Cervical cancer is the second most common cancer among women all over the world [1,2]. In India, it is the most common gynaecological cancer and one of the leading causes of cancer-related deaths in women. In Kolar, Karnataka, the prevalence of carcinoma cervix amounts to 17.55% of all cancer cases in the female population. Squamous cell carcinoma constitutes 80% of cases and adenocarcinoma is relatively rare [3]. The diagnosis of pre-malignant and malignant lesions of the cervix is predominantly dependent on the presence of atypia. These atypical cells are primarily identified and classified based on their characteristic nuclear features [2]. There is a high degree of interobserver variability in the subcategorisation of LSIL and HSIL as well as LCGIN and AIS. These discrepancies are due to the dependency on visual interpretation for the diagnosis of these lesions. Moreover, very few studies have attempted morphometric analysis of both the ectocervical and endocervical; pre-malignant and malignant lesions [4-6]. This study attempts to reduce the variability in the use of subjective visual evaluation of histopathological specimens, which is the gold standard for diagnosis, by employing morphometrical analysis and thus providing an objective, quantitative and reproducible interpretation of endocervical and ectocervical pre-malignant and malignant lesions.
Materials and Methods
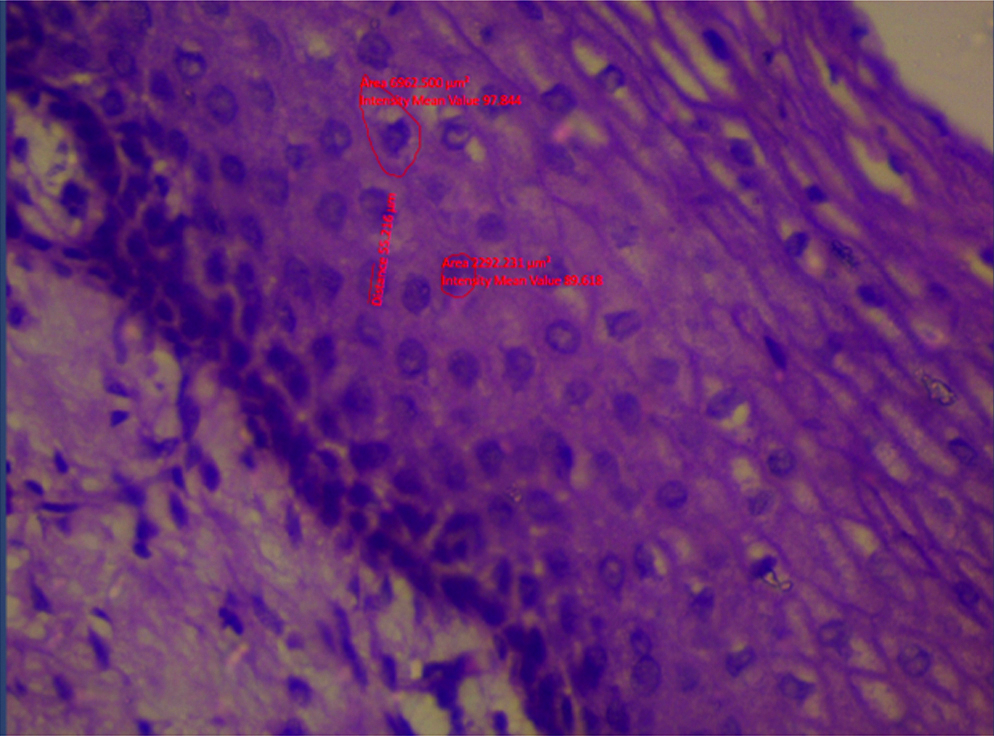
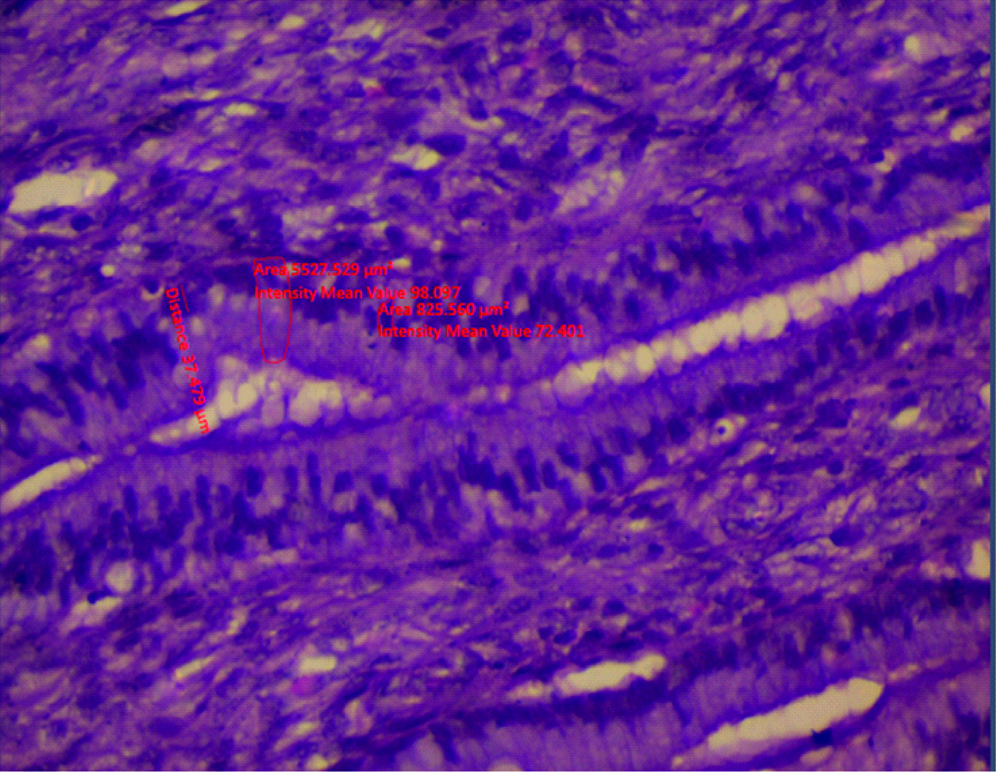
This study is a retrospective cross-section study which was done on 120 cases of cervical specimens which were either in the form of cervical biopsy or hysterectomy specimens. This study was approved by the Institutional Ethics Committee (DMC/KLR/IEC/155/2016-2017). The records and histopathological slides of these cases were retrieved from the archives of the Department of Pathology, Sri Devaraj URS Medical College between October 2016 to September 2017. Cases that had undergone chemotherapy or radiotherapy were excluded from the study. The 120 cases were then categorised histomorphologically into normal ectocervix, chronic cervicitis, LSIL, HSIL, SCC, normal endocervix, chronic endocervicitis, LCGIN, AIS and adenocarcinoma. The diagnosis of LCGIN is more challenging as many features overlap with those of reactive changes. The glands in LCGIN show pseudostratification, with mild loss of polarity, hyperchromatic nucleus and absent/minimal mitosis. Stroma is typically devoid of inflammatory or reactive changes. In AIS dysplasia is more severe. The glands show crowding with numerous architectural patterns such as branching, intraluminal papillary pattern, micropapillary pattern and sometimes cribriform pattern of glands. The atypical cells have scant to moderate amount of mucin, markedly pleomorphic and hyperchromatic nuclei. Also, the degree of atypia and mitotic activity is greater than that seen in LCGIN [7]. The quantitative morphometrical analysis was done by using images captured of the representative area under Carl ZeissTM Primo StarTM microscope at X400 magnification for each case. At least 50 non-overlapping cells were analysed per case. The stromal cells or background cells were not included in the analysis. These cells were outlined using the ZEN 2.3 (blue edition) version 2.3.69.1000 @Carl Zeiss Microscopy GmbH, 2011 software. MNA, MNP, mND, MND were measured as shown in [Table/Fig-1,2]. These parameters were saved in the excel sheet and later were used to calculate the other three parameters namely,
Morphometrical analysis of cells using the ZEN 2.3 (blue edition) version 2.3.69.1000 @Carl Zeiss Microscopy GmbH, 2011 software.
Morphometric image of endocervical cells using the ZEN 2.3 (blue edition) version 2.3.69.1000 @Carl Zeiss Microscopy GmbH, 2011 software.
Mean nuclear Compactness (MNC)=MNP2/MNA
Mean Shape factor (MSHF)=4×π×MNA/MNP2
Mean Nuclear size (MNS)=2×(MNA/π)0.5 [8]
After obtaining the above parameters for each case, finally, the average value of each parameter was calculated for each histopathological category.
Statistical Analysis
All the captured data was coded and entered in Microsoft Excel sheet. Continuous variables were represented by mean±SD. The nuclear parameters between all the groups of ectocervix and endocervix were analysed using ANOVA and between the groups using a post-hoc test i.e. Bonferroni multiple comparison tests. Analysis was done by using SPSS software, version 22.0. The p-value <0.05 was considered as statistically significant.
Results
A total of 120 cases of cervical specimens were studied. These cases were then categorised into two main groups of ectocervix and endocervix. The ectocervix group was subcategorised into normal ectocervix (12), chronic cervicitis (12), LSIL (05), HSIL (08), squamous cell carcinoma (24). Similarly, the endocervix group was subcategorised into normal endocervix (26), chronic endocervicitis (13), LCGIN (20). Authors did not receive any case of AIS and adenocarcinoma during the period of study. [Table/Fig-3,4] show the nuclear parameters analysed in the different groups of both the ectocervical and endocervical cases. Using ANOVA for the ectocervical cases, all the nuclear parameters were statistically significant (p-value <0.05) except MSHF where the p-value was 0.415 whereas, in the endocervical cases, only mND and MSHF were statistically significant (p-value <0.05) [Table/Fig-3,4].
Nuclear parameters in different ectocervical lesions.
| Ectocervix | NEC | CE | LSIL | HSIL | SCC | ANOVA (F value) | p-value |
|---|
| (n=12) | (n=12) | (n=5) | (n=8) | (n=24) |
|---|
| Mean±SD | Mean±SD | Mean±SD | Mean±SD | Mean±SD |
|---|
| mND (μ) | 13.71±1.49 | 15.40±0.92 | 44.70±2.68 | 60.48±4.31 | 43.43±6.09 | 162.77 | <0.001 |
| MND (μ) | 24.55±1.21 | 27.76±1.61 | 64.91±2.91 | 72.43±7.78 | 76.42±8.66 | 146.512 | <0.001 |
| MNA (μ2) | 235.15±10.08 | 265.18±52.37 | 2098.51±428.03 | 3340.31±564.57 | 4317.19±889.62 | 37.3 | <0.001 |
| MNP (μ) | 60.09±2.06 | 67.77±4.75 | 161.44±16.92 | 207.62±10.91 | 289.65±19.89 | 196.20 | <0.001 |
| MNC | 15.35±1.28 | 17.31±1.50 | 12.42±0.05 | 12.91±3.07 | 17.56±6.10 | 3.108 | 0.022 |
| MSHF | 0.81±0.06 | 0.72±0.05 | 1.01±0.01 | 0.97±0.14 | 0.84±0.44 | 1.001 | 0.415 |
| MNS | 17.31±0.37 | 18.38±1.90 | 51.7±5.38 | 65.23±5.91 | 73.48±10.22 | 73.6 | <0.001 |
NEC: Normal ectocervix; CE: Chronic cervicitis; LSIL: Low grade squamous intraepithelial lesion; HSIL: High grade squamous intraepithelial lesion; SCC: Squamous cell carcinoma
Nuclear parameters in different endocervical lesions.
| Endocervix | NEN | PEC | LCGIN | ANOVA (F Value) | p-value |
|---|
| (n=26) | (n=13) | (n=20) |
|---|
| Mean±SD | Mean±SD | Mean±SD |
|---|
| mND (μ) | 53.11±1.55 | 54.03±1.50 | 47.70±3.64 | 12.16 | <0.001 |
| MND (μ) | 65.01±1.56 | 62.64±1.72 | 65.62±2.88 | 2.27 | 0.121 |
| MNA (μ2) | 2167.51±13.57 | 2162.83±41.03 | 1184.25±371.19 | 2.76 | 0.079 |
| MNP (μ) | 185.56±2.47 | 183.18±4.97 | 178.03±8.51 | 3.11 | 0.059 |
| MNC | 15.88±0.36 | 15.24±0.86 | 12.94±3.69 | 2.01 | 0.152 |
| MSHF | 0.79±0.01 | 0.82±0.04 | 0.97±0.12 | 9.30 | <0.001 |
| MNS | 52.55±0.16 | 52.94±0.49 | 55.86±4.67 | 2.13 | 0.136 |
NEN: Normal endocervix; PEC: Polypoidal endocervicitis; LCGIN: Low grade cervical glandular intraepithelial neoplasia
Discussion
Cervical cancer is one of the leading causes of cancer and cancer-related morbidity among women all over the world [1,2]. In Kolar, Karnataka, cervical cancer accounts for 17.55% of all cancer cases in the female population. In a developing country like India, most of these case present at an advanced stage [3]. The diagnosis of premalignant and malignant lesions of the cervix is predominantly dependent on the presence of abnormal cells. These abnormal cells are primarily identified and classified subjectively based on their characteristic nuclear features such as nuclear size, irregularity of nuclear border, nuclear pleomorphism, nuclear hyperchromatism and chromatin distribution [4]. There is a high degree of interobserver variability in the subcategorisation of high and low-grade lesions by subjective assessment. These discrepancies can be reduced by using objective visual evaluation by employing morphometrical analysis [5,6,9-12]. Thus, authors aimed at assessing the utility of nuclear morphometry through digital image analysis in converting these subjective parameters into an objective, quantitative, and reproducible parameters for the interpretation of endocervical and ectocervical pre-malignant and malignant lesions.
In the present study, authors have considered the nuclear parameters such as mND, MND, MNA, MNP, MNC, MSHF and MNS to differentiate between premalignant and malignant lesions in ectocervix and endocervix. The MSHF indicates nuclear shape irregularity [9]. Some of the studies which are done in breast and thyroid cases used these parameters for nuclear morphometry study and are published in English literature [8,13]. Among the mentioned parameters which were studied in the ectocervix group, all the nuclear parameters were statistically significant (p-value <0.05) except for MSHF where the p-value was 0.415 [Table/Fig-3]. Conversely, in the endocervix group only mND and mean shape factor MSHF were statistically significant (p-value <0.05) [Table/Fig-4]. However, due to the unavailability of cases in the endocervix group, a concrete opinion cannot be formed regarding the utility of morphometry in this group.
In a study done on cervical pap smears by Divya Rani MN et al., nuclear diameter and nuclear area were statistically significant (p-value <0.001) between premalignant and malignant squamous lesions of cervix [2]. In a similar study done by Po CH et al., using computer-based image analysis and Support Vector Machine, it showed that nuclear perimeter, nuclear area and nuclear diameter were statistically significant in dysplastic squamous cells [4]. Another study was done on cervix by Nemec E et al., using Feulgen stained tissue showed 97% specificity and 88% sensitivity in differentiating between normal and dysplastic squamous cells [14]. In this study, there was gradual increase in the nuclear parameters as the disease progressed from normal cervix to premalignant lesion to carcinoma in both the ectocervix and endocervix group with statistical significance [Table/Fig-3,4]. Similar findings were seen in the study done by Divya Rani MN et al., in Pap smears, however this study was done on tissue sections [2].
Many morphometry studies of other organs as breast and thyroid are published. In a morphometry study done on breast FNAC by Sabina L et al., parameters like nuclear diameter and nuclear area were statistically significant (p-value <0.001) between benign and malignant breast lesions [13,14]. Thus, in this study, nuclear diameter, nuclear perimeter, nuclear area, nuclear compactness and nuclear size were highly useful in differentiating premalignant lesions from carcinoma in the ectocervix group with a p-value of <0.05. Mean shape factor was not significant in doing the same with a p-value of >0.05 [Table/Fig-3]. However, in the endocervix group minimum nuclear diameter and nuclear shape factor was the significant parameters in differentiating between the normal endocervix, endocervicitis and LCGIN with a p-value of <0.05. All the other parameters were not statistically significant [Table/Fig-4].
Limitation
The limiting factors of this study were the unavailability of AIS and adenocarcinoma cases during the stipulated period. Thus, the nuclear morphometric parameters were not assessed in these two subgroups of endocervical lesions. However, the present study highlights the nuclear morphometric analysis in both ectocervical and endocervical tissue sections. The study was done on tissue sections which can overcome the fixation artefacts as in Pap smears. Doing this study in large population can help to derive the normal and abnormal values of different nuclear parameters in different grades of the ectocervical and endocervical lesions and can be used in cases with diagnostic ambiguity. The mean values derived in this study in different ectocervical and endocervical lesions can be applied for cytology smears.
Conclusion
Nuclear morphometry can be used as a tool in distinguishing the premalignant and malignant lesions in both ectocervix and endocervix. It can aid in solving cases with diagnostic ambiguity and offer appropriate quality treatment strategies. As this study was done on histopathology tissue sections, the nuclear morphometric mean values derived can be used as basic values in morphometric assessment of Pap smears.
NEC: Normal ectocervix; CE: Chronic cervicitis; LSIL: Low grade squamous intraepithelial lesion; HSIL: High grade squamous intraepithelial lesion; SCC: Squamous cell carcinoma
NEN: Normal endocervix; PEC: Polypoidal endocervicitis; LCGIN: Low grade cervical glandular intraepithelial neoplasia