Fever is a common presentation for paediatric patients, often posing a difficulty for health professionals who must determine whether there is an underlying serious illness. The prevalence of paediatric presentations of fever is known to vary between community and hospital-based encounters. In the community, fever is one of the most common reasons for children to attend General Practice, along with cough, earache, sore throat and generalised weakness/tiredness [1,2]. Variable prevalence for the presentation of fever to Emergency Departments (ED) is reported; notably in Sydney at the New Children’s Hospital, 20-30% of all children’s visits to the ED were for fever [3].
The management of fever requires the health professional to balance the physiological benefits of fever, detrimental impacts of an uncontrolled febrile response, and adverse effects associated with investigations and consequent management [4,5]. Clinical guidelines exist to stratify children by their risk of serious illnesses in specific cases, for example, febrile infants less than three months [6-9]. Such guidelines recognise that this age group may not display characteristic signs of serious infection or typical localising features and are more likely to deteriorate rapidly than older children [8,9]. These children require a full septic workup (full blood count, blood culture, urine culture and lumbar puncture, chest X-ray if clinically indicated) as well as hospital admission for empiric intravenous antibiotics and fluids [6,7]. Clinical Guidelines, however, are less prescriptive in effectively guiding clinical decision making in older age groups. Furthermore, adherence to guidelines is likely influenced significantly by factors such as clinician experience. Community paediatricians in the USA, for example, were shown to have followed guidelines for only 42% of paediatric fever presentations [10]. A Canadian study found that even between centres using similar guidelines there were huge variations in the number of urine tests and lumbar punctures ordered as well as antibiotics administered [11].
The present study aimed to compare paediatric presentations of fever in community locations to hospital locations in regards to patient flow, which relates specifically to investigations ordered, follow-up arrangements made and advice given.
Materials and Methods
The present study was a retrospective cross-sectional study which analysed the data from the Australian National University (ANU) Clinical Audit Project (CAP) database.
Operational Definitions
For the purpose of this study, hospital locations refer to presentations to an emergency department, hospital inpatients, hospital wards, operating theatres or ambulance service. Community locations refer to medical centres, community health services, community paediatrics, general practice, hospital outpatients and private rooms. The symptom of fever was inclusive of presentations documented as International Classification of Primary Care version 2 Plus (ICPC 2+) diagnostic coding code A03 and A78 which include “fever”, “fever; unknown origin”, “feeling; feverish”, “fever; relapsing” and “fever; viral” [12]. Patient flow refers to the handling of a patient during their encounter with a medical facility, inclusive of (1) investigations ordered, (2) follow-up arranged and (3) advice offered. Investigations encompassed haematology, biochemistry, imaging or bacteriology.
Participants
This study analysed patient data from the Australian National University (ANU) Clinical Audit Project (CAP) dataset, collected by year 3 medical students from 2007-2012 and 2014. This dataset documents demographic and clinical parameters for 9,154 patient encounters at The Canberra Hospital or numerous community health locations in the Australian Capital Territory and surrounding areas of New South Wales. Patients were surveyed from a period inclusive of 2007-2012 and additionally 2014 by way of a written questionnaire completed by third-year ANU medical students [Appendix-1]. From this dataset 319 were included in the final analysis of this study with inclusion criteria of age ≤16 years and fever (ICPC 2+ code A03 and A78).
The study has the approval of the respective ANU, New South Wales Health and ACT Health Ethics committees with signed consent forms requested from all participants. Equivalent approval has been provided by Central Australian Aboriginal Congress (CAAC) in the Northern Territory.
Survey Parameters
Relevant to this study, the CAP electronic database included the following parameters; age, encounter site, reasons for encounter, investigations ordered, consequence of encounter and advice have given [Appendix-1]. Survey data were entered into the database using standardised fields with reasons for encounter and diagnoses coded using the International Classification of Primary Care version 2 plus (ICPC 2+) diagnostic coding [12].
Statistical Analysis
All analyses were performed using SPSS for Windows (version 22.0; SPSS: An IBM Company, Chicago, Illinois USA, 2013). Data were presented as number and percentage (%). The clinical and demographic characteristics were compared between community and hospital locations by chi-square test with continuity correction where appropriate. Statistical significance was defined as p-value <0.05.
Results
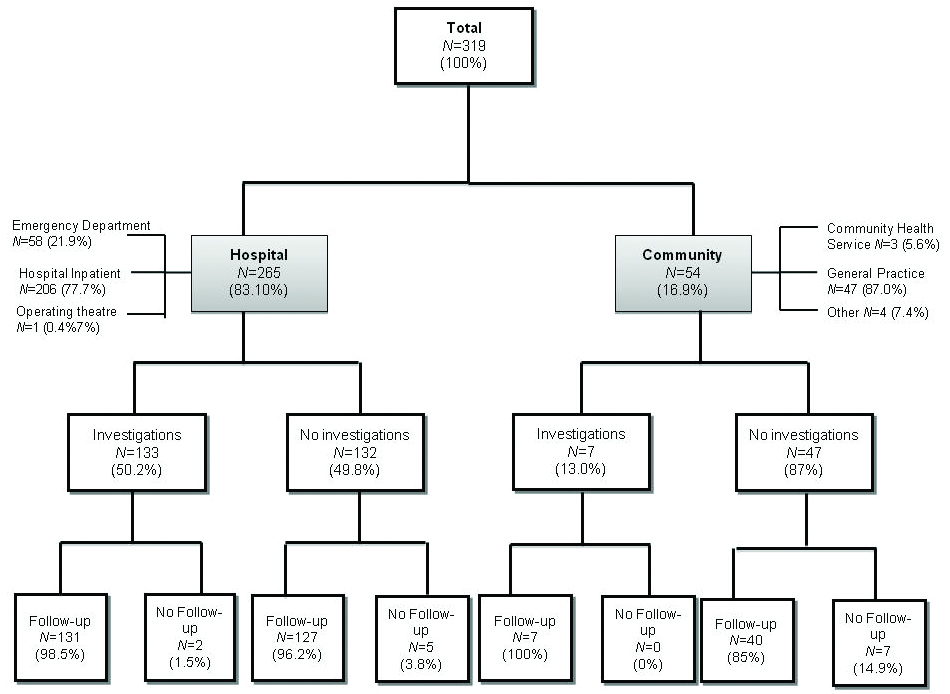
This study used a population of 319 patients [Table/Fig-1]. Of these, 265 (83.1%) were surveyed in hospital locations and 54 (16.9%) were surveyed in community locations. Within hospital locations133 (50.2%) of the patients surveyed had at least one investigation, while in community locations only seven patients (13.0%) had at least one investigation. Almost all patients were followed-up [Table/Fig-1]. Among the patients who received no investigations in the community setting (n=47, 87%), only seven patients (14.9%) had no follow-up compared to 5 (3.8%) among hospital setting. In the hospital location, the majority of patients received follow-up advice regardless of whether investigations were performed or not (98.5% and 96.2% respectively) [Table/Fig-1].
Study Design showing the total number patients analysed and resulting percentage of patients through various patient-flow pathways.
Investigations
The present data shows that haematology was the most common investigation performed both in hospital (50.2%) and community (13%) locations (p<0.001). It was followed by biochemistry in both hospital (40.8%) and community (7.4%) groups (p<0.001). Beyond this the order of most frequently used investigations between groups differs, with the next most common investigation being X-ray (32.8%) in hospital locations and ultrasound (3.7%) in community settings [Table/Fig-2].
Frequencies of investigations, types of advice, and follow-up in the hospital and community. (Only relevant data presented here).
| Hospital (n=265) | Community (n=54) | p-value |
|---|
| Investigations |
| Haematology | 133 (50.2) | 7 (13.0) | <0.001 |
| Biochemistry | 108 (40.8) | 4 (7.4) | <0.001 |
| Cervical Cytology | 0 (0.0) | 1 (1.9) | 0.027 |
| Other Cytology | 8 (3.0) | 0 (0.0) | 0.196 |
| Bacteriology | 66 (24.9) | 1 (1.9) | <0.001 |
| X-Ray | 87 (32.8) | 1(1.9) | <0.001 |
| Ultrasound | 21 (7.9) | 2 (3.7) | 0.274 |
| ECG | 31 (11.7) | 0 (0.0) | 0.008 |
| CT-Scan | 25 (9.4) | 2 (3.7) | 0.168 |
| MRI-Scan | 6 (2.3) | 0 (0.0) | 0.264 |
| Advice |
| Further investigations awaited | 70 (26.4) | 2 (3.7) | <0.001 |
| Referral to specialist | 20 (7.5) | 1 (1.9) | <0.001 |
| Specific health promotion advice | 20 (7.5) | 4 (7.4) | 0.387 |
| Specific treatment advice | 155 (58.5) | 47 (87.0) | <0.001 |
| Follow-up |
| Admitted | 58 (21.9) | 1 (1.9) | <0.001 |
| Asked to make follow-up appointment | 7 (2.6) | 7 (13.0) | <0.001 |
| Continuing inpatient care | 119 (44.9) | 0 (0.0) | <0.001 |
| Discharge to GP | 39 (14.7) | 0 (0.0) | <0.001 |
| Follow-up not required | 7 (2.6) | 7 (13.0) | <0.001 |
| Referred to other health professional | 2 (0.8) | 0 (0.0) | <0.001 |
| Referred to specialist medical/OPD | 4 (1.5) | 2 (3.7) | <0.001 |
| Return as needed | 5 (1.9) | 36 (66.7) | <0.001 |
| Theatre | 10 (3.8) | 1 (1.9) | <0.001 |
| Other | 14 (5.3) | 0 (0.0) | <0.001 |
Data are presented as n (%). CT: Scan denotes Computerised tomography scan; ECG: Electrocardiogram; GP: General practitioner; MRI: Magnetic resonance imaging; and OPD: Outpatient department
Advice
The type of advice given was found to differ in several ways between the hospital and community groups. Within hospital locations, it was significantly more likely than in community locations for doctors to advise patients to await further investigations (26.4% vs. 3.7%, respectively; p<0.001) and to refer patients to a specialist (7.5% vs. 1.9%, respectively; p<0.001). On the other hand, ‘specific treatment advice’ was less likely to be provided in hospital than in community locations (58.5% vs. 87%, respectively; p<0.001). There was no difference between the two groups in provision of ‘specific health promotion advice’ (7.4% vs. 7.5% respectively; p=0.387) [Table/Fig-2].
Follow-up
Within hospital locations, the most common type of follow-up was continuing inpatient care (44.9%), followed by admission (21.9%), and discharge with General Practitioner (GP) follow-up (14.7%). In community locations, the most common type of follow-up was ‘return as needed’ (66.7%), followed by ‘asked to make follow-up appointment’ (13%), and ‘no follow-up required’ (13%). Presentation of paediatric fever within the community was significantly more likely to conclude with ‘return as needed’ than in hospital locations, (p<0.001). Patients presenting in the community were also significantly more likely to be designated as ‘follow-up not required’, or ‘asked to make follow-up appointment’ than in the hospital (p<0.001). On the other hand, all other follow-up options were significantly more likely to be designated in the hospital than in the community [Table/Fig-2].
Discussion
The present study of paediatric patient flow in the ACT and surrounding NSW has shown that children who presented with fever to a hospital location were four times more likely to have investigations than those who presented to a community location. Haematology and biochemistry were the most common investigations ordered in both groups. Although quantification of cost is beyond the scope of this study, the greater number of investigations ordered for hospital patients suggests that care of febrile paediatric patients within the hospital is more expensive than within the community.
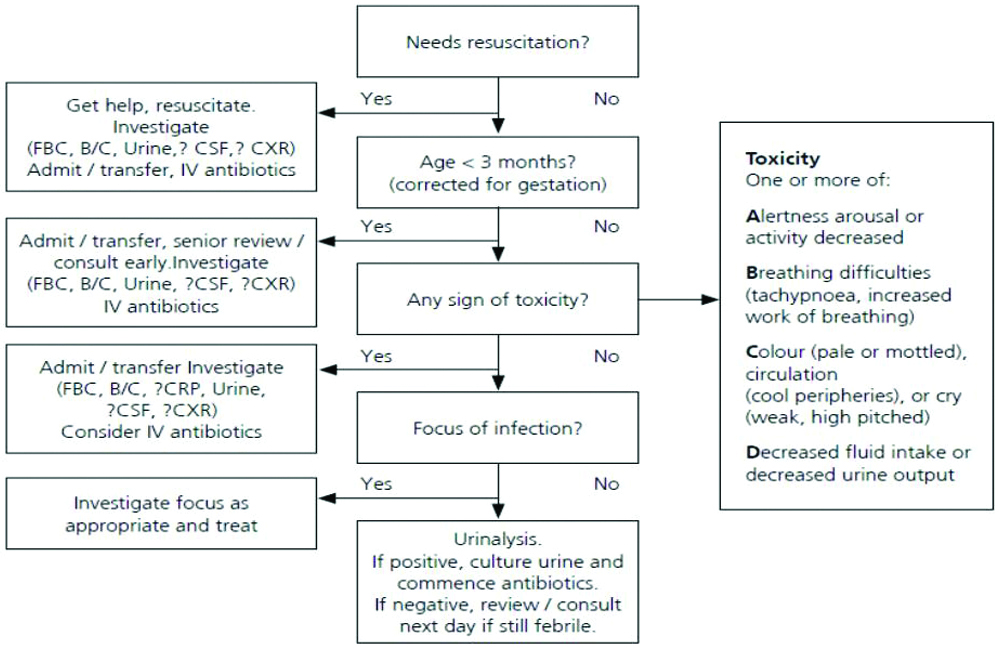
The advice was given to patients in each group also differed, reflecting the greater number of investigations performed in hospital locations. Patients most commonly received ‘specific treatment advice’ in both hospital (58.5%) and community (87.0%) locations. However, hospital patients were seven times more likely to be advised to await further investigations than those in the community. As expected, follow-up in the two settings also differed. The majority (66.7%) of patients seen in the community were told to ‘return as needed’ and a further 13% were asked to make a follow-up appointment. In the hospital, 44.9% of patients were monitored with continuing in-patient care, and 21.9% were admitted following the presentation. It is unclear from this study to definitively say whether the NSW Health Acute Management of Fever Guidelines were followed [Table/Fig-3] [8]. However, for those children that did have investigations, haematology and biochemistry were the first-line investigations ordered as per the recommendations.
Infants and Children: Acute Management of Fever. NSW Health Clinical Practice Guidelines; 2nd Edition (2010).
The present study does demonstrate that patient follow-up could be improved. Recommendations are for follow-up within 24 hours post-ED discharge to assess the progression of the infection, response to treatment and results of investigations, with these, follow-up instructions to be relayed to parents in writing. The present study showed that of the patients discharged from hospital, 14.7% were discharged into the care of a GP, a further 2.6% were specifically asked to make a follow-up appointment and 1.9% was told to return as needed. Provision of appropriate advice in community locations was superior to hospital with 13.0% asked to make a follow-up appointment, and 66.7% told to return as needed. The levels of specific treatment advice in both the hospital and community locations more closely followed the recommendations, with 58.5% and 87.0% respectively.
The design of this research study showed trends around patient flow, with regards to fever presentations in hospital versus community settings.
Limitation
Firstly, the absence of 2013 data results in a non-continuous data set from 2007 to 2014. Secondly, patients included in this study were those that presented with fever, either alone or with additional symptoms. Stratifying the data to look at fever alone, or fever with other presenting complaints may perhaps reveal different patient flow patterns. Since this study encompassed all patients up to and including the age of 16, stratifying the data into narrower age brackets to account for a confounder effect may also reveal different patient flow patterns. All children below 3 months of age with a fever, for example, are routinely examined with a full septic screen [8,9], whereas presentations of fever in older children do not fall under this strict guideline. Furthermore, the precise temperature in degrees Celsius at which a child was considered to have a fever, and whether the severity of fever behaved as an effect modifier in influencing investigations ordered, were not considered in this study. An assumption has been made, furthermore, that both community and hospital healthcare workers have identical access to the various investigations discussed in this study. If this is not, in fact, the case, this may again affect the patient flow patterns suggested in this study. In addition, it was not known whether patient presentations in hospital had, in fact, come from a community consultation initially. Finally, it is important to acknowledge that there was a lack of systemic collection of data as data collectors were neither officially trained nor monitored regarding data collection. It is unknown whether this would have led to systematic error in the data, but it is a possibility.
It is unclear from this study to definitively say whether the NSW Health Acute Management of Fever Guidelines were followed [8]. However, for those children that did have investigations, haematology and biochemistry were the first-line investigations ordered as per the recommendations. Selection bias should also be assumed, as the data collection was only carried out at select and limited sites where third-year ANU medical students were routinely assigned on placement. This restricted patient selection to predominantly smaller private practices in urban communities of ACT and southeast NSW. Thus, it could be anticipated that the findings are not representative of patients who access public health services (e.g. walk-in clinics) or bulk-billing centres. The study is also limited by the lack of data on patient comorbidities, which may have strongly influenced patients flow.
Future directions stemming from this study, therefore, are to clarify some of the limitations discussed above. In addition to these study design aspects, it would be interesting to investigate whether the results of this study are unique to ACT and surrounding NSW or similarly unique to the time frame analysed. Importantly, asking further questions around why patient flow patterns are evidently different between community and hospital locations, and how this affects patient outcome as well as the cost of resources, would be of great interest to pursue further.
Conclusion
This study provides a unique look into how the flow of paediatric patients is managed across different healthcare settings in the ACT and surrounding NSW. It suggests that paediatric patient flow following presentations of fever differ significantly between the community and hospital location. This suggests the existence of important disparities between the resources consumed in the care of febrile paediatric patients in the hospital versus community. These data also reveal that clinical guidelines are not strictly adhered to, particularly with regards to patient follow-up. This suggests the need for further research into the impact of differences in patient flow.