Medical Therapy, A Better Alternative to Micro Lymphatic-Venous Anastomosis in Advanced Lymphoedema of the Leg: Review of Some Cases
Dwijesh Kumar Panda1
1 Lymphologist and Pathologist, Department of Pathology and Medicine, Sanaria Filaria Clinic and Research Centre, Bhubaneswar, Odisha, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Dwijesh Kumar Panda, M5/12, Acharya Vihar, Bhubaneswar-751013, Odisha, India.
E-mail: doctordwijesh@gmail.com
Advanced lymphoedema of leg is frequently encountered in clinical practice. Chronic inflammation and fibrosis are the histological hallmarks of lymphoedema. This article presents three case reports. Two patients were suffering from advanced lymphoedema who underwent micro lymphatic-venous anastomosis. And the third patient suffering from advanced lymphoedema was treated with medical therapy. Surgery was a failure whereas medicine treatment helped the patients to lead a normal life.
Bridging techniques, Lymphoscintigraphy, Surgery
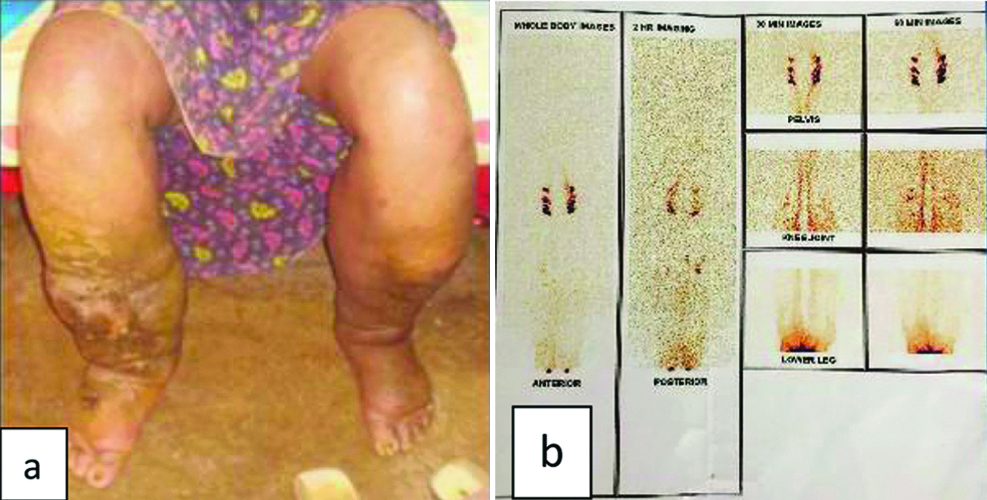
Case 1
A male aged about 45-year-old suffered from elephantiasis of both legs for a period of more than 10 years [Table/Fig-1]. It was diagnosed to be stage IV lymphoedema. The lymphoscintigraphy report suggested dermal back flow along with non-visualisation iliacal and paraaortic lymph nodes. The quantitative monoclonal antibody-based ELISA test (OG4C3) for detection of circulating filarial antigen became highly positive. He was operated for micro lymphatic-venous (end-to-end) anastomosis (MLVA) followed by pneumatic compression and elastic compression garments. There was 30% to 40% reduction of oedema for a period of three months. Subsequently the size of the leg reversed. The signs and symptoms recurred along with cellulitis. Ulcer and discharge of pus from the ankle and lower part of leg continued. The patient was confined to house and ultimately lost his job. The later period of life became precarious.
(a) Clinical picture demonstrating chronic ulcer, discharge of pus from bilateral lower limbs after MLVA surgery; (b) Lymphoscintigraphy of the limbs showing lymphatic obstruction.
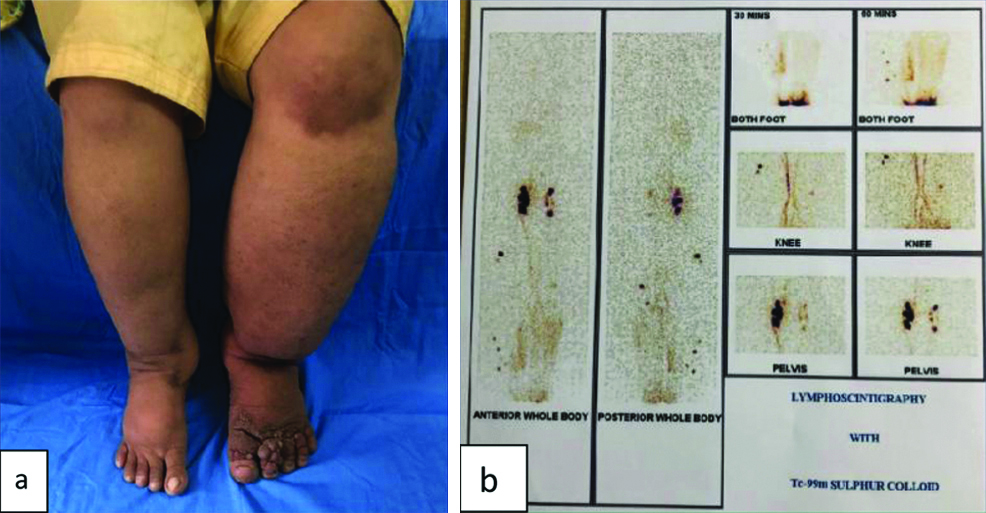
Case 2
A female aged about 31-year-old suffered from bilateral elephantiasis of leg [Table/Fig-2]. The right leg was grade III and the left leg grade IV with nodules on the toes and candida infection in between. The lymphoscintigraphy report showed severe impairment of lymphatic flow on both sides with dilated lymphatic channels and persistent popliteal lymph nodes on both sides. There was non-visualisation of iliacal and paraaortic lymph nodes as well as activity in the liver suggesting stagnation of lymphatic flow from both extremities. The quantitative monoclonal antibody-based ELISA test (OG4C3) for detection of circulating antigens was found positive in moderately high titre. The patient was operated for MLVA followed by pneumatic compression. The size of the leg reduced 40% for a period of four months. Subsequently, it bounced back.
(a) Clinical picture of bilateral elephantiasis of leg after MLVA surgery; (b) Lymphoscintigraphy shows severe impairment of lymphatic flow on both sides.
Case 3
A male aged about 21-year-old developed bilateral elephantiasis of leg [Table/Fig-3]. The diagnosis was confirmed by lymphoscintigraphy. Severe impairment of lymphatic flow on both sides with dilated lymphatic channels and persistent popliteal lymph nodes on both sides was seen. There was non-visualisation of iliacal and paraaotic lymph nodes as well as activity in the liver suggesting stagnation of lymphatic flow from both extremities. The circulating monoclonal filarial antigen (OG4C3) test found positive in very high titre. He was treated successfully with medical therapy alone. He was on Benzathine Penicillin 12 lacs intramuscularly every 15 days after sensitivity test to avoid infection along with application of compression stocking to improve limb volume. Benzathine penicillin proved to be very effective in the prevention of recurrent infections. Studies have shown that between 80-90% of patients reporting a penicillin allergy do not in fact have true hypersensitivity reactions and the vast majority of these patients can tolerate beta-lactams.
(a) Clinical picture demonstrating elephantiasis of leg with medicine treatment alone; (b) Lymphoscintigraphy of the both legs showing impairment of lymphatic flow with dilated lymphatic channels.
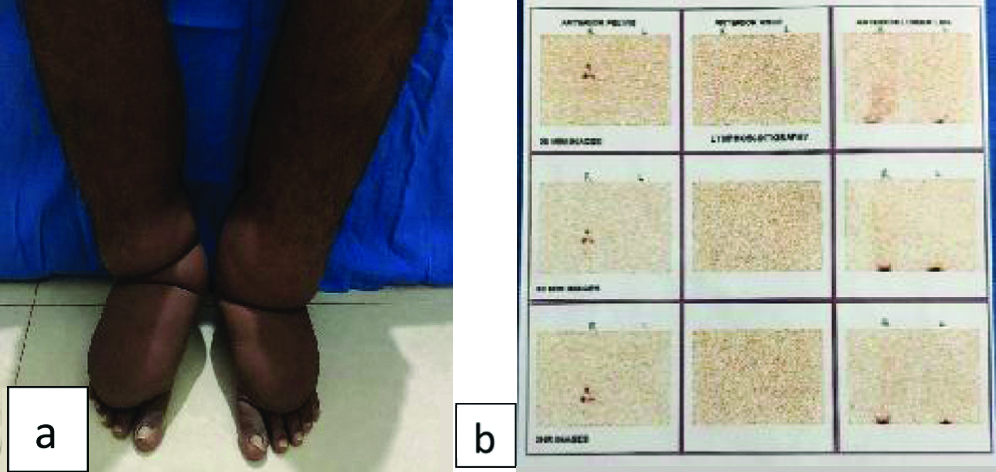
The patient was instructed to take care of the foot and toe spaces to avoid recurrent fungal and bacterial infection. Elastic compression stocking enhanced lymphatic contractility and redirect flow into the non-obstructed lymphatics. There was no recurrence of dermato-adenolymphangitis after six months of treatment.
Discussion
Lymphoedema is the second leading cause of permanent disfiguring, debilitating, and disability in the world [1]. The permanent cure is not possible as the body is unable to regrow new lymphatics. Each episode of infection is followed by breakdown of the skin immune barriers which worsens in advanced lymphoedema [2]. Recurrent attacks of Adeno-Dermato-Lymphangitis (ADL) leads tolymphoedema. Surgery reduces the weight of the lymphoedematous region, minimise the frequency of infections/inflammatory episodes, and/or improve cosmesis and function. Other categories of surgical treatment include: (1) excisional operations (e.g., debulking, amputation, and liposuction); (2) lymphatic reconstruction; (3) tissue transfer procedures. Lymphatic reconstruction and tissue transfer procedures can be done in earlier stages of elephantiasis, and for later stages debulking procedures and split skin grafting are done. The complications of debulking surgery range from breakdown of the skin graft, chronically non-healing oozing wound and repeated skin infections and in worst case, sepsis [3,4]. The bridging technique allows drainage of the superficial lymphatics through the deep system by excision of strips of fascia. The fascial barrier reform and the operation become ineffective. Lymphatic anastomosis is done to relieve obstructive lymphoedema. Lymphatic-venous shunts although encouraging in early stages, are found disappointing later on.
Management of lymphoedema is a continuing challenge to patients and clinicians. Early diagnosis by monoclonal circulating adult filarial antigen test (OG4C3) [5] and lymphoscintigraphy [6] improved accuracy of diagnosis and effective medical treatment. Inflammation and infection of the leg, interdigital skin lesions of the foot associated with Streptococcus pyogenes, noticed in 50% of cases. Each episode of infection leads to advanced stages of deep lymphoedema. Severe infections require hospitalisation and intensive antibiotic therapy [7,8]. Advanced lymphoedema leads to grotesque deformity. Massive chronic swellings are unfortunately irreversible and lymphatic microsurgery continues to remain an unfulfilled promise [9].
Conclusion
In the indexed cases, medical therapy was aimed to avoid repeated bacterial and fungal infection. The surgical intervention was done to anastomose venous and lymphatic vessels. This proved to be unsuccessful as the lymphatic ducts were not patent distal to the obstruction.
[1]. World Health Organization, the Regional Strategic Plan for Elimination of Lymphatic Filariasis (2010-2015): Expert Committee on Filariasis, Geneva. WHO Technical Services [Google Scholar]
[2]. Panda DK, Mohapatra DP, Mohapatra MM, Breastfilariasis or inflammatory breast carcinoma? Reaching a diagnosisBMJ Case Rep 2015 2015:pii:bcr2015212254doi: 10.1136/bcr-2015-21225410.1136/bcr-2015-21225426567240 [Google Scholar] [CrossRef] [PubMed]
[3]. Cormier JN, Rourke L, Crosby M, Chang D, Armer J, The surgical treatment of lymphoedema: a systematic review of the contemporary literature (2004-2010)Ann SurgOncol 2012 19:642-51.10.1245/s10434-011-2017-410.1245/s10434-011-2017-421863361 [Google Scholar] [CrossRef] [PubMed] [CrossRef] [PubMed]
[4]. Panda DK, Mohapatra DP, Mohapatra M, The Complications of Surgical Treatment of Grade IV Filarial Lower Limb LymphedemaAustin J Trauma Treat 2016 3(1):1008 [Google Scholar]
[5]. Lalitha P, Ravichandran M, Suba S, Kaliraj P, Narayanan RB, Jayaraman K, Quantitative assessment of circulating antigens in human lymphatic filariasis: a field evaluation of monoclonal antibody-based ELISA using blood collected on filter stripsTrop Med Int Health 1998 3(1):41-45.10.1046/j.1365-3156.1998.00170.x9484967 [Google Scholar] [CrossRef] [PubMed]
[6]. Narushima M, Yamamoto T, Ogata F, Yoshimatsu H, Mihara M, Koshima I, Indocyaninegreen lymphography findings in limb lymphoedemaJ ReconstrMicrosurg 2016 32(01):072-079.10.1055/s-0035-156460826422172 [Google Scholar] [CrossRef] [PubMed]
[7]. International Society of LymphologyThe diagnosis and treatment of peripheral lymphoedema: 2013 Consensus Document of the International Society of LymphologyLymphology 2013 46:1 [Google Scholar]
[8]. Dreyer G, Addiss D, Gadelha P, Lapa E, Williamson J, Dreyer A, Interdigital skin lesions of the lower limbs among patients with lymphoedema in an area endemic for bancroftianfilariasisTrop Med Int Health 2006 11(9):1475-81.10.1111/j.1365-3156.2006.01687.x16930270 [Google Scholar] [CrossRef] [PubMed]
[9]. Panda DK, Mohapatra DP, Dermato-lymphangitis infilariasis resembles infected chronic venous insufficiency:Two Case Reports and Review of LiteratureJ ClinDiag Res 2018 12(9):PE01-PE04.10.7860/JCDR/2018/37460.12046 [Google Scholar] [CrossRef]