Pyrexia of Unknown Origin: A Perplexing Case
Kiren George Koshy1, Moothezhathu Kesavadas Suresh2, Jithin John3, Karthik Vijayakumar4, Krishnakumar Madhavan5
1 Junior Resident, Department of Internal Medicine, Government Medical College, Thiruvananthapuram, Trivandrum, Kerala, India.
2 Professor, Department of Internal Medicine, Government Medical College, Thiruvananthapuram, Trivandrum, Kerala, India.
3 Junior Resident, Department of Internal Medicine, Government Medical College, Thiruvananthapuram, Trivandrum, Kerala, India.
4 Junior Resident, Department of Internal Medicine, Government Medical College, Thiruvananthapuram, Trivandrum, Kerala, India.
5 Junior Resident, Department of Internal Medicine, Government Medical College, Thiruvananthapuram, Trivandrum, Kerala, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Kiren George Koshy, TC 4/2559(1); Pattom Kawdiar Road; Kawdiar PO; Trivandrum, Kerala, India.
E-mail: kirenkoshy@gmail.com
Pyrexia of Unknown Origin (PUO) is a common diagnostic dilemma in the medical wards. We present the case of a 64-year-old man who had presented with fever, fatigue, dry cough and bloody diarrhea. Over the next few days, he developed severe testicular pain and renal failure. Blood results revealed anaemia, raised ESR, negative ANA and negative ANCA. Renal biopsy showed crescentic glomerulonephritis. Repeat value of c-ANCA was positive which clinched the diagnosis of Granulomatosis with Polyangiitis (GPA). We present this case in order to illustrate the masquerading nature of the vasculitic syndromes and to emphasise the need to integrate clinical and laboratory clues to reach a diagnosis.
Crescentic glomerulonephritis, Polyangiitis, Vasculitis
Case Report
A 64-year-old man was admitted in hospital with chief complaints of fever, anorexia and fatigue for one month. He had a dry cough with breathlessness which had worsened over two weeks and severe pain in the right calf muscle.
Clinical examination revealed fever, tachypnea and crepitation in all lung fields. Neurological examination was unremarkable except for an absent right ankle jerk. There were no oral ulcers, arthritis or photosensitivity.
Blood investigations showed anaemia with elevated ESR. There were widespread patchy opacities in the chest X-ray [Table/Fig-1]. He was put on broad spectrum antibiotics with a provisional diagnosis of bronchopneumonia.
Initial chest X-ray showing widespread patchy opacities.

On day 2 of admission, he developed bloody diarrhea with cramps. As the stool examination revealed trophozoites of amoeba, metronidazole was added to his antibiotic regimen. On Day 3, he developed excruciating pain in his right testicle. Renal function worsened dramatically over the next two days and the serum creatinine rose to 3.5 mg/dL on the fourth day. A routine urine examination showed albuminuria with RBC casts. Blood, urine and stool cultures were sterile.
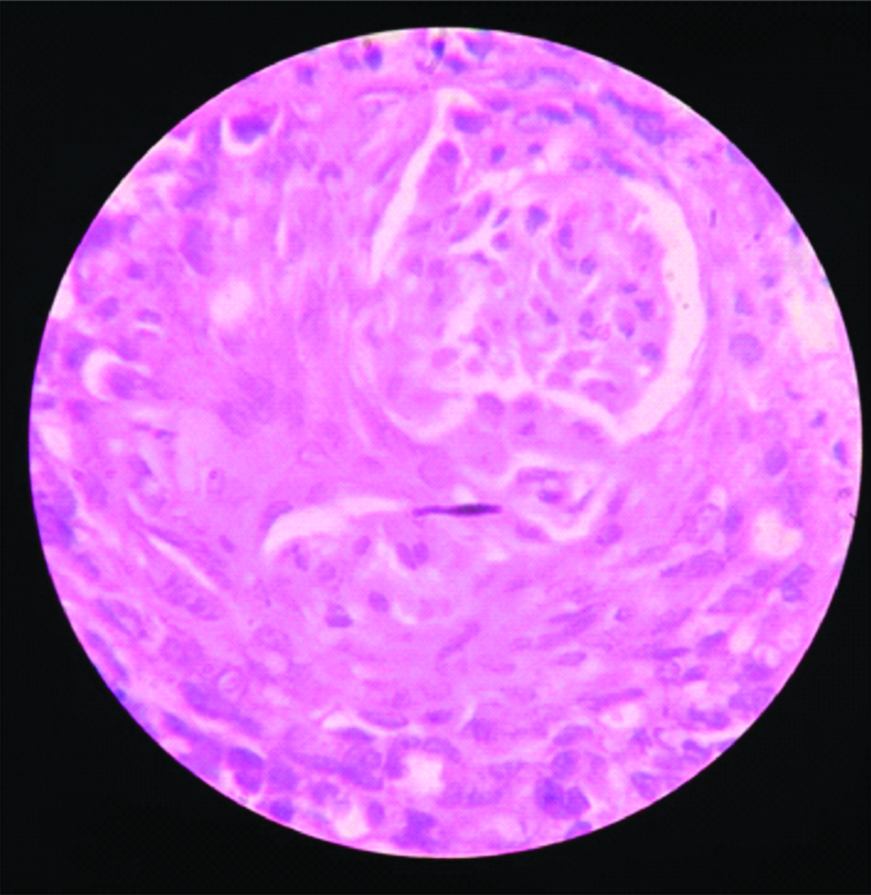
Based on the rapidly progressive renal failure and multisystem involvement, the diagnosis was revised as vasculitis. Sputum Acid Fast Bacillus (AFB), Cartridge Based Nucleic Acid Amplification Test (CBNAAT) and tests for leptospirosis, scrub typhus and hantavirus were negative. ANA, c-ANCA and p-ANCA were also negative. Nerve Conduction study revealed an axonal neuropathy involving the right tibial and common peroneal nerves. The renal biopsy showed crescentic glomerulonephritis [Table/Fig-2].
Renal biopsy showing crescentic glomerulonephritis. (100X magnification, Haematoxylin and Eosin staining)
A clinical diagnosis of ANCA-associated vasculitis was made and the patient was given pulsed steroids (intravenous methylprednisolone) with cyclophosphamide. There was remarkable recovery of the clinical and renal parameters. A repeat Chest X-ray showed clearance of chest infiltrates [Table/Fig-3]. On repeating after two weeks, c-ANCA was strongly positive. The patient remains on pulsed cyclophosphamide and tapering doses of steroid.
Repeat chest X-ray showing clearance of opacities.

Discussion
GPA (Granulomatosis with Polyangiitis) is an ANCA associated vasculitis predominantly involving the upper respiratory tract, the lungs and the glomeruli. Over 90% of cases have upper airway involvement [1]. GPA may present in many ways including PUO, Rapidly Progressive Glomerulonephritis (RPGN) and mononeuritis multiplex. Diagnosis is often delayed [2]. While c-ANCA is positive in about 90% of cases of GPA, it is not an essential criterion for diagnosis [3]. Dermatological involvement is also common in GPA with palpable purpura in 50% of cases. The main cause of mortality in this condition is infection and active vasculitis [4].
Vasculitis is difficult to diagnose and can masquerade as a variety of other diseases. Precise diagnosis of a named vasculitis is even more difficult. In the present case study, the presence of severe testicular pain is more characteristic of Polyarteritis Nodosa (PAN), but lung parenchymal and glomerular involvement is in favour of GPA [5].
ANCA can be false negative early in the course of GPA and should be repeated if clinically indicated [6].
In severe GPA, especially in the presence of RPGN, treatment may have to be started before a definitive diagnosis is obtained. Pulsed steroids and cyclophosphamide may be organ-saving, and indeed, life-saving in such cases. The EULAR (European League Against Rheumatism) recommendations state that cyclophosphamide with steroids are the first line therapy in generalised GPA [7]. In refractory cases, rituximab may be used. Alternatively, rituximab can be used as a first-line of agent especially in younger patients [8].
Conclusion
We present a case of prolonged fever, pneumonitis and renal failure which was diagnosed as ANCA positive vasculitis probably Granulomatosis with Polyangiitis. The early clues to the diagnosis of vasculitis included testicular pain, rapidly progressive renal failure and painful neuropathy. A renal biopsy clinched the diagnosis. We wish to stress the importance of avoiding over-reliance on antibodies in diagnosing vasculitis, and the need for prompt immunosuppression without waiting for histological evidence.
[1]. Hoffman GS, Kerr GS, Leavitt RY, Hallahan CW, Lebovics RS, Travis WD, Wegener’s granulomatosis: An analysis of 158 patientsAnn Intern Med 1992 116:488-98.10.7326/0003-4819-116-6-4881739240 [Google Scholar] [CrossRef] [PubMed]
[2]. Abdou NI, Kullman GJ, Hoffman GS, Sharp GC, Specks U, McDonald T, Wegener’s granulomatosis: Survey of 701 patients in North America. Changes in outcome in the 1990sJ Rheumatol 2002 29:309-16. [Google Scholar]
[3]. Latalo PM, Cruz DP, Diagnosis and classification of granulomatosis with polyangiitisJ Autoimmun 2014 48:94-98.10.1016/j.jaut.2014.01.02824485158 [Google Scholar] [CrossRef] [PubMed]
[4]. Luqmani R, Suppiah R, Edwards CJ, Philip R, Maskell J, Culliford D, Mortality in Wegener’s granulomatosis: A bimodal patternRheumatology 2011 50:697-702.10.1093/rheumatology/keq35121112869 [Google Scholar] [CrossRef] [PubMed]
[5]. Hernandez-Rodriguez J, Alba MA, Prieto-Gonzalez S, Cid MC, Diagnosis and classification of polyarteritis nodosaJ Autoimmun 2014 48:84-89.10.1016/j.jaut.2014.01.02924485157 [Google Scholar] [CrossRef] [PubMed]
[6]. Wang R, Yang XC, Zhou SJ, Sun GY, Anti-neutrophil cytoplasmic antibody-negative microscopic polyangiitis: A case report and literature reviewExp Ther Med 2015 10(2):749-52.10.3892/etm.2015.252326622387 [Google Scholar] [CrossRef] [PubMed]
[7]. Mukhtyar C, Guillevin L, Cid MC, Dasgupta B, de Groot K, Gross W, EULAR recommendations for the management of primary small and medium vessel vasculitisAnn Rheum Dis 2009 68:310-17.10.1136/ard.2008.08809618413444 [Google Scholar] [CrossRef] [PubMed]
[8]. Jones RB, Tervaert JW, Hauser T, Luqmani R, Morgan MD, Peh CA, Rituximab versus cyclophosphamide in ANCA-associated renal vasculitisN Engl J Med 2010 363:211-20.10.1056/NEJMoa090916920647198 [Google Scholar] [CrossRef] [PubMed]