Introduction
Donovanosis is a chronic, sexually transmitted infection caused by gram negative rod-shaped bacterium Calymmatobacterium granulomatis, now known as Klebsiella granulomatis. It is characterised by slowly progressive, painless ulceration with beefy red granulation tissue predominantly over genitalia and inguinal region and the ulcer shows little or no tendency to spontaneous healing [1].
Donovanosis is endemic in tropical regions of the world. The prevalence has decreased but cases are still reported from Papua New Guinea, India, Brazil, Australia and South Africa [2]. In India, it is endemic along the east coast i.e., Orissa, Andhra Pradesh and Tamil Nadu [3]. We hereby report six cases of Donovanosis from Central India registered in two years (January 2016-December 2017).
Case Series
All six cases were subjected to routine investigations such as complete blood counts, liver and renal function tests, urine routine and culture, Venereal Disease Research Laboratory test (VDRL) and Human Immunodeficiency Virus-Enzyme Linked Immuno-Sorbent Assay (HIV-ELISA) test (in healthy subjects) along with gram staining, Ziehl-Nielson (ZN) staining, tzanck smear and tissue smear from ulcer. Biopsy was done only in atypical presentation.
Case 1
A 55-year-old married male, on Antiretroviral Therapy (ART) since four years visited the tertiary care hospital in Central India with complaints of painless raw area over penis since six months which was gradually increasing in size and associated with purulent discharge and bleeding on touch. He gave history of unprotected exposure with a Commercial Sex Worker (CSW) one year back.
Cutaneous examination revealed a single ulcer present over prepuce and shaft of penis. The ulcer was well defined, irregular, 7×5 cm sized, with exuberant, beefy red granulation tissue covered with purulent discharge at floor with raised margins. [Table/Fig-1]. On palpation, the ulcer was non-tender with indurated base and was bleeding easily on touch. Inguinal lymph nodes were not palpable. Oral and anal examination was normal. The cutaneous examination of spouse did not reveal any abnormality. Based on clinical features, differential diagnosis of Donovanosis and Bowen’s disease were being evaluated.
Single, well defined ulcer on penis with beefy red exuberant granulation tissue (Case 1).

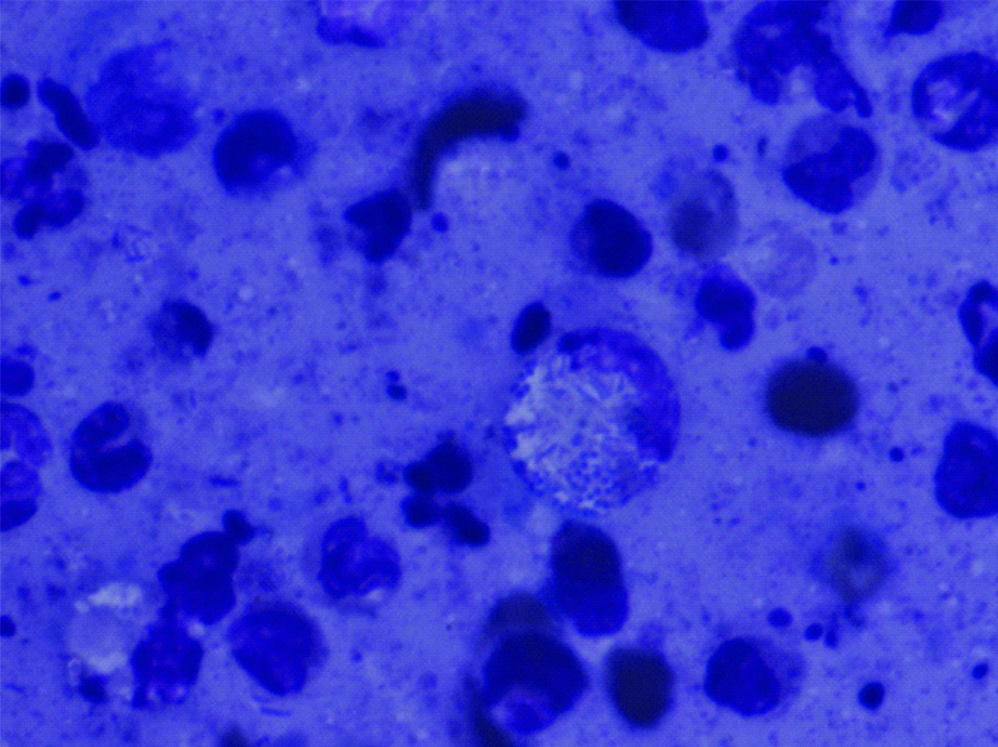
The routine blood and urine investigations were normal. Tzanck smear, Gram’s staining and ZN staining didn’t reveal any abnormality. VDRL was non-reactive. Tissue smear stained with giemsa showed large monocytes with vacuolated cytoplasm containing deeply stained intracytoplasmic inclusion bodies called Donovan bodies [Table/Fig-2]. Based on clinical features and tissue smear report, a final diagnosis of donovanosis was considered.
Tissue smear stained with giemsa showing Donovan bodies.
The patient was started on treatment with oral doxycycline 100 mg twice daily, tablet azithromycin 1 g weekly dose and topical fusidic acid twice daily. After six weeks of treatment, though there was no increase in size, the ulcer didn’t show any signs of healing. Hence intravenous gentamycin 1 mg/kg in 8 hourly doses was started while continuing doxycycline. The healing of ulcer was appreciated beginning from periphery towards the centre and after six weeks of treatment, the ulcer healed completely with dyspigmentation at affected site [Table/Fig-3]. The patient was followed up for a period of six months and genital examination was normal.
Post-treatment image of Case 1 showing healing of ulcer with dyspigmentation.

Case 2
A 34-year-old housewife was on ART since seven years, presented with multiple ulcers involving perianal area with purulent discharge since two months. Patient gave history of extramarital unprotected intercourse three months back. Cutaneous examination revealed well defined, irregularly shaped ulcers with exuberant granulation tissue and purulent discharge present over apposing surfaces of perianal area [Table/Fig-4]. There was no evidence of lymphadenopathy. Differential diagnosis of donovanosis and herpetic ulcers in HIV were considered.
Well-defined ulcers with purulent discharge on apposing surfaces of perianal area (Case 2).

Routine blood and urine investigations were normal and VDRL was non-reactive. Gram staining and tzanck smear were normal. Tissue smear showed donovan bodies on giemsa stain. Considering final diagnosis of donovanosis, patient was treated with oral doxycycline 100 mg twice daily with topical fusidic acid cream twice daily. The ulcers healed with mild superficial scarring after treatment for eight weeks [Table/Fig-5]. Follow-up examination done upto three months was normal.
Post-treatment image of Case 2 showing healing of ulcer with mild superficial scarring.

Case 3
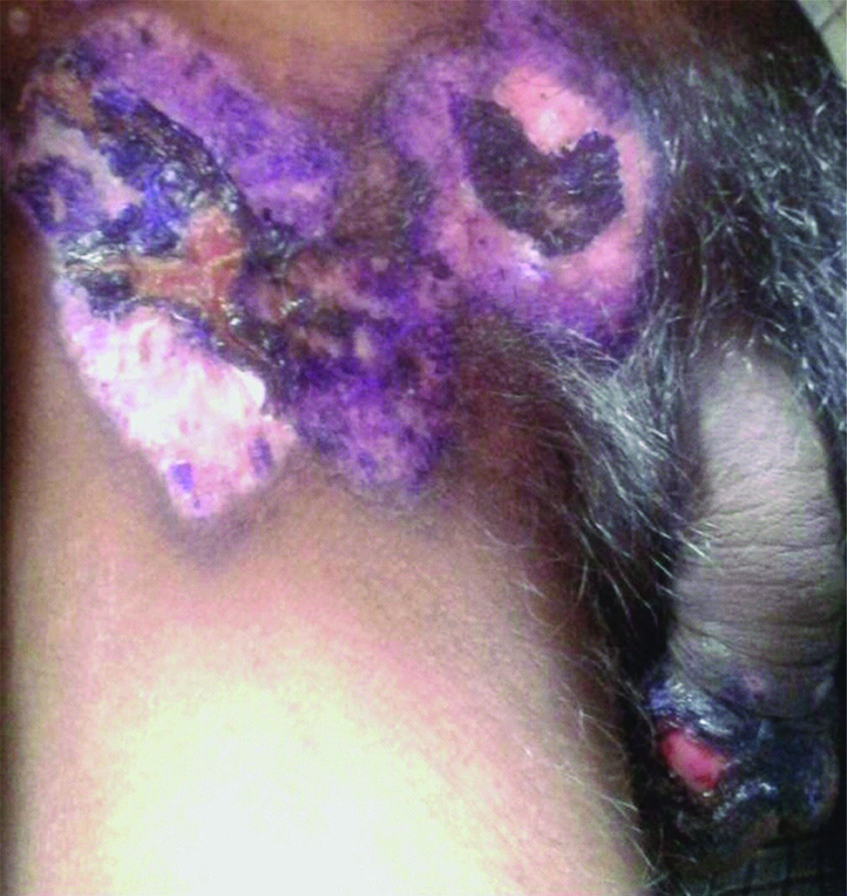
A 35-year-old married male, truck driver by occupation, presented with painless ulcers over penis and groin since three months. The patient gave history of multiple unprotected exposures and was on ART since five years. Cutaneous examination revealed multiple ulcers over glans penis and inguinal area [Table/Fig-6]. The ulcer over inguinal area was well defined, irregular shaped, approximately 15×8 cm with beefy red exuberant floor and raised margins. The ulcer was non-tender and was bleeding easily on touch. Multiple ulcers with similar morphology were present on glans penis and prepuce. Inguinal lymph nodes were non-palpable. Donovanosis and herpes genitalis in HIV were considered as differential diagnosis. Routine blood investigations were normal and VDRL was non-reactive. Tissue smear revealed donovan bodies and tzanck smear was negative.
Multiple ulcers with beefy red granulation tissue on penis and inguinal areas (Case 3).

The patient was treated with oral doxycycline 100 mg twice daily and topical gentian violet for first six weeks. However, there were no signs of healing. Hence intravenous gentamycin 1 mg/kg in 8 hourly doses was added to existing treatment which was continued for another six weeks, but showed no signs of healing. Further, the patient was started on streptomycin 1 g intramuscularly daily along with oral doxycycline 100 mg twice daily for next six weeks. The ulcers healed beginning from periphery towards the centre with formation of crusted erosions, later healing with minimal scarring and dyspigmentation after total 18 weeks of treatment [Table/Fig-7].
Post-treatment image of Case 3 showing healing of ulcer with dyspigmentation and central crusting.
Case 4
A 22-year-old healthy male, presented with asymptomatic ulcer over perineal area with purulent discharge since 15 days. He gives history of treatment with co-amoxiclav in view of furuncle from other clinic, but noticed increase in size. He gave history of unprotected intercourse with CSW two months back. On examination, a single, well defined, ulcer of size 6×3 cm with beefy red granulation tissue, elevated margins and purulent discharge at floor was seen on perineal area [Table/Fig-8]. On palpation, ulcer was non-tender and bleeding easily on touch. Inguinal lymph nodes were non-palpable. HIV and VDRL were non-reactive. Tissue smear showed Donovan bodies. The ulcer responded to treatment with oral doxycycline 100 mg twice daily and topical mupirocin ointment twice daily for four weeks with complete resolution of lesions on further follow-up [Table/Fig-9].
Single well defined ulcer in perineal area with purulent discharge and bleeding (Case 4).

Post-treatment image of Case 4 showing healing of ulcer.

Case 5
A 45-year-old married male, on ART since three years, presented with asymptomatic raised lesion in right groin since six months. Examination revealed a verrucous lesion with dry irregular surface and seropurulent discharge with crusting at central part present over right inguinal area [Table/Fig-10]. On palpation, the lesion was firm and non-tender. Inguinal lymph nodes were non-palpable. Genital examination of spouse was normal. Based on clinical examination, differential diagnosis of genital wart and verrucous granuloma inguinale were considered. Tissue smear revealed Donovan bodies. Biopsy showed areas of necrosis and ulceration in epidermis and papillary dermis along with presence of mixed inflammatory infiltrate in perivascular areas. Based on presence of Donovan bodies, final diagnosis of verrucous variant of granuloma inguinale was made. The patient was started on oral doxycycline 100 mg twice daily and tablet cotrimoxazole DS (160 mg+800 mg) twice daily. There was reduction in size of lesion after 12 weeks and further the patient was lost to follow-up.
Verrucous lesion with dry, irregular surface in right inguinal area (Case 5).

Case 6
A 50-year-old male truck driver presented with painless ulcers with seropurulent discharge over perianal area since two months. He gave history of unprotected sexual exposures with CSWs and was on ART since three years. Examination revealed single, well defined irregularly shaped ulcer of size 6×12 cm with purulent discharge and beefy red granulation tissue [Table/Fig-11]. The ulcer was non-tender and was bleeding easily on touch. Inguinal lymph nodes were non-palpable. Differential diagnosis of donovanosis and perianal Crohn’s disease were considered. VDRL was non-reactive. Tissue smear showed donovan bodies and diagnosis of donovanosis was established. Patient was treated with oral doxycycline 100 mg twice daily for ten weeks.
Well defined ulcer with purulent discharge in perianal area (Case 6).

The case details of the patients have been shown in [Table/Fig-12].
Case details of the patients.
| Case details | Case 1 | Case 2 | Case 3 | Case 4 | Case 5 | Case 6 |
|---|
| Age (years) | 55 | 34 | 35 | 22 | 45 | 50 |
| Sex | M | F | M | M | M | M |
| Marital Status | Married | Married | Married | Single | Married | Married |
| History of ART | + | + | + | - | + | + |
| Duration of complaints (in months) | 6 | 2 | 3 | 0.5 | 6 | 2 |
| Sites | Penis | Perianal | Penis and Inguinal | Perineal | Inguinal | Perianal |
| Morphological Type | Ulcerogranulomatous | Ulcerogranulomatous | Ulcerogranulomatous | Ulcerogranulomatous | Hypertrophic | Ulcerogranulomatous |
| Tissue Smear | + | + | + | + | + | + |
Discussion
McLeod (1882) was the first to describe the disease as serpiginous ulceration of the groin. Donovanosis is described under numerous terminologies such as Granuloma inguinale, Granuloma venereum, Granuloma inguinale tropicum and ulcerating granuloma of the pudenda. The term Donovanosis was suggested to honour Donovan (1905) who first described the causative organism and the characteristic inclusion bodies [4].
Four types of presentation are described in Donovanosis, namely-ulcerogranulomatous type, hypertrophic or verrucous type, sclerotic or cicatricial type and necrotic or phagedenic type [5]. The ulcerogranulomatous type is most common and presents with slow progressing, painless, well defined ulcers with exuberant beefy red granulation tissue and bleeds easily on touch. The hypertrophic variant presents with dry verrucous growth over genito-inguinal region. The sclerotic type is associated with scarring of genitalia. The necrotic (phagedenic) variant is associated with rapidly progressive ulcers with destruction of surrounding tissues. In our study, case 5 was hypertrophic type whereas other five cases were ulcerogranulomatous type.
The incubation period is uncertain, ranging between 3-40 days. Experimental lesions were induced in humans 50 days after inoculation. The genital region is affected in 90% of cases and inguinal area in 10%. In men, the coronal sulcus, subpreputial region, and anus and in women, the labia minora, fourchette and perianal areas are most commonly involved [5].
Confirmatory diagnosis is based on tissue smear in which a small piece of tissue from the margin of ulcer is removed using forceps or edge of razor blade and crushed between two slides (Rajam and Rangiah method). The specimen is stained with Giemsa or Leishman stain [6]. Biopsy is more time consuming and associated with discomfort to patient and thus advised only in tissue smear negative cases and cases which are unresponsive to treatment or if malignancy is suspected [7].
The Centers for Disease Control and Prevention (CDC) recommends tablet azithromycin one gram weekly or 500 mg daily for at least three weeks or until all lesions have healed. Other alternatives include oral doxycycline 100 mg twice daily or cotrimoxazole DS twice daily for a period of three or more weeks. Erythromycin 500 mg four times a day is drug of choice during pregnancy or lactation. In case of no response within few weeks, gentamycin 1 mg/kg 8 hourly should be used. Partners within 60 days prior to onset of lesions should be examined and offered treatment [8].
Four patients in our study (case 2, 4, 5 and 6) responded well to treatment with oral doxycycline, whereas, case 1 and 3 required addition of injectable gentamycin and streptomycin respectively. In a study conducted to observe the mean healing time of donovanosis ulcers, reported that time required in HIV-positive patients was approximately 26 days as compared to 17 days in HIV-negative cases [9]. In our study, the healing time in the HIV negative case was 4 weeks whereas it ranged from 8-18 weeks in HIV positive subjects. Hence, we can conclude that HIV patients require longer duration of therapy, often requiring a combination of drugs primarily injectable aminoglycoside.
Various studies conducted on pattern of Sexually Transmitted Infections (STIs) in different parts of India reveal reduction in prevalence of donovanosis [10-14]. Cases of donovanosis have not been reported from Central India. In a study of pattern of STIs from Jabalpur, no cases of donovanosis were found [12]. However, six cases of donovanosis presented to our tertiary care centre in two year period (January 2016-December 2017). The probable causes include high risk sexual behaviour among all cases, exposure from CSW, visits to endemic region as seen in cases 3 and 6 who were truck drivers with frequent visits to Orissa and Andhra Pradesh.
Donovanosis is usually considered as STI spread by autoinoculation and faecal contamination has also been described [5]. Though donovanosis has low infectivity, the presence of large ulcers and chances of bleeding on touch possess a greater risk of transmission of HIV [5]. Prompt diagnosis and treatment, prolonged use of antibiotics, partner evaluation and promotion of safe intercourse techniques are important steps in controlling both donovanosis and HIV.
Conclusion
Although the prevalence of donovanosis has decreased and it is considered to be an endemic disease, we should evaluate the patients with granulomatous ulcers over genitals even in non-endemic areas. Most of the cases found have associated HIV infection and require prolonged treatment duration with combination of antibiotics.
[1]. Pilani A, Vora R, Anjaneyan G, Granuloma inguinale mimicking as squamous cell carcinoma of penisIndian J Sex Transm Dis 2014 35(1):56-58.10.4103/0253-7184.13243324958990 [Google Scholar] [CrossRef] [PubMed]
[2]. O’Farrell N, Moi H, European guideline on donovanosisInt J STD AIDS 2016 27(8):605-07.10.1177/095646241663362626882914 [Google Scholar] [CrossRef] [PubMed]
[3]. Ganesh R, Donovanosis. In: Sharma VK, editorSexually Transmitted Diseases and HIV/AIDS 2009 2nd edNew DelhiViva Books Private Limited:347-55. [Google Scholar]
[4]. O’Farrell N, Donovanosis. In: Holmes KK, Sparling PF, Stamm WE, et. al. (eds)Sexually Transmitted Diseases 2008 4th edThe McGraw-Hill Companies, Inc:701-08. [Google Scholar]
[5]. O’Farrell N, DonovanosisSex Transm Infect 2002 78:452-57.10.1177/095646241663362626882914 [Google Scholar] [CrossRef] [PubMed]
[6]. Kaimal S, Thappa DM, Methods of specimen collection for the diagnosis of STIsIndian J Dermatol Venereol Leprol 2007 73(2):129-32.10.4103/0378-6323.3190717456928 [Google Scholar] [CrossRef] [PubMed]
[7]. Richens J, Donovanosis (granuloma inguinale)Sexually Transmitted Infections 2006 82:21-22.10.1136/sti.2006.02313517151047 [Google Scholar] [CrossRef] [PubMed]
[8]. Workowski KA, Bolan GA, Centers for Disease Control and Prevention. Sexually transmitted diseases treatment guidelines, 2015MMWR Recomm Rep 2015 64(RR-03):1-137. [Google Scholar]
[9]. Jamkhedkar PP, Hira SK, Shroff HJ, Lanjewar DN, Clinico-epidemiologic features of granuloma inguinale in the era of acquired immune deficiency syndromeSex Transm Dis 1998 25:196-200.10.1097/00007435-199804000-000049564722 [Google Scholar] [CrossRef] [PubMed]
[10]. Chandragupta TS, Badri SR, Murty SV, Swarnakumari G, Prakash B, Changing trends of sexually transmitted diseases at KakinadaIndian J Sex Trans Dis 2007 28:6-9.10.4103/0253-7184.35703 [Google Scholar] [CrossRef]
[11]. Jain VK, Dayal S, Aggarwal K, Jain S, Changing trends of sexually transmitted diseases at RohtakIndian J Sex Transm Dis 2008 29:23-25.10.4103/0253-7184.42710 [Google Scholar] [CrossRef]
[12]. Chatterjee M, Ramadasan P, Profile of sexually transmitted diseases in and around JabalpurIndian J Sex Trans Dis 2004 25:13-17. [Google Scholar]
[13]. Narayanan B, A retrospective study of the pattern of sexually transmitted diseases during a ten-year periodIndian J Dermatol Venereol Leprol 2005 71:333-37.10.4103/0378-6323.1678416394458 [Google Scholar] [CrossRef] [PubMed]
[14]. Nair SP, A study of the changing trends in the pattern of sexually transmitted infections in the state of KerelaIndian J Sex Transm Dis 2012 33:64-65.10.4103/0253-7184.9383522529462 [Google Scholar] [CrossRef] [PubMed]