Comparison of Propofol Alone and Propofol-Ketamine Mixture for Sedation during Endoscopic Retrograde Cholangiopancreatography (ERCP): A Randomised Study
Aditya Garg1, Mukesh Kumar Prasad2, Gurdeep Singh Jheetay3, Rohit Kumar Varshney4, Amit Kumar Choudhary5, Himani Saroha Garg6
1 Postgraduate Resident, Department of Anaesthesia, Teerthankar Mahaveer Medical College and Research Centre, Moradabad, Uttar Pradesh, India.
2 Associate Professor, Department of Anaesthesia, Teerthankar Mahaveer Medical College and Research Centre, Moradabad, Uttar Pradesh, India.
3 Professor and Head, Department of Anaesthesia, Teerthankar Mahaveer Medical College and Research Centre, Moradabad, Uttar Pradesh, India.
4 Associate Professor, Department of Anaesthesia, Teerthankar Mahaveer Medical College and Research Centre, Moradabad, Uttar Pradesh, India.
5 Assistant Professor, Department of Anaesthesia, Teerthankar Mahaveer Medical College and Research Centre, Moradabad, Uttar Pradesh, India.
6 Assistant Professor, Department of Paediatrics, Teerthankar Mahaveer Medical College and Research Centre, Moradabad, Uttar Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Mukesh Kumar Prasad, Associate Professor, Department of Anaesthesia, Teerthankar Mahaveer Medical College and Research Centre, Teerthanker Mahaveer University, Moradabad-244001, Uttar Pradesh, India.
E-mail: mukeshkumar2002@gmail.com
Introduction
Propofol is frequently used for deep sedation for Endoscopic Retrograde Cholangiopancreatography (ERCP). Sedation-Related Adverse Events (SRAEs), associated with propofol administration, include hypotension, arrhythmia, oxygen desaturation, unplanned intubation and procedure termination whereas, ketamine propofol combination has favourable haemodynamic effects.
Aim
To evaluate the efficacy of the synergistic effect of small dose of ketamine (25 mg) and propofol in comparison with propofol alone on propofol consumption for deep sedation in patients undergoing ERCP.
Materials and Methods
A total of 60 patients undergoing ERCP were randomly assigned to one of the two medication regimens through chit and box method. Patients in Group 1 (n=30) received only intravenous propofol, while patients in Group 2 (n=30) received 25 mg of i.v. ketamine along with intravenous propofol and both groups of patients were titrated to achieve deep sedation. Total propofol consumption was recorded in both groups.
Results
Patients in both groups were comparable in terms of BMI, ASA status and duration of ERCP. Group 1 patients required significantly higher doses of propofol (370±123.4 mg) as compared with Group 2 (342.65±116.4 mg). The mean percentage decline in oxygen saturation during the procedure was greater in Group 1 than it was in Group 2.
Conclusion
Authors concluded that during ERCP addition of ketamine to propofol resulted in decrease in propofol consumption without disturbing intra and post-procedure haemodynamic stability.
Consumption, Endoscopic retrograde, Ramsay sedation
Introduction
Endoscopic Retrograde Cholangiopancreatography (ERCP) is the most common management for pancreatobiliary disorders. ERCP is the ideal method for removal of common bile duct stones and has reduced the requirement of invasive surgical procedures which are associated with high morbidity mainly in old age patients. ERCP with stent placement is an effective methodology for palliative care in obstructive jaundice in patients with pancreatic cancer [1,2].
Endoscopic Retrograde Cholangiopancreatography (ERCP) is time taking and complex procedure, with a substantially higher complication rate in comparison with upper Gastrointestinal endoscopic procedures [3]. Most of the complications in ERCP are related to sedation which includes cardiopulmonary events such as hypoxemia, apnoea, arrhythmia, hypotension, hypoventilation, airway obstruction and vasovagal episodes [4,5].
Propofol is commonly used in GI endoscopic procedures due to its rapid onset of action and fast recovery time but unfortunately, it could cause possible cardiovascular and respiratory depression in a dose-dependent manner [6]. It is a γ-aminobutyric acid facilitator in the central nervous system. It might be inadequate to comfort patients in painful processes since it lacks analgesic properties. Ketamine acts on N-methyl-D-aspartate receptors and produces dissociative anaesthesia and provides sedation, analgesia and amnesia. Although it is recognised as an effective and reliable anaesthetic agent, cardiotoxicity and induction of transitory psychotic episodes, together with delayed recovery and secretions are the main drawbacks for ketamine use although authors have not assessed this aspect in this study [7-9].
To eliminate untoward effects of both anaesthetic agents, the combination of both is tried for sedation. Ketamine mitigates propofol-induced hypotension, and propofol mitigates ketamine-induced vomiting and recovery agitation [10]. The drugs display synergic and smoother sedation, and the combination has the theoretical evidence of decreasing the propofol dosage [11]. Authors hypothesised that propofol-ketamine combination would have favourable effects on haemodynamic parameters and recovery times compared to propofol alone with negligible side-effect in patients undergoing ERCP. The primary objective of this study was to evaluate the efficacy of synergistic effect of small dose of ketamine (25 mg) and propofol in comparison with propofol alone on propofol consumption for deep sedation in patients undergoing ERCP. The secondary objectives were to compare the two groups with regard to gastroenterologist’s satisfaction, the recovery time, and the adverse events related to sedation.
Materials and Methods
After taking approval of Institutional Ethical Committee (certificate reference no: TMMS/IEC/2017/21), this randomised controlled study was conducted in Teerthakar Mahavir Medical College and Hospital, Moradabad, Uttar Pradesh, India. Patients of ASA Grade I and II aged between 18-65 years with their due written consent, undergoing ERCP were included in study. The duration of study was between August 2017 and April 2018. ERCP was done by same gastroenterologist who was blinded to both groups. The sample size was based on data of previous studies [12,13] which indicated that a total sample size of 60 patients (after exclusion of the drop out) randomly allocated into two equal groups (30 patients in each group) is sufficient to ensure power 80%.
Exclusion criteria included pregnancy, opioid or any substance abuse history, patients having anticipated difficult airway or history of obstructive sleep apnea, allergic to propofol or eggs.
Electrocardiogram, pulse oximetry, and noninvasive blood pressure were monitored, and oxygen at 4 L/minute was supplemented using nasal prongs. All patients were given intravenous Glycopyrrolate 0.2 mg and intravenous Ondansetron @0.15 mg/kg as premedication. As per the institution protocol, all patients received one gram I.V Paracetamol at the time of induction. Study medication was prepared and given by fellow anaesthesiologist who is not involved in any other part of study.
Patients were randomised into 2 groups of 30 each by chit and box method. Group 1 received 1 mL normal saline+Propofol and Group 2 received Injection ketamine (25 mg i.v stat) + Propofol.
Both groups of patients received 20 mg propofol in bolus. Sedation was maintained at Ramsay sedation score >4 with infusion of propofol at 50 mcg/kg/hour which was titrated to 150 mcg/kg/hour as per requirements [Table/Fig-1] [14]. Sedation was checked by response to verbal command and light glabellar tap every five minutes. The primary objective was to determine total dose of propofol, incidence of hypotension (fall in BP >20% of baseline), incidence of fall in oxygen saturation (<90%), incidence of nausea or vomiting and any other adverse event.
Ramsay sedation score [14].
| Sedation score | Clinical response |
|---|
| 0 | Paralyzed, unable to evaluate |
| 1 | Awake |
| 2 | Light sedated |
| 3 | Moderately sedated, follows simple command |
| 4 | Deeply sedated, responds to non painful stimuli |
| 5 | Deeply sedated, responds only to painful stimuli |
| 6 | Deeply sedated, unresponsive to painful stimuli |
The gastroenterologist was asked to rate operator feasibility on subjective assessment as poor, average, or good. Gastroenterologist’s satisfaction was subjective, for quality of sedation based on a previous study [15].
Statistical Analysis
Qualitative data were expressed as frequency and percentage. Chi-square test (Fisher’s-exact test) was used to examine the relationship between qualitative variables. For quantitative data, comparison between two groups was done using independent sample t-test or Mann-Whitney test. Comparison of repeated measures was done using ANOVA test for repeated measures. A p-value <0.05 was considered significant. Data were entered into MS-Excel spreadsheet and analysis was performed using Statistical Package for the Social Sciences for Windows version 23.0 (IBM Corp, Armonk, NY, USA).
Results
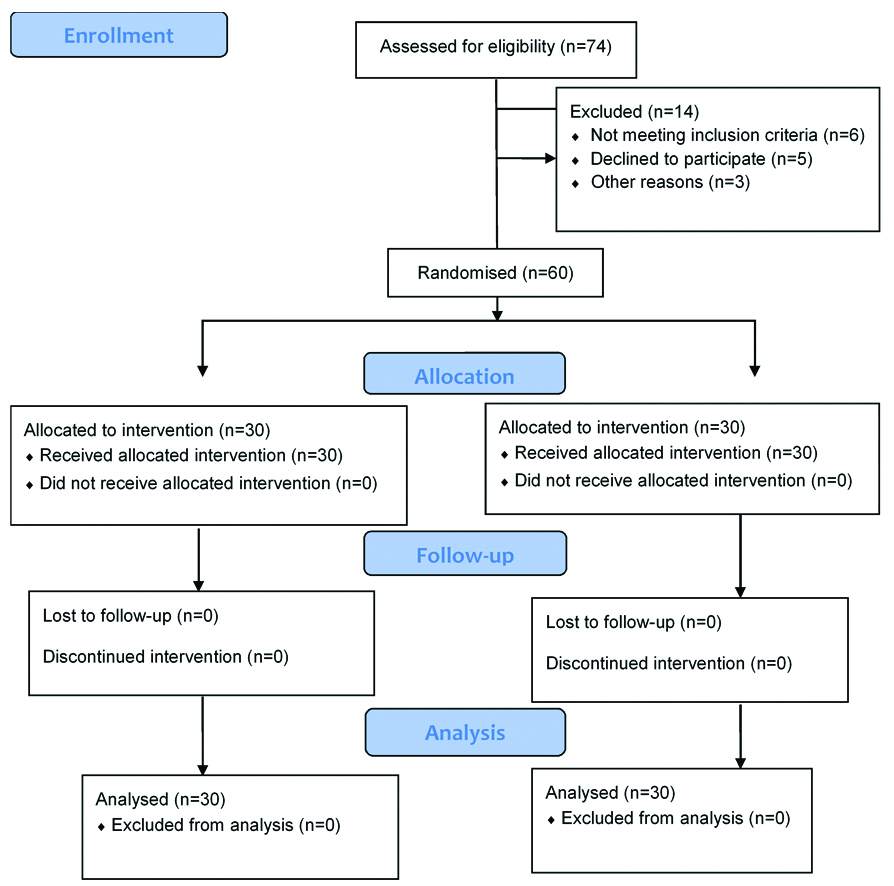
Patient selection and follow-up methodology is shown in consort diagram [Table/Fig-2].
Consort flow diagram of present study.
Baseline characteristics (age, sex, weight and duration of procedure) were observed to be statistically insignificant between the groups in [Table/Fig-3]. This shows that patients demographics and duration of procedure did not effect propofol dosage overall.
Patient demographics and procedure times.
| Variables | Propofol (N=30) Group 1 | Propofol/Ketamine (N=30) Group 2 | p-value |
|---|
| Age (years) | 42.7±8 | 39±10.7 | 0.135 |
| Weight (in kg) | 60.7 ±8.5 | 61.8±9.7 | 0.642 |
| Sex (male/female) | 21/9 | 17/13 | 0.211 |
| Duration of the procedure (minutes) | 48.3±8.2 | 46.5±7.5 | 0.379 |
The total dose of propofol consumption was significantly low in synergy with ketamine as compared to propofol only sedation. Clinical characteristics like sedation related adverse events hypoxia and hypotension were comparable during the procedure [Table/Fig-4].
Clinical characteristics.
| Variables | Propofol (N=30) Group 1 | Propofol/Ketamine (N=30) Group 2 | p-value |
|---|
| Total dose of propofol | 370 (±123.4) | 342.65 (±116.4) | 0.004* |
| Hypotension | 7 | 2 | 0.08 |
| Hypoxia | 7 | 2 | 0.08 |
| Post procedure nausea | 5 | 3 | 0.35 |
*p<0.05
The [Table/Fig-5] reveals gastroenterologists feasibility between both the groups. The gastroenterologists’ satisfaction score was comparable in both the groups. All the patients were discharged from recovery room after two hours of observation. No patient had any recall or memory after the procedure.
Gastroenterologists feasibility.
| Propofol (N=30) Group 1 | Propofol/Ketamine (N=30) Group 2 | |
|---|
| Good | 22 | 26 | 0.31 |
| Average | 8 | 4 | 0.22 |
| Poor | 0 | 0 | - |
Discussion
From the study, it is observed that there is significant reduction in total dosage of propofol in combination with ketamine than giving propofol alone for comparable procedure time. Ketamine and propofol have been studied extensively individually or in conjunction with other sedatives/analgesics. Ketamine has demonstrated a wide margin of safety, with slight risk of serious adverse-effects [16,17], whereas propofol although shown safe for faster induction of sedation but also has higher incidence of hypoxia and hypotension.
The opposing haemodynamic and respiratory effects of ketamine and propofol suggest the potential for synergy. The combination has been used outside the Emergency Department for sedation, with positive results [18]. Specifically, Frey K et al., and Akin A et al., found that there may be reduced rates of respiratory depression and increased quality of sedation when a combination of ketamine/propofol was compared against propofol alone and fentanyl/propofol, respectively [19,20]. These findings were in accordance with the present study. Hwang J et al., in study evaluating patient controlled sedation observed a reduced systolic blood pressure during fiberoptic bronchoscopy in patients undergoing sedation with alfentanil/propofol compared with those receiving a ketamine/propofol combination as in the present study, patients were more haemodynamic stable in ketamine propofol group [21].
Mourad M et al., showed that when low-dose ketamine was used in conjunction with propofol for procedural sedation and analgesia, a significant reduction in the amount of propofol required for sedation was observed [22]. The mechanism of this effect is not clear. It has been stated that ketamine in less than dissociative doses does not have anaesthetic effects but rather has analgesic effects [23]. Ketamine act synergistically by either potentiating the sedative activity of propofol or producing enough analgesia to allow a lower dose of propofol to produce the desired sedation level.
Aydogan H et al., in the study done in upper GI endoscopy procedure found that ketamine-propofol group consumed 72±12 mg of propofol while propofol group alone consumed 92±10 mg; much lower in ketamine+propofol similarly as in the present study [24]. Here total propofol consumption is lower in both groups as upper GI endoscopy procedure was less time-consuming.
Propofol consumption in a study performed by Saric PJ et al., was (352.65±109.44 mg) in ketamine-propofol group versus (380±135.4 mg) in propofol alone for deep sedation during ERCP in elderly, p-value was 0.0268 while the present study also shows significant reduction in propofol with p-value being 0.004 [25].
Limitation
The potential limitations were inability to assess intraoperative depth of anaesthesia and incidence of intraoperative awareness as the BIS monitor was unavailable, however the intensity of noxious stimuli that the patients received during procedure might be relatively homogeneous because of the same intervention. Therefore, authors believe that there may have been only a small difference in anaesthetic depth between the groups during the study period. Finally, the cost effectiveness was not evaluated in the current study.
Conclusion
Authors conclude that addition of ketamine to propofol results in decrease in propofol consumption during Endoscopic Retrograde Cholangiopancreatography (ERCP) procedures. Better haemodynamic stability in propofol+ketamine group makes it more convincing in patients with compromised status. Moreover, propofol ketamine mixture maintains better oxygen saturation levels in patients undergoing ERCP.
*p<0.05
[1]. Fanti L, Testoni PA, Sedation and analgesia in gastrointestinal endoscopy: what is new?World J Gastroenterol 2010 16(20):2451-57.10.3748/wjg.v16.i20.245120503443 [Google Scholar] [CrossRef] [PubMed]
[2]. Adler DG, Baron TH, Davila RE, Egan J, Hirota WK, Leighton JA, Standards of Practice Committee of American Society for Gastrointestinal endoscopy. ASGE guidelines: the role of ERCP in diseases of the biliary tract and the pancreasGastrointest Endosc 2005 62(1):1-8.10.1016/j.gie.2005.04.01515990812 [Google Scholar] [CrossRef] [PubMed]
[3]. Standards of Practice Committee of the American Sociecty for Gastrointestinal EndoscopyLichtenstein DR, Jagannath S, Baron TH, Anderson MA, Banerjee S, Sedation and anaesthesia in GI endoscopyGastrointest Endosc 2008 68(5):815-26.10.1016/j.gie.2008.09.02918984096 [Google Scholar] [CrossRef] [PubMed]
[4]. Chainaki IG, Manolaraki MM, Paspatis GA, Deep sedation for endoscopic retrograde cholangiopancreatographyWorld J Gastrointest Endosc 2011 3(2):34-39.10.4253/wjge.v3.i2.3421403815 [Google Scholar] [CrossRef] [PubMed]
[5]. Beeton A, Refresher course; Quoted ERCP: sedation or anaesthesia?South Afr J Anaesth Analg 2011 17(1):124-25.10.1080/22201173.2011.10872755 [Google Scholar] [CrossRef]
[6]. Rex DK, Overley CA, Walker J, Registered nurse administered propofol sedation for upper endoscopy and colonoscopy: Why? When? How?Rev Gastroenterol Disord 2003 3(2):70-80. [Google Scholar]
[7]. Okamoto N, Nakai T, Sakamoto K, Nagafusa Y, Higuchi T, Nishikawa T, Rapid antidepressant effect of ketamine anaesthesia during electroconvulsive therapy of treatment-resistant depression: comparing ketamineand propofol anaesthesiaJ ECT 2010 26(3):223-27.10.1097/YCT.0b013e3181c3b0aa19935085 [Google Scholar] [CrossRef] [PubMed]
[8]. Rasmussen KG, Jarvis MR, Zorumski CF, Ketamine anaesthesia in electroconvulsive therapyConvuls Ther 1996 12(4):217-23. [Google Scholar]
[9]. Yan JW, McLeod SL, Iansavitchene A, Ketamine-propofol versus propofol alone for procedural sedation in the emergency department: a systematic review and meta-analysisAcad Emerg Med 2015 22(9):1003-13.1993508526292077 [Google Scholar] [CrossRef] [PubMed]
[10]. Song JW, Shim JK, Song Y, Yang SY, Park SJ, Kwak YL, Effect of ketamine as an adjunct to intravenous patient-controlled analgesia, in patients at high risk of postoperative nausea and vomiting undergoing lumbar spinal surgeryBr J Anaesth 2013 111(4):630-35.10.1093/bja/aet19223744819 [Google Scholar] [CrossRef] [PubMed]
[11]. Paspatis GA, Manolaraki MM, Vardas E, Theodoropoulou A, Chlouverakis G, Deep sedation for endoscopic retrograde cholangiopancreatography: intravenous propofol alone versus intravenous propofol with oral midazolam premedicationEndoscopy 2008 40(4):308-13.10.1055/s-2007-99534618058653 [Google Scholar] [CrossRef] [PubMed]
[12]. Elzohry AAM, Ali AAM, Shehata MR, Ketamine versus Dexmedetomidine as Adjunct Agent to Propofol for Sedation during Endoscopic Retrograde Cholangiopancreatography (ERCP)Integr Anaesthesiol 2018 1(1):01-07. [Google Scholar]
[13]. Sethi P, Mohammed S, Bhatia PK, Gupta N, Dexmedetomidine versus midazolam for conscious sedation in endoscopic retrograde cholangiopancreatography: An open-label randomised controlled trialIndian J Anaesth 2014 58(1):18-24.10.4103/0019-5049.12678224700894 [Google Scholar] [CrossRef] [PubMed]
[14]. Ramsay MAE, Savege TM, Simpson BRJ, Goodwin R, Controlled sedation with alphaxalone-alphadoloneBr Med J 1974 2(5920):656-59.10.1136/bmj.2.5920.6564835444 [Google Scholar] [CrossRef] [PubMed]
[15]. Singh SA, Prakash K, Sharma S, Dhakate G, Bhatia V, Comparison of propofol alone and in combination with ketamine or fentanyl for sedation in endoscopic ultrasonographyKorean J Anaesthesiol 2018 71(1):43-47.10.4097/kjae.2018.71.1.4329441174 [Google Scholar] [CrossRef] [PubMed]
[16]. Zed PJ, Abu-Laban RB, Chan W, Harrison DW, Efficacy, safety and patient satisfaction of propofol for procedural sedation and analgesia in the emergency department: a prospective studyCJEM 2007 9(6):421-27.10.1017/S148180350001544X18072987 [Google Scholar] [CrossRef] [PubMed]
[17]. Bassett KE, Anderson JL, Pribble CG, Guenther E, Propofol for procedural sedation in children in the emergency departmentAnn Emerg Med 2003 42(6):773-82.10.1016/S0196-0644(03)00619-X [Google Scholar] [CrossRef]
[18]. Burton JH, Miner JR, Shipley ER, Strout TD, Becker C, Thode HC Jr, Propofol for emergency department procedural sedation and analgesia: a tale of three centersAcad Emerg Med 2006 13(1):24-30.10.1197/j.aem.2005.08.01116365337 [Google Scholar] [CrossRef] [PubMed]
[19]. Frey K, Sukhani R, Pawlowski J, Pappas AL, Mikat-Stevens M, Slogoff S, Propofol versus propofol ketamine sedation for retrobulbar nerve block: comparison of sedation quality, intraocular pressure changes, and recovery profilesAnaesth Analg 1999 89(2):317-21.10.1097/00000539-199908000-0001310439740 [Google Scholar] [CrossRef] [PubMed]
[20]. Akin A, Esmaoglu A, Tosun Z, Gulcu N, Aydogan H, Boyaci A, Comparison of propofol with propofol-ketamine combination in pediatric patients undergoing auditory brainstem response testingInt J Pediatr Otorhinolaryngol 2005 69(11):1541-45.10.1016/j.ijporl.2005.04.01115936092 [Google Scholar] [CrossRef] [PubMed]
[21]. Hwang J, Jeon Y, Park HP, Lim YJ, Oh YS, Comparison of alfentanil and ketamine in combination with propofol for patient-controlled sedation during fiberoptic bronchoscopyActa Anaesth Scand 2005 49(9):1334-38.10.1111/j.1399-6576.2005.00842.x16146472 [Google Scholar] [CrossRef] [PubMed]
[22]. Mourad M, El-Hamamsy M, Anwar M, Schwarz E, Low dose ketamine reduces sedative doses of propofol during ambulatory transoesophageal echocardiographyEgypt J Anaesth 2004 20(1):41-46. [Google Scholar]
[23]. Green SM, Research advances in procedural sedation and analgesiaAnn Emerg Med 2007 49(1):31-36.10.1016/j.annemergmed.2006.09.02017083997 [Google Scholar] [CrossRef] [PubMed]
[24]. Aydogan H, Aydgoan T, Uyankoglu A, Kucuk A, Yuce HH, Alpkarahan M, Propofol–ketamine combination has shorter recovery times with similar haemodynamics compared to propofol alone in upper gastrointestinal endoscopy in adults: a randomized trialActa Medica Mediterranea 2013 29:259-64. [Google Scholar]
[25]. Saric PJ, Matasic H, Zenko J, Ivanov N, Comparison of propofol and ketamine for deep sedation during ERCP in elderly 2AP1-2Eur J Anaesthesiol 2012 29:3110.1097/00003643-201206001-00101 [Google Scholar] [CrossRef]