Association of Arterial Stiffness and Lipid Profile in Coronary Artery Disease
Damacharla Balakrishna1, B Sowjanya2, P Ramamohan3, John Preetham Kumar Gurja4, ML Sreenivasa Kumar5, Pushpaja Mitta6
1 Ph.D Scholar, Department of Biochemistry, Narayana Medical College, Nellore, Andhra Pradesh, India.
2 Professor, Department of Biochemistry, Narayana Medical College, Nellore, Andhra Pradesh, India.
3 Professor, Department of Pharmacology, Narayana Medical College, Nellore, Andhra Pradesh, India.
4 Tutor, Department of Physiology, Narayana Medical College, Nellore, Andhra Pradesh, India.
5 Assistant Professor, Department of Cardiology, Narayana Medical College, Nellore, Andhra Pradesh, India.
6 MBBS Student, Narayana Medical College, Nellore, Andhra Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Damacharla Balakrishna, Ph.D Scholar, Department of Biochemistry, Narayana Medical College, Nellore-524003, Andhra Pradesh, India.
E-mail: dganithanvi@gmail.com
Introduction
Coronary Artery Disease (CAD) is one of the leading causes of death in India. The prevalence of the CAD related mortality in non-diabetic patients is 11%. Increased arterial stiffness may be independently contributing to increased mortality and morbidity in CAD. However, arterial stiffness and hyperlipidaemia are known to coexist in CAD.
Aim
To measure lipid profile and arterial stiffness and to explore the possible association between the two.
Materials and Methods
It was a cross-sectional study, 150 angiographically proven CAD patients and 150 apparently healthy subjects with no history of CAD were recruited. The study was initiated after written consent informed was obtained. Augmentation Index (AIx) and Sub Endocardial Viability Ratio (SEVR) were measured out in all the participants using Pulse wave analysis (SphygmoCor device). Lipid profile parameters (Total cholesterol, triglycerides, high density lipoproteins, low density lipoproteins, very low density lipoproteins, and total cholesterol/high density lipoproteins ratio) were measured using Humastar automated analyser. All the measured parameters were analysed by student t-test using SPSS version 22.0.
Results
The present study found that significant increase in AIx in CAD patients (29.66±12.85) than controls (23.28±7.96%) (p<0.0001) and decrease in SEVR (p<0.0001) in CAD cases (139.56±31.77) when compared to controls (161.99±37.33). There was no significant difference in lipid profile between the two groups.
Conclusion
The results suggest that arterial stiffness has independently increased in patients with CAD. However, we did not find significant association between lipid profile and arterial stiffening.
Atherosclerosis, Augmentation index, Pulse wave analysis, Sub endocardial viability ratio
Introduction
Coronary artery disease has been a leading cause of morbidity and mortality across the globe. In India, CAD has become epidemic, showing steady rise in mortality rate with increasing prevalence of 6% from 1% in rural and to 10% from 1% in urban areas over the past 6 decades [1,2]. One of the predictive risk factor for coronary artery disease is increased arterial stiffness, which occurs due to decrease in the elasticity of the arterial wall. Biological ageing and arteriosclerosis leads to formation of arterial stiffness [3]. Mechanical fraying of lamellar elastin structures which occurs due to repeated cycles of mechanical stress, loss of arterial elastin and fibrosis as a compensatory mechanism results in changes in the morphology and increase in content of arterial collagen proteins which contributes to increased arterial stiffening [4]. There is increased load on the heart due to increase in arterial stiffness which results in left ventricular hypertrophy and remodeling leading to heart failure [5,6]. Hyperlipidaemia is believed to be a risk factor for CAD, while High Density Lipoprotein (HDL) is cardio protective [7]. Lowering the cholesterol retards progression of atherosclerosis and even regression of some plaques is observed, reducing the risk of CAD [8]. Plasma lipids, inflammation, endothelial damage and atherosclerosis are potential mechanism leading to arterial stiffness [9]. However, there is inconsistent relationship between serum lipid profiles and arterial stiffness. Significant association between dyslipidaemia and AIx were not found. According to a study it was found that lower LDL was linked with higher mortality risk, which is opposite to what was expected [10-12]. So, early detection and prevention of CAD is very important, which may help in better prognosis through lifestyle modification that may further decrease mortality and morbidity rates. It’s imperative to study the association of CAD to lipid levels and arterial stiffness in light of the contrary findings of lipid profile and its association to arterial stiffness in CAD.
Materials and Methods
This cross-sectional study includes 150 angiographically proven CAD patients recruited from the Department of Cardiology, Narayana Medical College, Nellore, Andhra Pradesh. 150 apparently healthy controls with no history of CAD, from general population of Nellore. The study was conducted from July 2017 to May 2018 and participants were selected using random sampling.
Sample size was calculated assuming equal standard deviation of 15% between two groups in augmentation index with a mean difference of 5%, keeping the power to 80% and alpha error to 5% and p-value two sided. The calculated sample size to detect such difference was 141. Sample size was rounded to 150 to overcome data loss.
Subjects with age less than 20 and more than 60 years, having a history of type 2 Diabetes Mellitus (DM) or taking medications for diabetes were excluded. Additionally, patients receiving statins were also excluded.
The Institutional Ethical Committee gave clearance to execute the study protocol (NMCH/IEC/22/2017); participants were recruited after informed written consent was obtained.
Demographic parameters such as age, sex, height, weight, and Body Mass Index (BMI) were recorded of each participant. The fasting blood samples were collected from both cases and controls. The serum was separated from blood by centrifugation at 3000 rpm for 5 minutes. Lipid profile parameters {Total Cholesterol (TC), Triglycerides (TGL), Low Density Lipoproteins (LDL), High Density Lipoproteins (HDL) and Very Low Density Lipoproteins (VLDL)} were estimated by enzymatic method using Master fully automated analyser.
Estimation of Lipid Profile Parameters
Cholesterol was estimated by cholesterol oxidase and peroxidase method, enzymatic colorimetric test for cholesterol with Lipid Clearing Factor (LCF). The cholesterol is determined after enzymatic hydrolysis and oxidation. The indicator quinone imine is formed from hydrogen peroxide and 4-amino phenazone in the presence of phenol and peroxidase. Reference values 150 to 200 mg/dL [13].
HDL was measured by direct homogenous enzymatic colorimetric test. The assay combines two specific steps: 1) Elimination of chylomicrons, VLDL, and LDL by cholesterol esterase and cholesterol oxidase; 2) Estimation of HDL by cholesterol oxidase and peroxidase method. Reference values 40 to 60 mg/dL [13].
TGL was estimated by enzymatic end point method glycerol-3-phosphate oxidase and P-aminophenazone (GPO-PAP). Reference values 80 to 160 mg/dL [13].
LDL and VLDL were calculated by a standard friedewald equation. LDL-C values were calculated according to the following formulas: VLDL-C=triglyceride/5 and LDL-C=cholesterol–(VLDL-C+HDL-C). Reference values for LDL are 80 to 160 mg/dL and VLDL is 25 to 40 mg/dL [13].
In these subjects, after an initial rest period of 10 minutes, average blood pressures of three readings were taken. Pulse wave velocity, AIx and SEVR was measured by using sphygmocor device (At Cor Medical Pvt., Ltd., Australia). The set up consists of a hand held tonometer attached to a device and a laptop. High fidelity sequential pressure wave forms were obtained by placing the tonometer on the radial artery of the dominant wrist. The device then applies transfer function to these peripheral measurements and central (aortic) pressure parameters and degree of augmentation secondary to reflected wave from periphery were estimated.
Augmentation index is calculated as the difference between two systolic peaks of a pulse wave P2 and P1 (ΔP) and expressed as a percentage of the Pulse Pressure (PP) [14] and SEVR is the ratio of the diastolic Area Under the Curve (AUC) of an arterial pulse wave to the systolic AUC [15,16]. Reference values for AIx are 7 to 30% and for SEVR are 121 to 172 as per the sphygmocor protocol.
Statistical Analysis
Continuous data was described as mean and standard deviation. Category data as numbers and percentages. Unpaired t-test was used to inference the differences among the profiles of vascular stiffness and lipid levels between the two groups. Statistical analysis was performed by using IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp. Further the association between AIx and other parameters was analysed with Pearson’s correlation test. A p-value<0.05 was considered to be significant.
Results
A total of 300 subjects participated in the study, there were 188/300 (62.66%) males and 112/300 (37.33%) females. In the CAD group the number of males and females were 111 and 39 respectively. In control group the number of males and females were 77 and 73 respectively. The mean age of the participants was 42.68±8.15 (22 to 60 years). However, there were more males in both the groups (p<0.05). The mean age of patients (46.97±7.61 years) was more than that of controls (38.39±10.24 years) (p<0.0001).
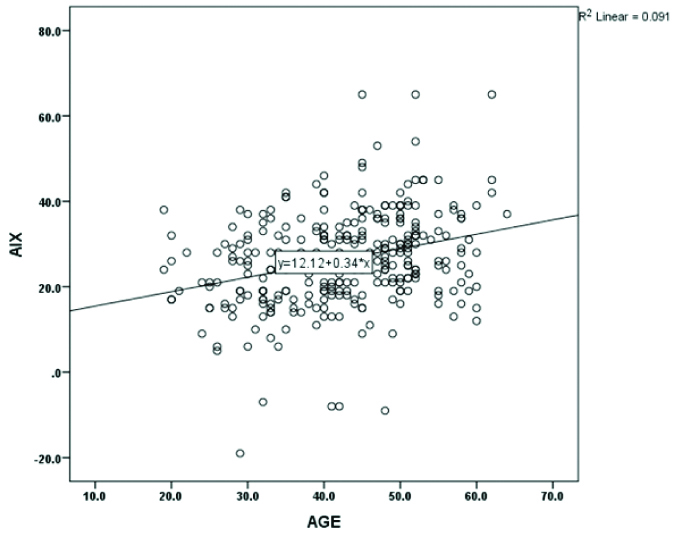
It can be seen from [Table/Fig-1] that this study finds a significant difference between the cases and controls in BMI (23.52±3.4 vs. 24.93±3.47 Kg/m2) SBP (128.07±15.30 vs. 119.47±10.09 mmHg) and DBP (80.03±8.36 vs. 76.27±6.98 mmHg) respectively. In contrast to the expectations there was no significant difference in lipid levels i.e. total cholesterol (170.83±33.48 vs. 168.87±31.55 mg/dL), TGL (142.75±0.65 vs. 134.65±43.48 mg/dL), LDL (100.13±21.68 vs. 99.67±20.65 mg/dL), HDL (42.08±8.16 vs. 42.59±7.60 mg/dL) and VLDL (28.83±8.62 vs. 26.99±8.59 mg/dL). However, the ratio of total cholesterol and HDL was significantly higher in CAD compared to control group (p-value <0.01). In addition, pulse wave measures such as AIx is significantly increased (29.66±12.85 vs. 23.28±7.96) (p<0.0001) and SEVR was decreased (139.56±31.77 vs. 161.99±37.33) (p<0.0001) in CAD when compared to controls respectively [Table/Fig-1]. Pearson’s correlations have revealed that there was no significant relationship between anthropometric, biochemical and pulse wave measures except between age and AIx which showed a significant positive relationship (p=<0.0001, r=0.301**) [Table/Fig-2].
Group statistics of anthropometric, biochemical and pulse wave analysis measures.
| Parameter | Cases (Mean±SD) | Controls (Mean±SD) | p-value |
|---|
| Age (years) | 46.97±7.61 | 38.39±10.24 | <0.0001** |
| SBP (mmHg) | 128.07±15.30 | 119.47±10.09 | <0.0001** |
| DBP (mmHg) | 80.03±8.36 | 76.27±6.98 | <0.0001** |
| Height (r) | 164.98±6.83 | 163.71±9.10 | 0.17 |
| Weight (Kgs) | 64.41±10.88 | 66.61±10.15 | 0.07 |
| BMI (kg/m2) | 23.52±3.40 | 24.93±3.47 | <0.0001** |
| AIx (%) | 29.66±12.85 | 23.28±7.96 | <0.0001** |
| SEVR | 139.56±31.17 | 161.99±37.33 | <0.0001** |
| Total cholesterol (mg/dL) | 170.83±33.48 | 168.87±31.55 | 0.60 |
| Triglycerides (mg/dL) | 142.75±0.65 | 134.65±43.48 | 0.11 |
| LDL (mg/dL) | 100.13±21.68 | 99.67±20.65 | 0.85 |
| HDL (mg/dL) | 42.08±8.16 | 42.59±7.60 | 0.57 |
| VLDL (mg/dL) | 28.83±8.62 | 26.99±8.59 | 0.06 |
| CHOL/HDL | 4.04±0.36 | 3.92±0.26 | <0.01* |
Significant-*, Highly significant-**
Correlation between AIx and Age.
Discussion
This research aimed at studying the arterial stiffness and lipid profile in CAD patients as there was inconsistency that is suggestive of causal role of the above in CAD. This study finds increased arterial stiffness in cases compared to controls. This is in line with increased arterial stiffness in CAD reported by Yingchoncharoen T et al., [17]. Stiffening of vessels may lead to earlier pulse wave reflection and increase left ventricular load, decreases diastolic perfusion compromising myocardial oxygen supply. Increased arterial stiffness may induce remodeling of the vessels and atherosclerosis further [18,19].
The present study shows a positive correlation of augmentation index with age. Janner JH et al., reported that the prevalence of CAD increased with age, as age is one of the unmodifiable risk factor [15]. These findings are in line with Weber T et al., findings showing strong relationship between CAD and Aix [20]. Arterial stiffness has been shown to be associated with the risk factors such as age, hypertension and diabetes mellitus [21,22]. On the other hand, the association between serum lipids and arterial stiffness was found to be inconsistent. Moreover, the superiority of lipid profiles in the early diagnosis has been questioned and unconfirmed [9,23,24].
This study did not find significant lipidemic difference between CAD and controls. It has been found that Indians are developing CAD at much lower cholesterol levels [25], suggesting that lipid profile does not necessarily have association with CAD as a risk factor. However, the accuracy of arterial stiffness as a predictor in establishing CAD diagnosis independent of lipid changes needs to be further validated with larger sample size.
Limitation
The study included only 150 patients from a single hospital, a larger study involving more patient groups from different hospitals could have been done to generalise present study results. Despite of weakness the results of current study indicates arterial stiffness is an independent predictor of CVD risk, which is non invasive and larger population studies can be taken up for cardiovascular risk assessment.
Conclusion
This study concludes that pulse wave analysis as AIx and SEVR may be better indicator for early prediction of CAD than lipid profile, as lipid profileis influenced by many factors. This possibly explains encountering CAD in subjects with normal or even low lipid profile parameters and AIx and SEVR merit as better predictors of the likely CAD.
Significant-*, Highly significant-**
[1]. Mishra S, Ray S, Dalal JJ, Sawhney JPS, Ramakrishnan S, Nair T, Management standards for stable coronary artery disease in IndiaIndian Heart J 2016 68:S31-49.10.1016/j.ihj.2016.11.32028038722 [Google Scholar] [CrossRef] [PubMed]
[2]. Gupta R, Mohan I, Narula J, Trends in coronary heart disease epidemiology in indiaAnn Glob Heal 2016 82(2):307-15.10.1016/j.aogh.2016.04.00227372534 [Google Scholar] [CrossRef] [PubMed]
[3]. Husmann M, Jacomella V, Thalhammer C, Amann-vesti BR, Markers of arterial stiffness in peripheral arterial diseaseVasa 2015 44(5):341-48.10.1024/0301-1526/a00045226317253 [Google Scholar] [CrossRef] [PubMed]
[4]. Zieman SJ, Melenovsky V, Kass DA, Mechanisms, pathophysiology, and therapy ofarterial stiffnessArterioscler Thromb Vasc Biol 2005 25(5):932-43.10.1161/01.ATV.0000160548.78317.2915731494 [Google Scholar] [CrossRef] [PubMed]
[5]. Cameron JD, Dart AM, Exercise training increases total systemic arterial compliance in humansAm J Physiol 1994 266(2 Pt 2):H693-701.10.1152/ajpheart.1994.266.2.H6938141370 [Google Scholar] [CrossRef] [PubMed]
[6]. Kohara K, Tabara Y, Oshiumi A, Miyawaki Y, Kobayashi T, Miki T, Radial Augmentation Index: A Useful and Easily Obtainable Parameter for Vascular AgingAm J Hypertens 2005 18(1 Pt 2):11S-14S.10.1016/j.amjhyper.2004.10.01015683726 [Google Scholar] [CrossRef] [PubMed]
[7]. Steinberg D, Atherogenesis in perspective: Hypercholesterolemia and inflammation as partners in crimeNat Med 2002 8(11):1211-17.10.1038/nm1102-121112411947 [Google Scholar] [CrossRef] [PubMed]
[8]. Libby P, Inflammation in atherosclerosisNature 2002 420(6917):868-74.10.1038/nature0132312490960 [Google Scholar] [CrossRef] [PubMed]
[9]. Wang F, Ye P, Luo L, Xiao W, Qi L, Bian S, Association of serum lipids with arterial stiffness in a population-based study in BeijingEur J Clin Invest 2011 41(9):929-36.10.1111/j.1365-2362.2011.02481.x21314825 [Google Scholar] [CrossRef] [PubMed]
[10]. Miller M, Cannon CP, Murphy SA, Qin J, Ray KK, Braunwald E, PROVE IT-TIMI 22 Investigators. Impact of Triglyceride Levels Beyond Low-Density Lipoprotein Cholesterol After Acute Coronary Syndrome in the PROVE IT-TIMI 22 TrialJ Am Coll Cardiol 2008 51(7):724-30.10.1016/j.jacc.2007.10.03818279736 [Google Scholar] [CrossRef] [PubMed]
[11]. Barter P, Gotto AM, LaRosa JC, Maroni J, Szarek M, Grundy SM, HDL cholesterol, very low levels of LDL cholesterol, and cardiovascular eventsN Engl J Med 2007 357(13):1301-10.10.1056/NEJMoa06427817898099 [Google Scholar] [CrossRef] [PubMed]
[12]. Olsson AG, Schwartz GG, Szarek M, Sasiela WJ, Ezekowitz MD, Ganz P, High-density lipoprotein, but not low-density lipoprotein cholesterol levels influence short-term prognosis after acute coronary syndrome: results from the MIRACL trialEur Heart J 2005 26(9):890-96.10.1093/eurheartj/ehi18615764620 [Google Scholar] [CrossRef] [PubMed]
[13]. Akhyani M, Ehsani AH, Robati AM, The lipid profile in psoriasis: a controlled studyJ Eur Acad 2007 21(10):1330-32.10.1111/j.1468-3083.2007.02260.x17958837 [Google Scholar] [CrossRef] [PubMed]
[14]. Nürnberger J, Keflioglu-Scheiber A, Opazo Saez AM, Wenzel RR, Philipp T, Schafers RF, Augmentation index is associated with cardiovascular riskJ Hypertens 2002 20(12):2407-14.10.1097/00004872-200212000-0002012473865 [Google Scholar] [CrossRef] [PubMed]
[15]. Janner JH, Godtfredsen NS, Ladelund S, Vestbo J, Prescott E, Aortic augmentation index: Reference values in a large unselected population by means of the sphygmocor deviceAm J Hypertens 2010 23(2):180-85.10.1038/ajh.2009.23419959999 [Google Scholar] [CrossRef] [PubMed]
[16]. Aslanger E, Assous B, Bihry N, Beauvais F, Logeart D, Cohen-Solal A, Baseline subendocardial viability ratio influences left ventricular systolic improvement with cardiac rehabilitationAnatol J Cardiol 2017 17(1):37-43.10.14744/AnatolJCardiol.2016.70095324860 [Google Scholar] [CrossRef] [PubMed]
[17]. Yingchoncharoen T, Limpijankit T, Jongjirasiri S, Laothamatas J, Yamwong S, Sritara P, Arterial stiffness contributes to coronary artery disease risk prediction beyond the traditional risk score (RAMA-EGAT score)Heart Asia 2012 4(1):77-82.10.1136/heartasia-2011-01007923585778 [Google Scholar] [CrossRef] [PubMed]
[18]. Subrahmanyam G, Pathapati RM, Ramalingam K, Indira SA, Kantha K, Soren B, Arterial stiffness and trace elements in apparently healthy population-a cross-sectional studyJ Clin Diagn Res 2016 10(9):LC12-LC15.10.7860/JCDR/2016/21648.854827790472 [Google Scholar] [CrossRef] [PubMed]
[19]. Quick S, Waessnig N, Sommer P, Heidrich FM, Pfluecke C, Ibrahim K, Impact of papillary muscles on ventricular function measurements in 3 T cardiac magnetic resonanceCor et Vasa 2017 59(2):e142-48.10.1016/j.crvasa.2016.06.002 [Google Scholar] [CrossRef]
[20]. Weber T, Auer J, O’Rourke MF, Kvas E, Lassnig E, Berent R, Arterial stiffness, wave reflections, and the risk of coronary artery diseaseCirculation 2004 109(2):184-89.10.1161/01.CIR.0000105767.94169.E314662706 [Google Scholar] [CrossRef] [PubMed]
[21]. Tuttolomondo A, Di Raimondo D, Di Sciacca R, Pecoraro R, Arnao V, Butta C, Arterial stiffness and ischemic stroke in subjects with and without metabolic syndromeAtherosclerosis 2012 225(1):216-19.10.1016/j.atherosclerosis.2012.08.02723031362 [Google Scholar] [CrossRef] [PubMed]
[22]. Yilmaz FK, Guler GB, Kaya O, Guler E, Demir GG, Gunes HM, Relationship between arterial stiffness parameters and the extent and severity of coronary artery diseaseCor et Vasa 2017 59(2):e134-41.10.1016/j.crvasa.2016.05.004 [Google Scholar] [CrossRef]
[23]. Di Bonito P, Moio N, Scilla C, Cavuto L, Sibilio G, Sanguigno E, Usefulness of the High Triglyceride-to-HDL cholesterol ratio to identify cardiometabolic risk factors and preclinical signs of organ damage in outpatient childrenDiabetes Care 2012 35(1):158-62.10.2337/dc11-145622040842 [Google Scholar] [CrossRef] [PubMed]
[24]. Holewijn S, Heijer M Den, Swinkels DW, Stalenhoef AF, Graaf J De, Apolipoprotein B, non-HDL cholesterol and LDL cholesterol for identifying individuals at increased cardiovascular riskJ Intern Med 2010 268(6):567-77.10.1111/j.1365-2796.2010.02277.x21091808 [Google Scholar] [CrossRef] [PubMed]
[25]. Lenkey Z, Illyés M, Böcskei R, Husznai R, Sárszegi Z, Meiszterics Z, Comparison of arterial stiffness parameters in patients with coronary artery disease and diabetes mellitus using arteriographPhysiol Res 2014 63(4):429-37. [Google Scholar]