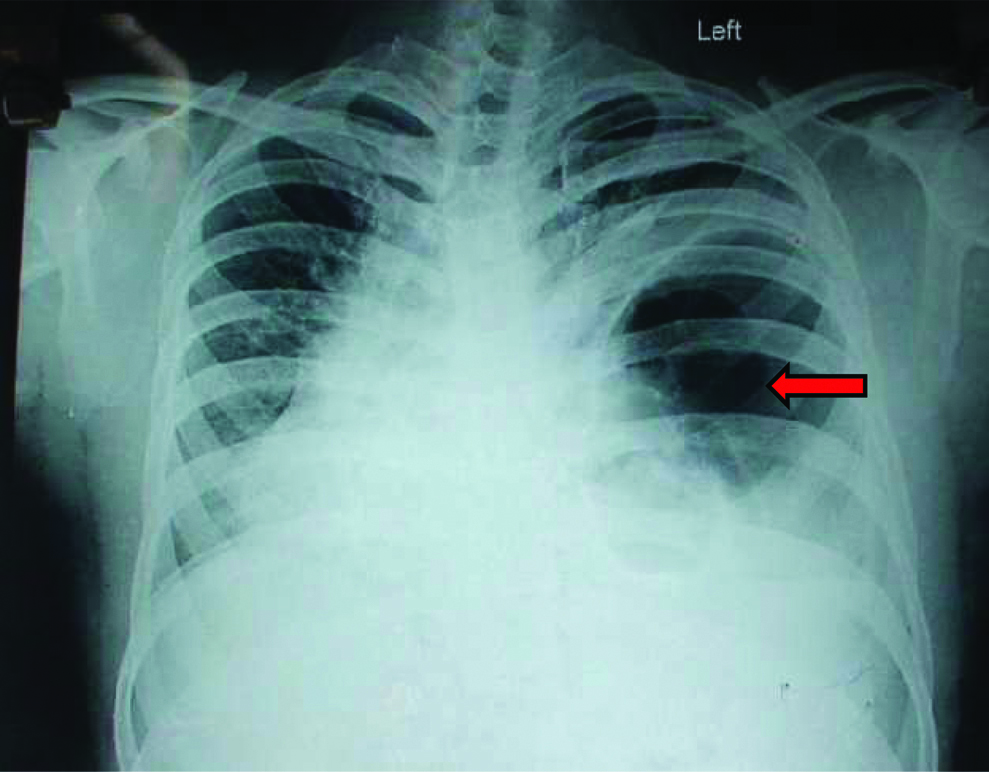
X-ray chest showing dilated bowel loops in the left chest (red arrow).
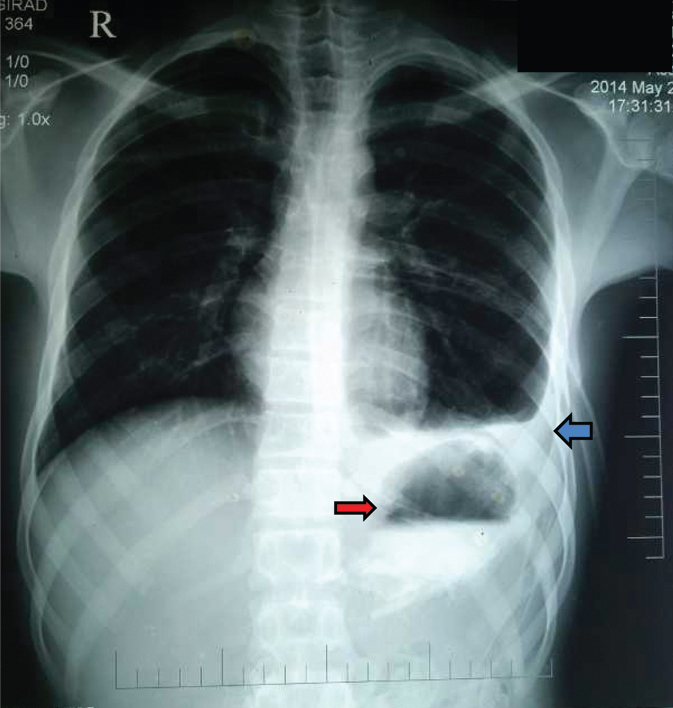
X-ray after primary repair showing normal lung fields with minimal obliteration of left costophrenic angle (blue arrow) and fundic air bubble in abdomen (red arrow).
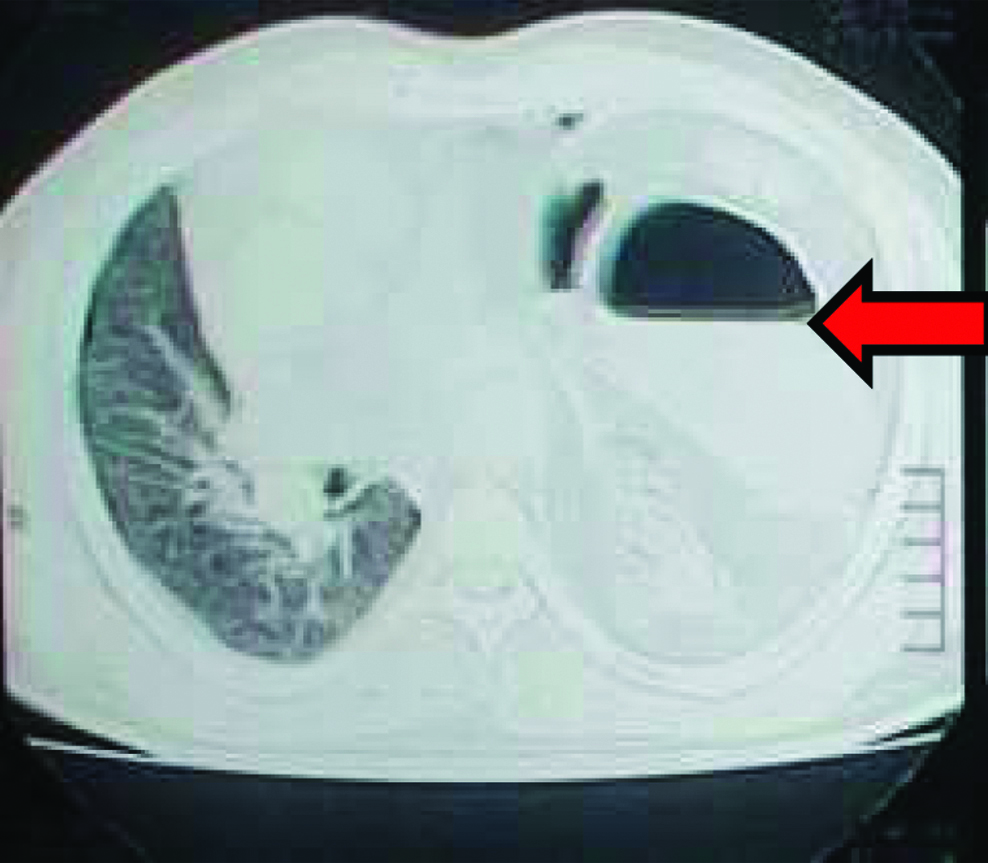
CT of patient showing bowel in thorax (red arrow).
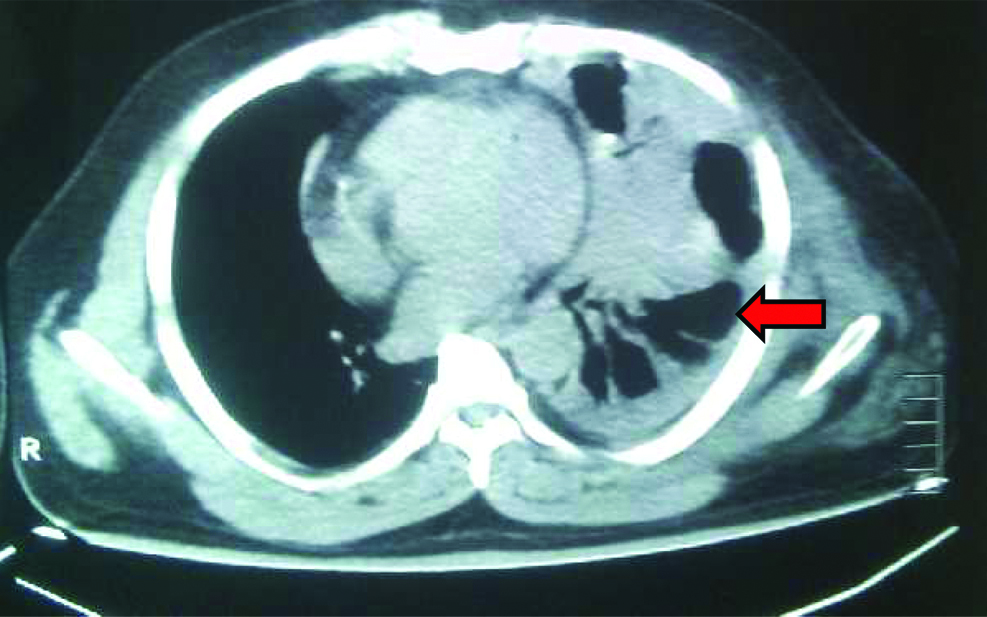
CT showing herniated intraabdominal content into the left chest (red arrow).
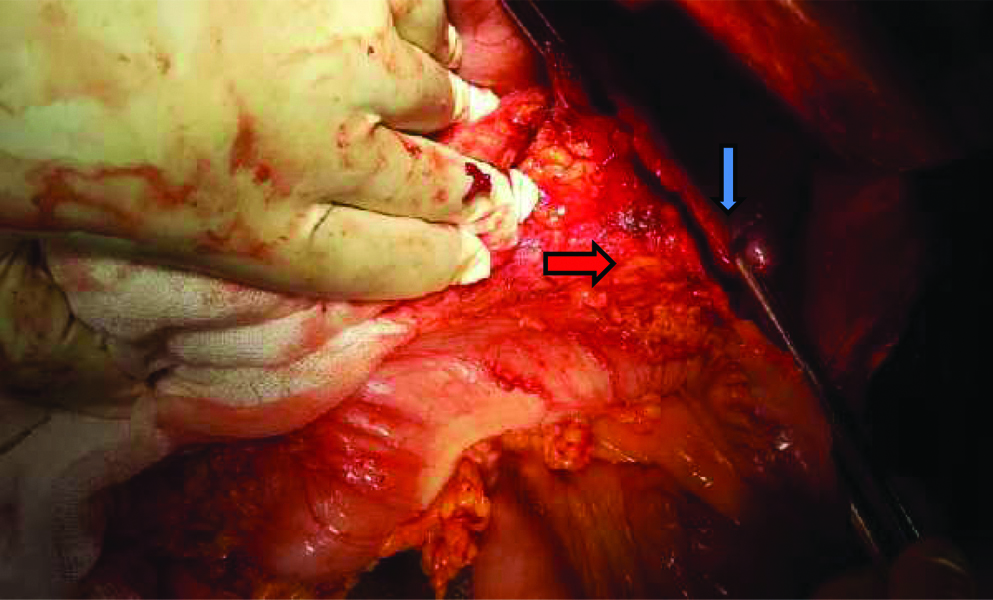
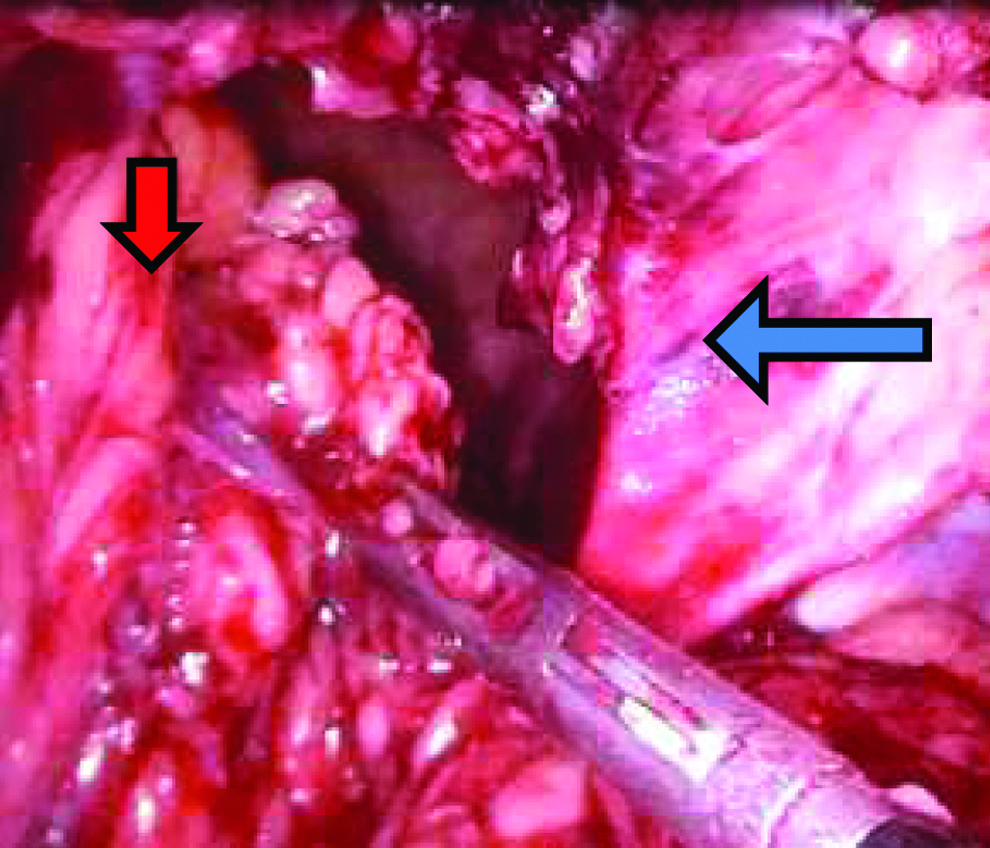
Laparotomy picture showing diaphragmatic tear (in forceps) (blue arrow) with herniated fundus of stomach (red arrow).
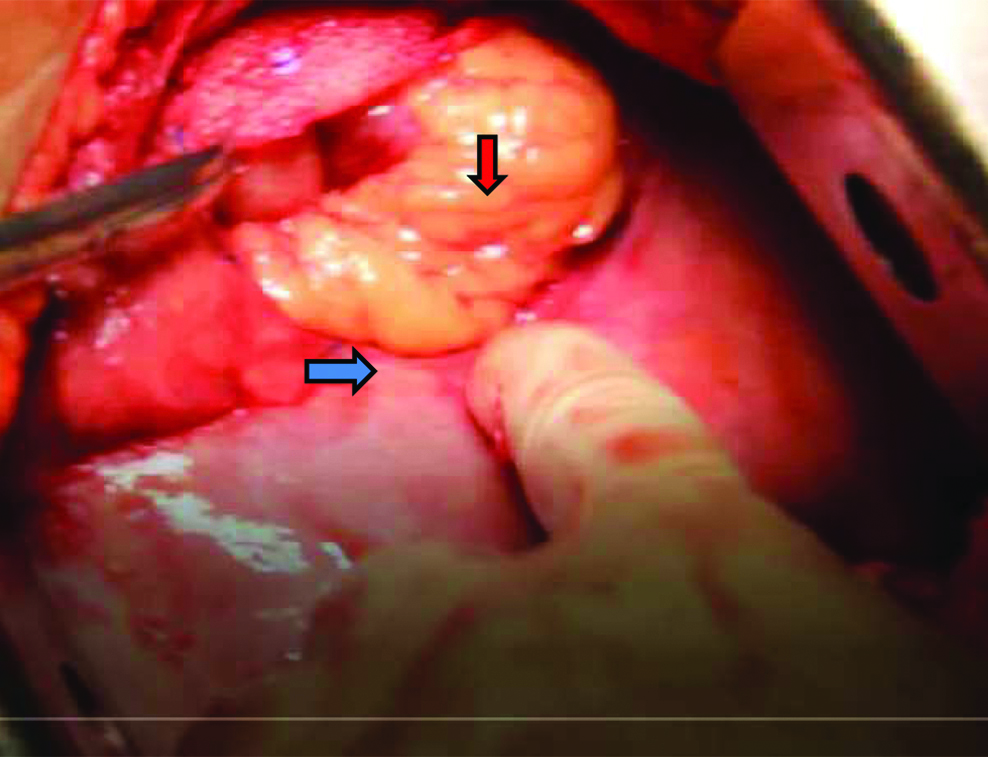
Thoracotomy picture showing diaphragmatic tear (blue arrow) and omentum prolapsing through the defect (red arrow).
Laparoscopic view showing hernial content of omentum (red arrow) in small defect (blue arrow).
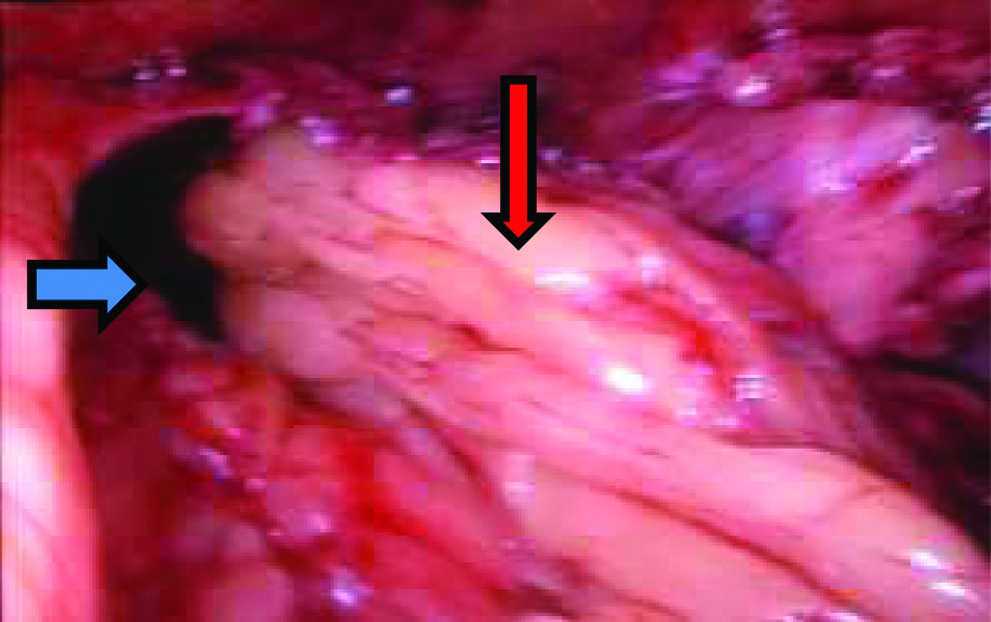
Laparoscopic hernia content of omentum (red arrow) being reduced from defect (blue arrow).
Cases with traumatic diaphragmatic hernia.
| Sex | Age | MOI | AI | TP (days) | SYMP | Size (cm) | Contents | SX | PO | HS (days) |
|---|
| 1 | M | 48 | RTA | FH, LPTX | 6 | B, P | 9 | GO, TC | T-PC | AT, EX | 17 |
| 2 | M | 50 | RTA | LPTX, GP (1.5 cm), FIB | 9 | B, P | 4 | ST | LO-PC, CGP | AT | 14 |
| 3 | M | 45 | RTA | LPTX, SDH, FBBLL | 1 | B, P | 10 | ST, TC, GO | O-PC | | 9 |
| 4 | M | 60 | TT | FLF, LPTX | 2 | P, B | 4 | ST, SP | O-PC, SPY | IOA | 17 |
| 5 | M | 50 | RTA | LPTX | 10 | P | 10 | ST, SP, GO, TC | O-PC | AT | 21 |
| 6 | F | 40 | RTA | LHPTX, GP (3 cm) | 1 | B, P | 4 | ST-P (3 cm) | O-PC, CGP, FJ | | 15 |
| 7 | F | 32 | TT | LPTX | 5 | B | 4 | ST | L-PC | | 8 |
| 8 | M | 28 | FALL | BLPTX, GP (2 cm) | 1 | B, P | 5 | ST-P (2 cm) | O-PC, CGP, FJ | FJ | 25 |
| 9 | M | 26 | RTA | BLPTX | 1 | B | 4 | ST, TC | LO-PC | AT | 14 |
| 10 | M | 30 | RTA | LPTX | 1 | B, P | 15 | ST | O-PC | | 14 |
| 11 | M | 18 | RTA | LPTX | 1 | B, P | 15 | ST, TC, GO | O-PC | IOA | 13 |
| 12 | F | 34 | RTA | LPTX | 4 | B | 3 | ST, GO | L-PC | | 9 |
AI: Associated injuries; AT: Atelectasis; B: Breathlessness; BLPTX: Bilateral pneumothorax; CGP: Closure gastric perforation-primary; EXP: Expired; F: Female; FBBLL: Fracture both bone left leg; FH: Fracture-humerus; FIB: Fracture-illiac bone; FJ: Feeding jejunostomy; GO: Greater omentum; GP: Gastric perforation; HS: Hospital stay; IOA: Intra-abdominal collection; LO-PC: Lap to open primary closure diaphram; L-PC: Lap primary closure-diaphram; LPTX: Left pneumothorax; M: Male; MOI: Mechanism of injury; O-PC: Open primary closure diaphram; P: Abdominal pain; PO: Post operative events; RTA: Road Traffic Accident; SDH: Subdural Haematoma; SP: Spleen; SPY: Splenectomy; ST: Stomach; ST-P: Stomach perforation; SYMP: Symptoms; SX: Surgery done; TC: Transverse colon; TP: Time to presentation after injury; T-PC: Thoracotomy-primary closure diaphram
Discussion
Herniation of abdominal contents into the thorax (seen in 30%) occurs due to sudden increase in the intra-abdominal pressure which may cause a diaphragmatic tear due to devitalisation. This may also be precipitated by mechanical ventilation [1]. The incidence of Traumatic Diaphragmatic Hernia (TDH) is more due to penetrating injury (10-19%) [2], than blunt thoracoabdominal trauma (5%). However, blunt trauma injuries resulting in diaphragmatic herniation are most likely to be missed unless there is a high threshold in searching for the same. TDH occurs in less than 50% of patients with diaphragmatic injuries [3]. Incorrect or late diagnosis is common which is associated with a higher complication rate. The explanation for late diagnosis of traumatic diaphragmatic rupture is delayed detection which occurs due to delayed herniation and co-existing injuries [4]. The most common cause of delayed diagnosis is a diaphragmatic rupture (50%) as seen in the present cases. The most common organ to herniate is the stomach due to close proximity with the exposed left diaphragm, as seen in the present case series [5]. Associated injuries depend on the severity of trauma and include splenic rupture occurring in 25% to 50% of patients with blunt diaphragmatic rupture, followed by liver lacerations in 10% to 50%, pelvic fracture in 30% to 50%, and thoracic aortic tears in 3% to 10% [5]. Associated organ injuries in the present case series were 25% (n=3) and is more of a marker of the level of trauma. Traumtic diaphragmatic hernia can occur in three phases namely acute, delayed and obstructive. Acute phase refers to time of the injury to the diaphragm, delayed phase to transient or reversible herniation of the viscera and obstruction phase, due to long-standing, irreversible herniation [6].
Most of these traumatic herniations (88-95%) occur on the left side and are symptomatic, presenting with respiratory distress [7,8]. It is to be noted that all (100%) of the traumatic diaphragmatic herniation in the present case series were on the left. The increased preponderance of left sided hernias is due to the protective effect of the liver on the right side and greater visualisation of the left diaphragm. Chest X-rays maybe notoriously insensitive for diagnosis of these injuries. In the present case series, 25% of herniations were missed on X-ray. Repetitive chest X-ray increases the accuracy of diagnosis and CT is more accurate in diagnosing the same with all cases being diagnosed by CT in the present case series also [7]. If needed, diagnostic laparoscopy and/or diagnostic thoracoscopy could be performed to improve accuracy further. It is to be noted that peritoneal lavage to detect diaphragmatic injuries, in most large series, has false-negative rates as high as 25% to 34%. In acute setting, laparotomy/laparoscopy is best done which helps not only to reduce the herniated contents but also explore intra-abdominal organs for associated injuries. The surgical treatment includes pleural drainage and repair of the diaphragmatic defect with primary closure or mesh repair. Primary repair with non-absorbable interrupted sutures is an acceptable option in relatively small defects as compared to synthetic mesh in the setting of multiple organ injuries like spleen. In the present case series, all the cases were repaired by primary closure. Mortality is mainly from ischaemic bowel secondary to strangulation which may be as high as 80% [9]. Delayed repair may be associated with atrophy of the diaphragm. In some cases, reinforcement in the form of a flap or prosthesis may be required to close unbridgeable defects [10]. Thoracic approach can be tried for defects in the acute setting provided there is no associated abdominal organ injury and in the delayed setting as there may be adhesions between the herniated contents and thoracic viscera and thoracic approach in this scenario would help in better visualisation [11]. However, it may be associated with high morbidity. Of the 2496 trauma patients in a study, 29 (1.1%) patients underwent thoracotomy which was the most common procedure (in 20 patients) and was associated with an increased morbidity of 24% and mortality of 13.8% [12]. Whether the method of visualisation is by thoracoscopy or laparoscopy, careful visual and manual inspection of the entire diaphragm is necessary to avoid missing diaphragmatic defects.
Conclusion
The responsibility for successful management of traumatic diaphragmatic injuries are heavily predicated on an accurate and early diagnosis in the trauma setting. If diagnosed early, the contents can be reduced and primary diaphragmatic repair using non-absorbable synthetic sutures can be done using laparoscopic or open technique with minimum morbidity and mortality.
AI: Associated injuries; AT: Atelectasis; B: Breathlessness; BLPTX: Bilateral pneumothorax; CGP: Closure gastric perforation-primary; EXP: Expired; F: Female; FBBLL: Fracture both bone left leg; FH: Fracture-humerus; FIB: Fracture-illiac bone; FJ: Feeding jejunostomy; GO: Greater omentum; GP: Gastric perforation; HS: Hospital stay; IOA: Intra-abdominal collection; LO-PC: Lap to open primary closure diaphram; L-PC: Lap primary closure-diaphram; LPTX: Left pneumothorax; M: Male; MOI: Mechanism of injury; O-PC: Open primary closure diaphram; P: Abdominal pain; PO: Post operative events; RTA: Road Traffic Accident; SDH: Subdural Haematoma; SP: Spleen; SPY: Splenectomy; ST: Stomach; ST-P: Stomach perforation; SYMP: Symptoms; SX: Surgery done; TC: Transverse colon; TP: Time to presentation after injury; T-PC: Thoracotomy-primary closure diaphram
[1]. Pappas-Gogos G, Karfis E, Kakadellis J, Tsimoyiannis EC, Intrathoracic cancer of the splenic flexureHernia 2007 11(3):257-59.10.1007/s10029-006-0182-317186114 [Google Scholar] [CrossRef] [PubMed]
[2]. Wadhwa R, Ahmad Z, Kumar M, Delayed traumatic diaphragmatic hernia mimicking hydropneumothoraxIndian J Anaesth 2014 58:186-89.10.4103/0019-5049.13082524963185 [Google Scholar] [CrossRef] [PubMed]
[3]. Hanna WC, Ferri LE, Fata P, Razek T, Mulder DS, The current status of traumatic diaphragmatic injury: Lessons learned from 105 patients over 13 yearsAnn Thorac Surg 2008 85(3):1044-48.10.1016/j.athoracsur.2007.10.08418291194 [Google Scholar] [CrossRef] [PubMed]
[4]. Meyers BF, McCabe CJ, Traumatic diaphragmatic herniaOccult marker of serious injury. Ann Surg 1993 218(6):783-90.10.1097/00000658-199312000-000138257229 [Google Scholar] [CrossRef] [PubMed]
[5]. Meyers B, McCabe CJ, Traumatic diaphragmatic hernia occult marker of serious injuryAnnals of Surgery 1994 218(6):783-90.10.1097/00000658-199312000-000138257229 [Google Scholar] [CrossRef] [PubMed]
[6]. Grimes OF, Traumatic injuries of the diaphragm. Diaphragmatic herniaAm J Surg 1974 128(2):175-81.10.1016/0002-9610(74)90090-7 [Google Scholar] [CrossRef]
[7]. Goh BK, Wong AS, Tay KH, Hoe MN, Delayed presentation of a patient with a ruptured diaphragm complicated by gastric incarceration and perforation after apparently minor blunt traumaCanadian Journal of Emergency Medicine 2004 6(4):277-80.10.1017/S148180350000926X17382006 [Google Scholar] [CrossRef] [PubMed]
[8]. Rashid F, Chakrabarty MM, Singh R, Iftikhar SY, A review on delayed presentation of diaphragmatic ruptureWorld Journal of Emergency Surgery 2009 4:3210.1186/1749-7922-4-3219698091 [Google Scholar] [CrossRef] [PubMed]
[9]. Christie DB, Chapman J, Wynne JL, Ashley DW, Delayed right-sided diaphragmatic rupture and chronic herniation of unusual abdominal contentsJournal of the American College of Surgeons 2007 204(1):17610.1016/j.jamcollsurg.2006.05.00717189127 [Google Scholar] [CrossRef] [PubMed]
[10]. Bernatz P, Burnside AF, Clapett OT, Problem of the ruptured diaphragmJAMA 1958 168:877-81.10.1001/jama.1958.0300007003300713587171 [Google Scholar] [CrossRef] [PubMed]
[11]. Lomanto D, Poon PL, So JB, Sim EW, El Oakley R, Goh PM, Thoracolaparoscopic repair of traumatic diaphragmatic ruptureSurg Endosc 2001 15(3):32310.1007/s00464004201211344439 [Google Scholar] [CrossRef] [PubMed]
[12]. Peer SM, Devaraddeppa PM, Buggi S, Traumatic diaphragmatic hernia-our experienceInternational Journal of Surgery 2009 7:547-49.10.1016/j.ijsu.2009.09.00319778644 [Google Scholar] [CrossRef] [PubMed]