Post Partum Seizures Associated with Reversible Posterior Leukoencephalopathy Syndrome (RPLS): A Case Report
Manali S Dhage1, S Sarumathy2, Fatema J Haji3, SP Ahalya4, K Muthuraj5
1 Student, Department of Pharmacy Practice, SRM College of Pharmacy, SRMIST, Chennai, Tamil Nadu, India.
2 Assistant Professor, Department of Pharmacy Practice, SRM College of Pharmacy, SRMIST, Chennai, Tamil Nadu, India.
3 Student, Department of Pharmacy Practice, SRM College of Pharmacy, SRMIST, Chennai, Tamil Nadu, India.
4 Assistant Professor, Department of Pharmacy Practice, SRM College of Pharmacy, SRMIST, Chennai, Tamil Nadu, India.
5 Professor, Department of Neurology, SRM Medical College Hospital and Research Centre (SRM MCHRC), Chennai, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. S Sarumathy, Assistant Professor, Department of Pharmacy Practice SRM College of Pharmacy SRMIST, Kancheepuram (District), Tamil Nadu-603203, India.
E-mail: saruprabakar@gmail.com
Reversible Posterior Leukoencephalopathy Syndrome (RPLS) is a condition characterised by severe headache, confusion, seizures and visual loss. It can occur secondary to electrolyte disturbances, eclampsia and preeclampsia, ultimately leading to vasogenic oedema in the cerebral parieto-occipital region. It is a rare condition and the prevalence is unknown. Inconsequential literature studies have been found related to RPLS associated with delayed onset of post partum eclampsia. Here we present a case of young female patient aged 25-year-old with complaints of post partum seizures preceded by severe headache and blurring of vision. She was treated with anti-hypertensive and anti-seizure medications. Imaging studies are vital for the prompt and accurate diagnosis of RPLS. Precise and immediate management has led to reversal of this syndrome in the patients.
Blood pressure, Grand tonic clonic seizures, Post partum eclampsia
Case Report
A young female patient aged 25-year-old, gravida three, para one was admitted with complains of post partum seizures since past four days (D6 post delivery) and was referred to our hospital for further management. The patient had an uneventful pregnancy and gave birth to a healthy baby boy. She had six episodes of seizures prior to admission. The onset of seizures preceded with severe headache and blurring of vision followed by Grand Tonic Clonic Seizures (GTCS) associated with up-rolling of eyes, loss of consciousness, involuntary micturition. The duration of seizures was approximately two minutes. The patient had no history of hypertension or mental illness and her blood pressure was normal during her pregnancy period. She was a known case of hypothyroidism since three months of gestation, on regular medication (T.Levothyroxine sodium 125 mg). According to her obstetrical history, patient had two abortions, 3 years back and the other 6 months prior to her current pregnancy.
On admission patient had elevated blood pressure of 150/90 mmHg with heart rate of 100 beats/min and respiratory rate of 20 beats/min. Pupils were equal with no contractions or dilatations and reactive to light. There was elevation in laboratory parameters such as ALP (138 U/L), LDH levels (369 U/L) CSF protein (63 mg/dL), and decrease in potassium levels (3.3 mmol/L), and neutrophils (83%). Trace amount of albumin was found in the urine. Complete Blood Count (CBC), serum electrolytes, blood glucose levels, Thyroid Stimulating Hormone (TSH), Prothrombin Time (PT) was found to be normal. USG renal doppler and renal function test were performed to preclude renal complications, which were found to be normal. Echocardiogram (ECG) report indicated unusual ‘U’ waves. Electroencephalogram (EEG) which was taken immediately after seizure revealed GTCS. Blood immunology was done to obviate Antiphospholipid antibody syndrome (APS). Magnetic resonance venography examination showed no abnormalities. Patient’s provisional diagnosis suggested delayed post partum eclampsia. Magnetic Resonance Imaging Fluid-Attenuated Inversion Recovery (MRI-FLAIR) showed a significant possibility of atypical RPLS. Consultation was sought from ophthalmology, nephrology, respiratory medicine, rheumatology, cardiology and obstetrics and gynaecology.
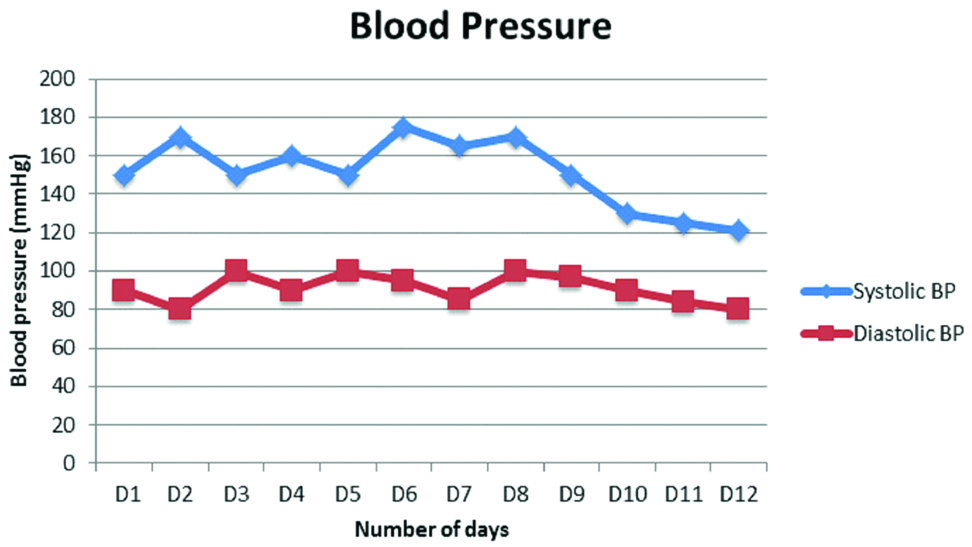
Patient was treated with intravenous (i.v) Fosphenytoin 150 mg and i.v Levetiracetam 500 mg twice daily. Despite therapy, recurrent two episodes of seizures occurred on day 3 and 4. The first convulsion occurred at 00:30 am with up-rolling of eyes, increase in blood pressure (170/80 mmHg) and heart rate (112 beats/min), with peripheral capillary oxygen saturation (SPO2) 100%, and it ceased within two minutes. The second episode occurred at 5:00 am which lasted for one minute with increase of blood pressure (160/100 mmHg) and heart rate (82 beats/min), preceded by severe headache and dizziness. Intravenous magnesium sulphate eight ml STAT was given in loading dose over five minutes followed by a maintenance dose of 2 mL/hr 25 mL amp infusion over 24 hours with monitoring of respiratory rate and patellar reflex. Patient was also given tablet labetolol (100 mg) and tablet nifedipine (10 mg) for aggressive blood pressure management. However, patient complained of severe headache and persistent elevation in BP was observed on examination. Hence, tablet nifedipine (10 mg) was withdrawn and tablet amlodipine (5 mg) was added. Syp. potassium chloride (5 mL) was given to normalise potassium levels. Blood pressure was significantly normalised after the administration of tablet amlodipine. Patient no longer complained of headaches and no episodes of recurrent seizures occurred untill day 9. The patient was kept under observation for 3 more days. Significant elevation in blood pressure is observed followed by normalisation post treatment, indicating possible reversal of oedema [Table/Fig-1]. and was discharged on 12th day after admission without any symptoms along with tablet amlodipine (5 mg), tablet labetolol (100 mg) and tablet levetiracetam (500 mg). Patient was advised for a review after 2 months.
Blood pressure chart of the patient.
Discussion
RPLS is also known as Posterior Reversible Encephalopathy Syndrome (PRES). The pathophysiology of RPLS is disputable and is largely based on the theory of disturbance in autoregulation of cerebral blood pressure which causes acute clinical symptoms such as headache, seizures, visual disturbances and neurological signs [1]. This widely proposed theory states that elevated blood pressure causes malfunctioning of autoregulation of cerebral blood flow which leads to breakdown of blood brain barrier, followed by vasogenic oedema. Another theory suggests a possibility in the role of endothelial dysfunction in the development of RPLS [2]. A study conducted by Pizon AF and Mattar F et al., concluded that women with post partum preeclampsia had a decreased blood pressure, minimal proteinuria and higher incidence of neurological deficits when compared to women with post partum eclampsia [3,4]. Eclamptic women often complain of a thunderclap headache, which can be defined as a severe headache which reaches its peak within a few seconds to minutes to reach its maximum intensity [5]. These symptoms are usually reversible upon prompt treatment and permanent neurological damage or death occurs in rare cases [6,7].
RPLS predominantly affects the parieto-occipital areas of the brain [1]. Pre-eclampsia and eclampsia are usually associated with RPLS during pregnancy. HELLP syndrome (Haemolysis, Elevated liver enzymes, Low platelet count) is a complication of pre-eclampsia and occurs in about one-third cases of eclampsia [8]. Post partum haemorrhage could be a possible trigger for RPLS associated with delayed post partum eclampsia. Triggering factors also include increased blood pressure, hormone fluctuations, massive blood transfusion [9]. A study suggested that delayed post partum eclampsia occurred in about 14% of the total cases of eclampsia [7].
Since the exact prevalence of RPLS in eclamptic patients is not exactly known, an issue with these rough values indicates that there is no consensus as to the right time for ordering neuroimaging studies [10]. A study conducted by Mayama M et al., concluded that 19% of women with preeclampsia and 92.3% of women with eclampsia complicated with neurological symptoms developed RPLS [11]. Hence, imaging studies are vital for the accurate diagnosis of RPLS. Although Computed Tomography (CT) scans may be performed as initial investigations, MRI is considered as gold standard for the diagnosis of RPLS. It can be used to rule out differential diagnosis and can provide data about cerebral involvement. [8]. Neurological findings mainly involve symmetrical vasogenic oedema in the posterior white matter of the brain. Findings of neuroimaging studies are not limited to occipital and parietal lobes of the brain as any part of the brain can be damaged, although majority of cases report abnormalities in these two regions [2]. Diffusion weighted MRI has a better intensity compared to CT as it can differentiate between cytotoxic and vasogenic oedema in eclamptic patients [12,13]. Although difficult, it is important to rule out differential diagnosis for prompt management of RPLS. Differential diagnosis mainly involves ischemic stroke, cerebral venous sinus thrombosis, mitochondrial disease and central nervous system infections (encephalitis, meningitis).
Present recommendations suggest supportive therapy along with treatment of underlying causes which generally leads to reversal of the neurological symptoms [14]. Although, no studies have been done to measure effect of controlling hypertension and specific anti-hypertensive drugs have not been clinically studied, there is a general belief among physicians that the control of blood pressure is important and the selection of these agents is left to the clinician [15]. The pharmacological therapy of this patient is similar to the therapeutic plan as reported in a case study by Rijal JP et al., wherein the patient was treated with Magnesium sulphate and Labetalol [7]. Literature review of several publications revealed similar line of pharmacological management. Magnesium sulphate is usually considered as first line therapy. When given intravenously, regardless of serum magnesium levels, it stabilises blood pressure by decreasing calcium dependent vasoconstriction. It also decreases vasogenic oedema and decreases Blood Brain Barrier (BBB) permeability [14]. Patients are monitored for tendon reflexes and urine output. Patients are concomitantly treated with anti-epileptic agents such as Phenytoin, Valproic acid and Diazepam as well as anti-hypertensive agents. Target blood pressure levels should reach systolic pressure of 140-155 mmHg and diastolic pressure of 90-105 mmHg. Anti-hypertensive agents preferred are calcium channel blockers, i.v hydralazine and orally administered labetolol and nifedipine [8]. Patients can also be treated with corticosteroids such as dexamethasone or betamethasone [6].
Conclusion
There is a good prognosis when RPLS is diagnosed accurately and neurological signs are reversed following prompt treatment within a few weeks.
[1]. Hobson EV, Craven I, Blank C, Posterior reversible encephalopathy syndrome: a truly treatable neurologic illnessPerit Dial Int 2012 32(6):590-94.https://doi.org/10.3747/pdi.2012.0015210.3747/pdi.2012.0015223212858 [Google Scholar] [CrossRef] [PubMed]
[2]. Verma AK, Garg RK, Pradeep Y, Malhotra HS, Rizvi I, Kumar N, Posterior encephalopathy syndrome in women with eclampsia: predictors and outcomePregnancy Hypertens 2017 10:74-82.10.1016/j.preghy.2017.06.00429153695 [Google Scholar] [CrossRef] [PubMed]
[3]. Pizon AF, Wolfson AB, Postpartum focal neurologic deficits: posterior leukoencephalopathy syndromeJ Emerg Med 2005 29(2):163-66.10.1016/j.jemermed.2005.02.00616029827 [Google Scholar] [CrossRef] [PubMed]
[4]. Mattar F, Sibai BM, Eclampsia: VIII. Risk factors for maternal morbidityAm J Obstet Gynecol 2000 182(2):307-12.10.1016/S0002-9378(00)70216-X [Google Scholar] [CrossRef]
[5]. Garg RK, Kumar N, Malhotra HS, Posterior reversible encephalopathy syndrome in eclampsiaNeurol India 2018 66(5):1316-23.10.4103/0028-3886.24136430232997 [Google Scholar] [CrossRef] [PubMed]
[6]. Demirel İ, Kavak BS, Özer AB, Bayar MK, Erhan ÖL, An intensive care approach to posterior reversible encephalopathy syndrome (PRES): An analysis of 7 casesJ Turk Ger Gynecol Assoc 2014 15(4):217-21.https://doi.org/10.5152/jtgga.2014.1407210.5152/jtgga.2014.1407225584029 [Google Scholar] [CrossRef] [PubMed]
[7]. Rijal JP, Giri S, Dawadi S, Dahal KV, Posterior reversible encephalopathy syndrome (PRES) in a patient with late postpartum eclampsiaBMJ Case Rep 2014 2014:bcr2013203162https://doi.org/10.1136/bcr-2013-20316210.1136/bcr-2013-20316224577180 [Google Scholar] [CrossRef] [PubMed]
[8]. Cozzolino M, Bianchi C, Mariani G, Marchi L, Fambrini M, Mecacci F, Therapy and differential diagnosis of Posterior Reversible Encephalopathy Syndrome (PRES) during pregnancy and postpartumArch Gynecol Obstet 2015 292(6):1217-23.10.1007/s00404-015-3800-426122264 [Google Scholar] [CrossRef] [PubMed]
[9]. Lio CF, Lee YH, Chan HY, Yu CC, Peng NJ, Chan HP, Posterior reversible encephalopathy syndrome in a postpartum hemorrhagic woman without hypertension: A case reportMedicine (Baltimore) 2017 96(16):e669010.1097/MD.000000000000669028422884 [Google Scholar] [CrossRef] [PubMed]
[10]. Camara-Lemarroy CR, Escobedo-Zúñiga N, Villarreal-Garza E, García-Valadez E, Góngora-Rivera F, Villarreal-Velázquez HJ, Posterior reversible leukoencephalopathy syndrome (PRES) associated with severe eclampsia: clinical and biochemical featuresPregnancy Hypertens 2017 :44-49.10.1016/j.preghy.2017.01.00328279447 [Google Scholar] [CrossRef] [PubMed]
[11]. Mayama M, Uno K, Tano S, Yoshihara M, Ukai M, Kishigami Y, Incidence of posterior reversible encephalopathy syndrome in eclamptic and women with preeclampsia with neurologic symptomsAm J Obstet Gynecol 2016 215(2):239.e1-5.10.1016/j.ajog.2016.02.03926902987 [Google Scholar] [CrossRef] [PubMed]
[12]. O’Kane M, Elhalwagy H, Kumar S, Badawi C, Unusual presentation of PRES in the postnatal periodBMJ Case Rep 2014 2014:pii: bcr201320340610.1136/bcr-2013-20340625008333 [Google Scholar] [CrossRef] [PubMed]
[13]. Watanabe Y, Mitomo M, Tokuda Y, Yoshida K, Choi S, Hosoki T, Eclamptic encephalopathy: MRI, including diffusion-weighted imagesNeuroradiology 2002 44(12):981-85.10.1007/s00234-002-0867-y12483442 [Google Scholar] [CrossRef] [PubMed]
[14]. Pandita A, Lehmann DF, Neurological function in Posterior Reversible Encephalopathy Syndrome (PRES) report of a caseNeurologist 2018 23(2):65-66.10.1097/NRL.000000000000017429494439 [Google Scholar] [CrossRef] [PubMed]
[15]. Fugate JE, Rabinstein AA, Posterior reversible encephalopathy syndrome: Clinical and radiological manifestations, pathophysiology, and outstanding questionsLancet Neurol 2015 14(9):914-25.10.1016/S1474-4422(15)00111-8 [Google Scholar] [CrossRef]